Advances in Anesthesia, Vol. 28, No. 1, 2010
ISSN: 0737-6146
doi: 10.1016/j.aan.2010.08.002
Single or Multiple Guidance Methods for Peripheral Nerve Blockade in Modern-Day Practice of Regional Anesthesia
Regional anesthesia has traditionally been performed with the help of a single modality, which has depended on the availability of technology at the time of performance of these blocks. The transitions from paresthesia-guided to nerve stimulation to ultrasound-guided nerve blocks have helped advance regional anesthesia as a science rather than an art, and have taken it to a higher level of sophistication. However, the visual information obtained with the use of ultrasonography remains subject to interpretation by the user and, consequently, is limited by the ability to optimize the sonographic image, variations in formal training of applied ultrasound physics, and overall experience in ultrasonography. Even though ultrasound visualization by itself is presumably associated with minimal risks, the safety claimed by ultrasound enthusiasts may not necessarily result in the safest clinical practice.
There is current debate as to whether the use of nerve stimulation or ultrasonography is superior as a nerve localization instrument for regional anesthesia; there is also a proposal that the use of dual or multiple guidance modalities may further expand the opportunities to employ regional anesthesia versus use of a single method. Regional anesthesia reliably works if the correct amount of the correct local anesthetic is placed within the correct fascial plane in correct proximity to the nerve. Nerve stimulation is generally able to provide one or two of these objectively, that is, depositing a local anesthetic near the nerve to be blocked. Anesthesiologists traditionally have used larger doses of local anesthetics with this technique to ascertain block success, as it is not possible to stimulate the nerve again after even a small dose of local anesthetic has been deposited. Ultrasonography does not solve all of these problems but it does provide extra information, such as direct visualization of nerve structures that need to be blocked, the appropriate spread of the local anesthetic around the nerve and within the correct fascial plane, and visualization of the surrounding perineural structures that need to be avoided. These advantages may improve success and reduce complications; however, experts have suggested that such claims may be premature [1]. The success rate and expertise of practitioner groups varies, making it very difficult to compare the results of studies from different institutions and operators. Use of one approach should not preclude the use of another, and the debate on the best methods needs to be more outcome-oriented than target-oriented. The guidance modalities used in each case must depend on the availability of equipment, the hospital setting, the individual patient’s needs, and the expertise of the practitioner. Current technologies aiding in block performance include feeling loss of tissue resistances with blunt needles, eliciting paresthesia, peripheral nerve stimulation (PNS), ultrasonography, and injection pressures [2,3]. However, addition of sophisticated modalities may not necessarily improve the success rate nor decrease the complication rate of peripheral nerve blocks, especially in the hands of experienced physicians.
In this review, the authors present the outcomes of randomized, controlled studies that compare single to dual guidance for regional anesthesia, concentrating on PNS in comparison with ultrasound guidance, or the combined use of the two technologies.
Evolution of regional anesthesia
In 1885, William Halsted performed the first brachial plexus block under direct visualization by applying cocaine directly to nerves that had been surgically exposed. Going forward, but before the invention of nerve stimulation, the nerves or nerve roots were recognized by the presence of paresthesia. Almost 100 years ago a German physician, Kulenkampff [4], used transcutaneous insertion of a needle and located nerves using the paresthesia technique. Paresthesia is a phenomenon whereby mechanical stimulation of a nerve results in a sensory feeling described as “an electric shock” in the sensory distribution of the nerve being contacted. Moore [5] stated “no paresthesias—no anesthesia,” which is still part of the controversy regarding the use of nerve stimulation. The knowledge of anatomy and its common variations are core to performing this technique, as is the ability to appreciate the fascial planes and tissue layers with the use of blunt needles. Patient understanding and cooperation greatly enhance success with this method. The success rate with these techniques is about 60% to 70% [6]. Moreover, paresthesia has been demonstrated to have poor sensitivity for needle to nerve contact [7].
Nerve stimulation became common in the late twentieth century and changed the face of regional anesthesia. In 1912, a peripheral nerve stimulator was introduced by Perthes, but the technique did not gain popularity until 1962, when a smaller and portable instrument was devised [8]. PNS provides an accurate approximation of the proximity of the stimulating needle tip to a nerve or plexus by using an electric current to elicit an objective functional motor response. One obvious advantage is that PNS causes minimal discomfort to patients, because the low stimulating currents (0.3–1.5 mA) readily stimulate the larger A-alpha motor fibers more than C pain fibers when short pulse duration (0.1 ms) is used [9]; this is in contrast to the paresthesia technique, which by its nature causes varying degrees of discomfort. A second advantage of PNS is that patient cooperation is not needed during the procedure, so a block can be performed in a lightly or moderately sedated patient, providing an extra degree of comfort. In addition, the incidence of nerve damage may be decreased with PNS as compared with paresthesia techniques [10,12], and the success rate with PNS may be equal to or greater than that from eliciting paresthesias [13]. Problems with this technique, however, are that a motor response may not be elicited if the tip of the needle is in contact with just the sensory portions of a given nerve [14], and a response to a stimulating current less than 0.5 mA does not guarantee extraneural placement [3,7,15,16].
