Paratubal or Paraovarian Cysts
Synonyms/Description
Etiology
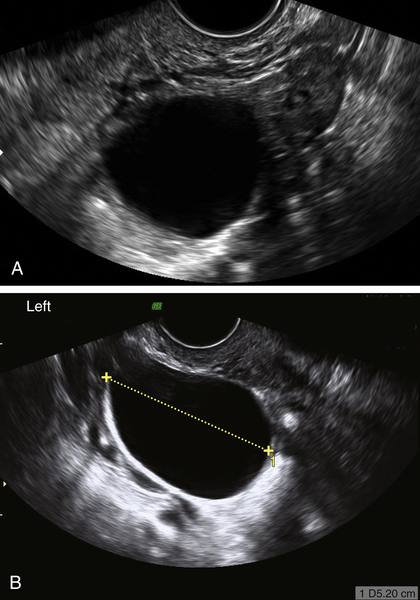
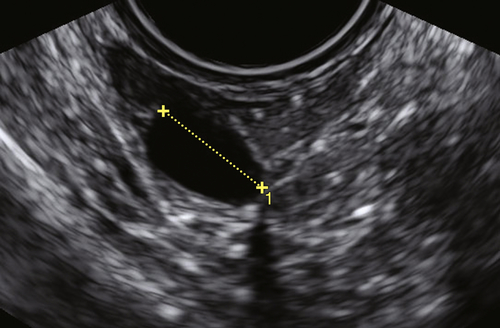
Ultrasound Findings
Differential Diagnosis
Clinical Aspects and Recommendations
Suggested Reading
Barloon T.J., Brown B.P., Abu-Yousef M.M., Warnock N.G. Paraovarian and paratubal cysts: preoperative diagnosis using transabdominal and transvaginal sonography. J Clin Ultrasound. 1996;24:117–122.
Kim J.S., Woo S.K., Suh S.J., Morettin L.B. Sonographic diagnosis of paraovarian cysts: value of detecting a separate ipsilateral ovary. Am J Roentgenol. 1995;164:1441–1444.
Kiseli M., Caglar G.S., Cengiz S.D., Karadag D., Yilmaz M.B. Clinical diagnosis and complications of paratubal cysts: review of the literature and report of uncommon presentations. Arch Gynecol Obstet. 2012;285:1563–1569.
Stein A.L., Koonings P.P., Schlaerth J.B., Grimes D.A., d’Ablaing 3rd. G. Relative frequency of malignant parovarian tumors: should parovarian tumors be aspirated? Obstet Gynecol. 1990;75:1029–1031.
Terek M.C., Sahin C., Yeniel A.O., Ergenoglu M., Zekioglu O. Paratubal borderline tumor diagnosed in the adolescent period: a case report and review of the literature. J Pediatr Adolesc Gynecol. 2011;24:e115–e116.