History of ultrasonography and its evolving use in regional anesthesia
Doppler and sonography became common for the placement of supraclavicular blocks as early as 1978 [17]. Ting and Sivagnanaratnam [18] first used ultrasound to confirm needle placement and observe local anesthetic spread during axillary nerve blocks in 1989. These investigators reported a 100% success rate with no complications during this pilot study, and that they were able to visualize the needle tip and axillary anatomy at all times. Subsequently, Kapral and colleagues [19] demonstrated that ultrasound-guided supraclavicular blocks resulted in safe and more effective anesthesia than axillary blocks for the brachial plexus distribution.
Marhofer and colleagues [20] demonstrated improved success of “3-in-1” lower extremity blocks performed under ultrasound guidance as compared with nerve stimulation. These investigators further showed a reduction in the volume of local anesthetic required to produce an effective block with ultrasound guidance than with nerve stimulation [21]. The use of ultrasound localization of nerves was further advanced when a group of researchers in Toronto demonstrated high-quality images of the brachial plexus with ultrasound [22]. This group also confirmed the findings by Urmey [23] that contact of a stimulating needle with the nerves does not necessarily initiate a motor response [14,22].
Within the past 6 years, Brian Sites and his colleagues [24–27] have developed and published core competencies training for ultrasound-guided regional anesthesia, and developed curricula focused on ultrasound physics and establishing appropriate learning metrics and behavior during ultrasonographic skill development. These guidelines for education and training in ultrasound-guided regional anesthesia have been adapted and published by the American and European Societies of Regional Anesthesia, and comprise formal guidelines and minimum expectations required of regional anesthesia practitioners, educators, and researchers in an attempt to create uniformity of practice in different parts of the world. The studies reviewed in this article lack this kind of consistency, but the authors hope that researchers in the future will follow these guidelines and that reviewers of their articles will have an easier time comparing studies from various countries.
Upper extremity blocks
Evidence for Interscalene and Supraclavicular Blocks
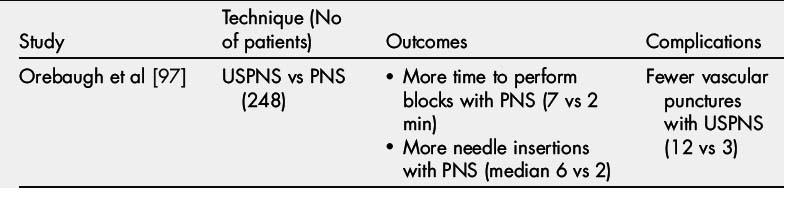
The upper extremity is especially well suited for ultrasound-guided regional anesthesia. High-frequency linear array transducers (10–15 Hz) provide very high-resolution images of the brachial plexus (Table 1) [28]. Supraclavicular blocks have regained popularity, because the dreaded complication of pneumothorax may be dramatically reduced with ultrasound-guided placement compared with the traditional landmark technique [17,19,29–32]. The interscalene and supraclavicular regions are rich in vessels and nerves, which helps allow clear identification of anatomic structures; conversely, it provides little room for error while performing regional blocks. Therefore, it seems likely that using ultrasound-guided regional anesthesia for the upper extremity may prevent severe complications (eg, vascular puncture and intravascular injection leading to local anesthetic systemic toxicity). However, differences between ultrasound-guided and PNS-guided blocks, as well as the combination of both techniques, are difficult to evaluate based on data available to date. Liu and colleagues [33] investigated ultrasound-guided and PNS-guided interscalene blocks in 219 patients, mainly to assess postoperative neurologic symptoms (PONS). These investigators found no difference in the failure rate, time to perform blocks, patient satisfaction, or postoperative neurologic outcome between techniques; however, they demonstrated fewer needle passes and quicker onset of motor block with ultrasound guidance [33]. This lack of difference in success (100% in both groups) could be attributed to the high volume of local anesthetic used in their study (55–65 mL mepivacaine 1.5% with sodium bicarbonate). In addition, this same group recently published a large prospective clinical registry of ultrasound-guided regional interscalene and supraclavicular blocks for shoulder surgery, demonstrating a 99.8% success rate of surgical anesthesia. The incidence of vascular puncture and permanent nerve injury was similarly low, at 0% (95% confidence interval [CI], 0%–0.3%), whereas the incidence of PONS was reported to be only 0.4% (95% CI, 0.1%–1%) [34].
Table 1 Randomized control trials comparing ultrasonography, peripheral nerve stimulation, or both for nerve block of upper extremities
By contrast, Kapral and colleagues [35] performed interscalene blocks using ultrasound in 160 patients, using a much lower volume of local anesthetic (20 mL of 0.75% ropivacaine). This study demonstrated both a quicker onset of sensory blockade and a stronger motor blockade in all nerves of the upper extremity, and detected anatomic variances in 11% of patients in the ultrasound group. In addition, they demonstrated an increased success rate in the ultrasound group (99%) versus the PNS group (90%). As elegantly described in the accompanying editorial [36], this could be caused by the methodological flaws of the study. For example, they used multiple injections for the ultrasound-guided group to ensure complete circumferential spread, but only a single stimulation for the PNS group, especially targeting for a twitch for middle and lower trunks only. Kapral and colleagues also highlight the lesser-known anatomic variation of the brachial plexus that constitutes roots located within the anterior or middle scalene muscles.
A single study performed by Williams and colleagues [30] compared combined ultrasound and PNS with anatomically guided PNS in 80 patients. These investigators demonstrated a higher success rate in complete block (95% vs 85%) and surgical anesthesia in the ultrasound group. Less time was required to perform the block in the ultrasound group (5.0 ± 2.4 minutes vs 9.8 ± 7.5 minutes, P = .0001).
The addition of nerve stimulation to ultrasound may not offer any advantage in supraclavicular blocks because about 13% of patients have no twitch response even after needle nerve contact, but will have successful surgical anesthesia [3,37].
Authors’ opinion
Interscalene and supraclavicular blocks should be performed under ultrasound guidance not only to avoid vascular or intrathecal puncture but also for a more circumferential spread of the local anesthetic, which is likely to increase the success rate. Ultrasonography would identify the abnormal location of one of the trunks within the scalene muscles. However, based on only one study in both interscalene (160 patients) and supraclavicular (80 patients) areas, it is difficult to comment as to whether using ultrasound and nerve stimulation guidance in combination will improve block quality, speed of onset, or duration of regional anesthesia.
Evidence for Infraclavicular Blocks
Compared with the supraclavicular area where the divisions of the brachial plexus are in close proximity to each other, the brachial plexus divides into cords below the clavicle. These cords surround the axillary artery laterally, medially, and posteriorly. Thus, methods for this block that use multiple-injection techniques are likely to achieve higher success rates than single-injection techniques. Eight randomized controlled studies have compared ultrasound-guided and PNS-guided infraclavicular blocks in adult patients [38–42]. Overall, 370 patients were included in these comparisons, with 37 to 103 patients per study. All studies reported a high success rate with either ultrasound guidance or with nerve stimulation guidance, without being able to demonstrate a clear difference between the 2 modes of nerve identification [38–41]. However, visualization of major anatomic structures by ultrasound appears to shorten the time to achieve a successful block [38,39]. Most studies failed to demonstrate a better quality of nerve blockade with one method over the other [38,40], but there was a trend toward a higher success rate in the ultrasound-guided groups [40]. Although limited by his small sample size, Gurkan and colleagues [41] demonstrated that the complication rate (eg, vascular puncture) was lower in the ultrasound-guided than in the PNS-guided group.
In contrast to the previous studies, Dingemans and colleagues [42] compared the combination of nerve stimulation and ultrasound guidance with ultrasound guidance alone for infraclavicular blocks. The trainee performing the block in all patients visualized the spread of the local anesthetic posterior to and to each side of the axillary artery in the ultrasound-only group with the minimum number of injections. The combined group received a single injection of local anesthetic after obtaining a distal motor response to nerve stimulation. Dingemans and colleagues concluded that infraclavicular nerve blocks were performed faster with a higher success rate in the ultrasound-only group. Patients with single injections in both groups had a similar success rate (86%), which reinforces the improved success with multiple injections.
Authors’ opinion
The majority of studies suggest that approaches using ultrasound guidance alone allow quicker performance and faster onset or surgical readiness of regional anesthesia, with fewer needle passes than nerve stimulation with or without ultrasound in the infraclavicular region. Thus nerve stimulation does not provide any additional benefit to ultrasound guidance in the infraclavicular region; however, ultrasound guidance seems to have a definite benefit over nerve stimulation alone in all aspects of regional anesthesia success as defined by onset time, success rate, and surgical anesthesia.
Evidence for Axillary Blocks/Single Nerve Blocks
Axillary brachial plexus block is performed at the level of terminal nerves surrounding the axillary artery in a sheath. Radial and musculocutaneous nerves are often missed with single-injection techniques. Multiple-injection techniques have been shown to provide a higher success rate and a shorter onset time compared with single-injection techniques, even though they take longer to perform [43]. If each of the 4 major nerves is blocked with localization by nerve stimulation rather than paresthesia, the success rate is more than 90%. Ultrasound techniques also have high success rates because it is possible to make multiple injections with visual confirmation around the 4 major nerves.
Multiple studies have focused on the effect of ultrasound on success rate, complications, and performance time of axillary brachial blockade. Morros and colleagues [44] demonstrated similar success rates with nerve stimulation–guided and combined ultrasound-guided and nerve stimulation–guided axillary plexus block, but the complication rate (eg, vascular puncture 8% vs 28%) dropped significantly as did the onset time of sensory and motor blockade with ultrasound-guided blocks. However, more time (350 seconds vs 291 seconds) was required to perform the procedure when nerve stimulation was combined with ultrasound.
The largest study conducted in axillary ultrasound-guided regional anesthesia by Chan and colleagues [45] (188 patients) had 3 groups (ultrasound alone, ultrasound with PNS, and PNS alone). The results clearly demonstrated that ultrasound, with or without PNS, was superior to PNS alone in terms of blockade of the 3 major nerves—radial, median, and ulnar. However, there was no clinical difference in terms of surgical anesthesia between groups (95%, 92%, and 86% in ultrasound, ultrasound with PNS, and PNS groups, respectively). In addition, complications such as postoperative axillary bruising and pain were less frequent in the groups in which ultrasound was used during block placement.
By contrast, Casati and colleagues [46] found no difference in success rate (100% in both groups) or time to onset of motor block with axillary blocks performed with ultrasound or nerve stimulation guidance with 4 separate injections. On the other hand, onset of sensory block was faster with ultrasound guidance compared with electrical guidance (14 minutes vs 18 minutes). Patient satisfaction was higher in the ultrasound group as well. In fact, almost 53% of patients with multiple nerve stimulations reported the procedure as painful [47], whereas 98% of patients receiving their blocks with ultrasound guidance reported high satisfaction and acceptance of their procedures [48]. Thus, ultrasound guidance may have an advantage in the performance of axillary plexus block in terms of patient comfort. Bloc and colleagues [49] confirmed this finding in their recent study comparing comfort of the patient during axillary block placement with PNS and ultrasound guidance.
Authors’ opinion
Overall patient comfort and satisfaction seem to be greater in patients receiving ultrasound-guided axillary blocks simply because nerve stimulation in this area is uncomfortable, requires more time, and use of ultrasound may be associated with a higher success rate. In terms of success rate, there is no evidence that dual guidance is superior to ultrasound alone in this region. Vascular puncture and bruising are likely to be reduced with use of ultrasound for axillary plexus block; thus, the authors recommend the routine use of ultrasound for this site.
Lower extremity blocks
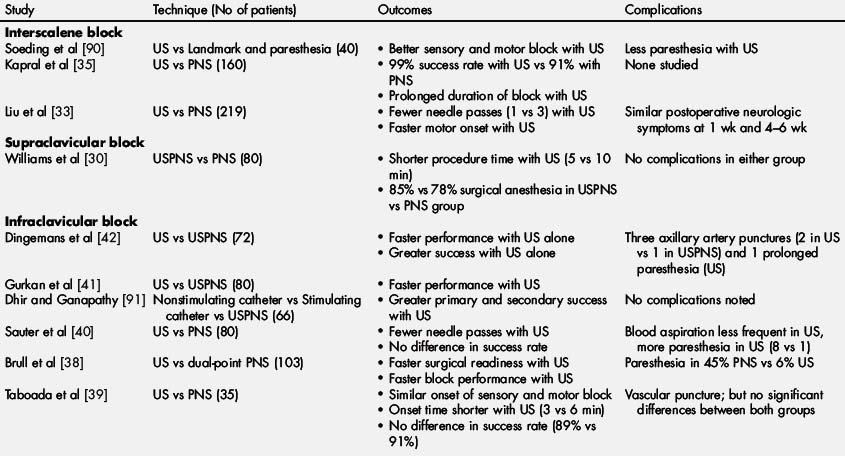
Unlike the upper extremities, there are relatively few studies that compare ultrasound with nerve stimulation guidance for lower extremity blocks, and in those available the total number of study subjects is small, allowing for limited interpretation of the results (Tables 2 and 3). A recent evidence-based review summarized the benefits of ultrasound versus nerve stimulation for lower extremity nerve block [50]. The conclusion was that there is level Ib evidence to make a grade A recommendation that ultrasound guidance improves onset and success of sensory block, decreases local anesthetic requirements, and needs decreased time to perform the lower extremity peripheral nerve blocks.
Table 2 Randomized control trials comparing ultrasonography, peripheral nerve stimulation, or both for nerve blocks of lower extremities
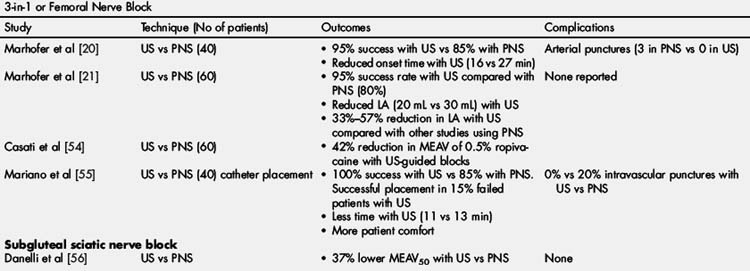
Complications with regional anesthesia are relatively rare; thus, it is difficult to comment on outcomes and safety based on 200 total patients undergoing femoral, 3-in-1, or fascia iliaca blocks, and slightly more than 200 patients undergoing sciatic nerve block. Comments can be made, however, about the success rate and block quality in these small studies, but even these results are subject to each institution’s expertise in performing these blocks. Abnormal location of femoral nerve makes it difficult to identify with ultrasound [51] or nerve stimulation alone, and ultrasound may not be of additional value in femoral nerve blocks with normal anatomy in terms of block efficacy. However, when in question, dual guidance may help the anesthesiologist to identify the desired target. For instance, at times the femoral nerve may not be very visible on the ultrasound screen and fascial structures either lateral or posterolateral to the femoral artery may appear as femoral nerve [52]. Here the authors present studies related to femoral and sciatic catheters that have included ultrasound-guided blocks in one of their study groups.
Evidence for Femoral Nerve Blocks and Catheter Placement
There is only one study that provides an anatomic basis to an educated approach to dual-guidance techniques to block peripheral nerves. Although not a direct comparison between the 2 techniques, a study by Nader and colleagues [53] demonstrates the anatomic basis for recommending dual-guidance techniques for femoral nerve blocks. Their cadaver dissections revealed that the branch to the quadriceps muscle originates from the lateral part of the common femoral nerve in 95% and medially in 5% of the specimens, while the fascicular branch to the sartorius muscle arises from the medial side of the common femoral nerve. A quadriceps contraction was elicited in 1.2% and 96% of the specimens when the medial and lateral aspects of the femoral nerve were stimulated, respectively. By contrast, a sartorius muscle contraction was elicited in 94% and 0% when stimulating the medial and lateral part of the femoral nerve, respectively. The investigators concluded that using out-of-plane ultrasound imaging at the inguinal crease to direct the stimulating needle to the lateral half of the femoral nerve should be associated with a higher probability of encountering the motor branch to the quadriceps muscle.
One of the proven advantages of ultrasound-guided femoral nerve block over nerve stimulation–guided blocks is the reduction of anesthetic dose. Studies have shown up to a 42% reduction in the mean effective anesthetic volume of local anesthetic needed to block the femoral nerve (15 mL in ultrasound vs 28 mL in PNS) [21,54]. With logistic regression and probit transformation, the estimated effective dose (ED95) for ultrasound was half of that for PNS (22 mL vs 41 mL) [21,54].
Adding nerve stimulation to ultrasound guidance (USPNS) does not seem to offer any advantages in terms of either a partial or complete block 40 minutes after local anesthetic injection (96% vs 88%; P = .19) [52]. There were more needle redirections in the USPNS group (4 vs 1, P<.001), with a higher percentage of patients requiring 2 or more needle attempts (44% vs 19%, P<.01), and the time to perform the block in USPNS group was longer (188 vs 148 seconds, P = .01). Thus, the addition of nerve stimulation to an ultrasound-guided femoral block did not improve efficacy as defined by the quality of the sensory and motor blocks, but did prolong the time to perform the procedure.
In a study by Mariano and colleagues [55], perineural catheters placed with ultrasound guidance (n = 20) took a median of 5.0 (range 3.9–10.0) minutes compared with 8.5 (4.8–30.0) minutes for the group using electrical stimulation (n = 20; P = .012). All ultrasound-guided catheters were placed within the parameters of the protocol (n = 20) versus only 85% of nerve stimulation–guided catheters (n = 20; P = .086). Patients in the ultrasound group found catheter placements to cause less discomfort than did those in the nerve stimulation group. There were no vascular punctures with ultrasound guidance, compared with 4 in the nerve stimulation group (P = .039).
Authors’ opinion
One of the major roles of the use of ultrasound will be to reduce the amount of local anesthetic required to block the femoral nerve and to reduce the incidence of vascular puncture; however, addition of nerve stimulation to ultrasound does not seem to offer further advantage in terms of time required to perform femoral blocks or their success rate. Successful continuous catheter placement may be facilitated with ultrasound guidance. Based on the anatomic study, an in-plane technique directed toward the lateral, rather than the medial, aspect of the nerve may have a higher likelihood of success with the femoral block when single or dual guidance is used.
Evidence for Sciatic Nerve Blocks
A single study [56] has examined an ultrasound-guided method to block the sciatic nerve at the subgluteal level, using the “up and down” method. Subjects in the ultrasound-guided group were reported to have a 37% reduction in mepivacaine requirements compared with those in the nerve stimulation–guided group. The reason for the lack of studies for this anatomic approach is probably because the sheer bulk of the gluteus maximums muscle makes the sciatic nerve more difficult to visualize at this anatomic approach [57], and nerve stimulation using palpable anatomic landmarks reliably provides quick and easy access to the sciatic nerve [58,59]. Abbas and Brull [60] mention in a letter to the editor their routine use of ultrasound at this level; however, it remains to be seen whether addition of ultrasound offers any advantage to this block.
Distal Sciatic Blocks at the Level of Midfemoral or Popliteal Region
Five randomized controlled trials (RCTs), including a total of 251 patients, have compared the use of ultrasound versus nerve stimulation guidance for sciatic nerve block at the popliteal level, which seems to be the preferred approach for many groups because of the ease of visualization of the nerve at this level. Danelli and colleagues [61] reported that although the onset times for sensory and motor blocks were comparable with the 2 methods, ultrasound guidance reduced needle redirections (P = .01), was associated with less procedural pain (P = .002), and required less time to perform (P = .002). The success rate was 100% for ultrasound-guided versus 82% for nerve stimulation–guided procedures (P = .116).
Mariano and colleagues [62] reported that perineural catheters placed with ultrasound guidance took a median of 5 (range 4–11) minutes compared with 10 (2–15) minutes for stimulation guidance (P = .034). Subjects in the ultrasound group experienced less pain during catheter placement, scoring a median discomfort of 0 (0.0–2.1) compared with 2.0 (0.0–5.0) for the stimulation group (P = .005) on a numeric rating scale of 0 to 10.
Perlas and colleagues [63] concluded that ultrasound guidance enhances the quality of single-injection popliteal sciatic nerve block compared with nerve stimulation–guided block using either a tibial or peroneal end point. Ultrasound guidance resulted in higher success rate (89% vs 60%), and faster onset and progression of sensorimotor block, without an increase in block procedure time or complications.
van Geffen and colleagues [64] concluded that the use of ultrasound localization for distal sciatic nerve block in the popliteal fossa reduced the required dose of local anesthetic (17 vs 37 mL, P<.001), reduced the number of needle passes required, and was associated with a higher success rate than nerve stimulation (100% vs 75%; P = .017), without changing block characteristics. A faster onset of both sensory and motor blockade with no change in block duration was also demonstrated.
Authors’ opinion
The sciatic nerve may be visualized with a high degree of success at the popliteal level with ultrasonography because of its superficial location. This delineation allows for a higher success rate compared with nerve stimulation techniques, and to faster onset of nerve block. There also seems to be less procedural pain and reduced local anesthetic requirements when ultrasound is employed in this area. These advantages could be attributed to a variable division of the sciatic nerve above the popliteal crease [65,66], which may prevent a complete circumferential spread of local anesthetic around both branches of sciatic nerve when using nerve stimulation alone. It may be advantageous to use dual guidance at this site.
Evidence for Neuraxial Blocks
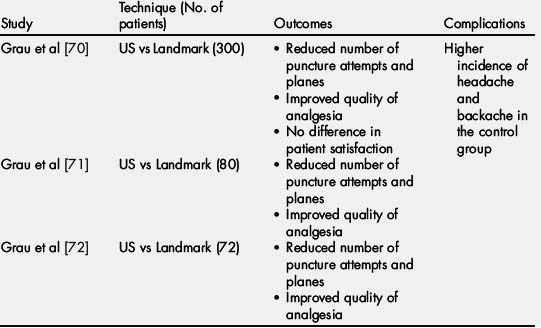
Studies have shown a strong correlation between depth of the epidural space from the skin as measured by ultrasound and as measured by loss of resistance via an epidural needle [67,69]. Subsequently, Grau and colleagues [70,72] completed 3 RCTs in adult obstetric patients (Table 4). Overall, these studies suggest that when used to identify the epidural space, level, and depth from skin to epidural space preprocedure, ultrasound reduces the number of punctures and the number of levels attempted, and improves the quality of resultant analgesia. Even in a patient population with expectation of difficult placement, either because of abnormal anatomy or previous history of difficult placement, catheter placement with ultrasound assistance resulted in higher patient satisfaction [72].
These same investigators subsequently demonstrated positive impacts on both patient care and in regional anesthesia education for neuraxial techniques [73] (see comment on education in ultrasound-guided anesthesia later in this article).
Some additional studies performed in the pediatric population and case reports published on ultrasound guidance for drainage of spinal abscess and use of ultrasound to guide lumbar facet nerve block [74] are beyond the scope of this review.
Authors’ opinion
Only 3 RCTs have been published on the use of ultrasound guidance in neuraxial blockade. Unfortunately, these studies are all from the same center with the same first author, who is an expert in ultrasonography of the spine. Therefore, more studies on patient populations other than obstetrics are needed to determine whether catheter placement guided by sonography of the neuraxis increases the speed or reliability of epidural analgesia/anesthesia. Although regional anesthesia performed in the obstetric population requires extensive experience, it would be interesting to determine whether the described results are reproducible in the thoracic spine, and in elderly patients or those with more challenging anatomic conditions.
Comparison of complications between guidance methods
Very few studies have actually shown a reduction of significant complications with ultrasound guidance as compared with nerve stimulation guidance. Renes and colleagues [75,76] demonstrated decreased occurrence of phrenic nerve block by using ultrasound in comparison with nerve stimulation for both supraclavicular blocks (0% ultrasound vs 53% PNS) and interscalene brachial plexus blocks (12% ultrasound vs 93% PNS). These investigators also reported objective evidence of impairment in the nerve stimulation group, including a significant reduction of forced expiratory volume in 1 second, forced vital capacity, and peak expiratory flow, along with evidence of paresis of the ipsilateral hemidiaphragm. A case report also described sparing of the phrenic nerve when an ultrasound-guided interscalene block was performed in a patient who had contralateral pneumonectomy [77].
A preliminary report from one of the largest studies on peripheral nerve blocks indicates that there is a reduction in the incidence of unintentional vascular puncture with the use of ultrasound because the practitioner can easily see the structures that need to be avoided (5% incidence with ultrasound vs 13% with PNS) [78]. Even though it seems intuitive that the needle tip may be visualized with ultrasound, occasional reports of seizures and cardiac arrest caused by local anesthetic toxicity have been reported even with the use of ultrasound [79,80]. Gnaho and colleagues [79] reported cardiac arrest while performing a sciatic block with a combined ultrasound and PNS technique. Barrington and colleagues [78] showed a similar incidence of local anesthetic systemic toxicity (0.98 per 1000 patients) with peripheral nerve blocks performed with either ultrasound or PNS techniques. By contrast, Auroy and colleagues [81] reported an incidence of between 0.75 and 2 incidents per 1000 patients in an earlier study performing peripheral nerve blocks with nerve stimulation. There was a trend toward lower local anesthetic toxicity in the ultrasound group (1.2 vs 0.8 per 1000 patients). Although the incidence of paresthesia was higher in the ultrasound group (20.5 vs 10.8 per 1000 patients), the late or long-term neurologic deficits were higher in the nerve stimulation group [78]. As noted previously, ultrasound-guided supraclavicular and interscalene blocks are associated with an extremely low incidence of vascular punctures and permanent nerve injury [34].
Limitations of ultrasound-guided regional anesthesia
Anesthesiologists using ultrasound in clinical practice need to appreciate and correctly interpret common ultrasound-generated, tissue-generated, and overlapping artifacts. Sono-anatomy of peripheral nerves is complex and continuing to be delineated. Accurate needle placement is facilitated by an “in-plane” approach, which can be challenging given narrow ultrasound beam widths. Higher-resolution images correlate with better image quality, which is a balance between spatial resolution (with higher frequencies) and depth of penetration (with lower frequencies); therefore, the authors expect that future ultrasound technology may be able to balance both these factors, and will increase the accuracy of nerve localization and perineural local anesthetic delivery.
Nerves may appear hypo- or hyperechoic on ultrasonography. In general, the hypoechoic areas correlate with the neural tissue and the hyperechoic structures correlate with the connective tissue. Because brachial plexus nerve roots may appear to be unifascicular or oligofascicular, they often produce hypoechoic shadows unlike the more peripheral nerves. The ratio of neural to nonneural tissue increases from 1:1 to 1:2 when comparing interscalene and supraclavicular regions with infraclavicular regions of the brachial plexus [82]. Different regions of the brachial plexus thus often manifest varying degrees of echogenicity, potentially confusing an ultrasound novice.
There are very few studies demonstrating the effectiveness of using ultrasound during placement of catheters at various sites [62,83]. An editorial by Mariano and colleagues [84] recently pointed out that a high or very high success rate with single-shot peripheral nerve blocks may not necessarily translate into a high success rate for perineural catheter placement, as the angle of the needle is very important for perineural catheter insertion, and it is difficult to visualize a catheter tip in relation to the target nerve as easily as it is to visualize needles with 2-dimensional ultrasound. Addition of stimulating catheters with the use of ultrasound may be an interesting area to study for improvement in the success rate of catheter placements.
Lastly, the cost of an ultrasound machine as compared with nerve stimulation equipment, and the effort and cost of training physicians in the core competencies of ultrasound-guided blocks, are among the major challenges faced by anesthesiologists attempting to incorporate ultrasound-guided regional anesthesia into their daily practice.
Advantages of ultrasound-guided regional anesthesia
High-resolution sonography provides visual information that is not obtainable by any other nerve localization method. The trained practitioner can image the vessels and nerves, including details up to 1 mm, depending on the frequency of the applied transducer and the quality of the ultrasound machine [85]. However, fascicles with small diameters (<1 mm) are not discerned with current high-frequency ultrasound technology and may only display about 33% of the total number of fascicles in a peripheral nerve [85]. If the needle tip is visualized, intraneural placement can be relatively easily discerned. PNS does not have the sensitivity to exclude direct needle tip to nerve contact or even intraneural placement, even with low stimulation currents [3]. In addition, studies show a reduction of the total dose of local anesthetic required to achieve surgical block when ultrasound was used compared with nerve stimulation alone. This dose sparing is in the range of 25% to 42% [54,86–89]. Thus, in summary, there may be an advantage of ultrasound in avoiding intravascular and intraneural injections, and a possible reduction of total amount of local anesthetic used.
Recommendations for dual guidance of regional anesthesia
Dual guidance of peripheral nerve blockade procedures with both nerve stimulation and ultrasound is definitely warranted under certain specific circumstances. Abnormal location of nerves makes it difficult to identify them reliably in all cases with ultrasound alone. Therefore, the combination of ultrasound and nerve stimulation is recommended in these cases. One important example of common abnormal nerve location involves the femoral nerve, as mentioned earlier. Additional indications are listed below and largely derive from situations involving difficulties with using either technique alone, because of either patient- or provider-imposed limitations. Based on the lack of concordance between the current output and the needle tip to nerve, it may be more useful and appropriate to use PNS (in conjunction with ultrasound) as a qualitative tool (“yes or no”) to confirm the location of peripheral nerve rather than attempting to achieve a predefined minimum current output.
Summary
Ultrasound guidance for peripheral nerve block performance is a relatively new technique. Consequently, available data in the literature are somewhat limited and interpretations are preliminary. Although nerve stimulation has been the standard of care for several decades and has been proved to be safe in experienced hands, the success rate varies in the hands of inexperienced care providers. However, does this justify the call for dual guidance, or is it more appropriate to provide additional training to produce higher predictability with one or the other modality?
Considering that dual guidance does not consistently produce better results with regional anesthesia, to add ultrasound to a very successful nerve stimulation–based practice will add cost for an experienced regional anesthesiologist, who may find little value in adding ultrasonography to routine practice. Although the literature comparing dual guidance with single guidance generally indicates better success rates with some blocks, it is important to realize that groups with high success rates and short procedural times reportedly using peripheral nerve stimulators alone also use multiple guidance techniques. Such techniques may be in the form of a strong anatomic background that includes a good knowledge of anatomic variations, good feel of the tissue and fascial planes with blunt needles, and paying attention to patients’ reporting of paresthesia or pain on injection [59].
In essence, ultrasound guidance or nerve stimulation, alone or in combination, allow high success rates with peripheral nerve blocks. Whether purchase of new equipment and adjustment to a relatively new technique will be efficient for individual institutions depends on the nature of the practice, the number of challenging patients (difficult anatomies, high number of comorbidities), and the expertise of the personnel in one technology or another. The literature favors neither sole technique nor dual techniques strongly, other than for cases in which difficult anatomy reduces success with a “single” technique approach. Nevertheless, in cases of doubt combinations of various techniques (eg, ultrasound or nerve stimulation) will help to avoid serious—although rare—complications.
Future developments, including reduced costs and improvements in image quality available with ultrasound machines, as well as formal training in ultrasound-guided techniques, seem likely to turn the tide toward ultrasound-based techniques as an integral part of regional anesthesia practice.
References
[1] A. Hadzic, X. Sala-Blanch, D. Xu. Ultrasound guidance may reduce but not eliminate complications of peripheral nerve blocks. Anesthesiology. 2008;108(4):557-558.
[2] J.C. Gadsden, D.M. Lindenmuth, A. Hadzic, et al. Lumbar plexus block using high-pressure injection leads to contralateral and epidural spread. Anesthesiology. 2008;109(4):683-688.
[3] C. Robards, A. Hadzic, L. Somasundaram, et al. Intraneural injection with low-current stimulation during popliteal sciatic nerve block. Anesth Analg. 2009;109(2):673-677.
[4] D. Kulenkampff. Zur Anaesthesierung des Plaxus brachialis. On anesthesia of the brachial plexus. Zentralblatt fuer Chirurgie. 1911;38:13.
[5] D.C. Moore. “No paresthesias-no anesthesia,” the nerve stimulator or neither? Reg Anesth. 1997;22(4):388-390.
[6] S. Sia, M. Bartoli, A. Lepri, et al. Multiple-injection axillary brachial plexus block: a comparison of two methods of nerve localization-nerve stimulation versus paresthesia. Anesth Analg. 2000;91(3):647-651.
[7] A. Perlas, A. Niazi, C. McCartney, et al. The sensitivity of motor response to nerve stimulation and paresthesia for nerve localization as evaluated by ultrasound. Reg Anesth Pain Med. 2006;31(5):445-450.
[8] G.M. Greenblatt, J.S. Denson. Needle nerve stimulator locator: nerve blocks with a new instrument for locating nerves. Anesth Analg. 1962;41:599-602.
[9] C.E. Pither. Insulation of needles. Anaesthesia. 1988;43(11):991.
[10] D. Selander. Paresthesias or no paresthesias? Nerve complications after neural blockades. Acta Anaesthesiol Belg. 1988;39(3 Suppl 2):173-174.
[11] D. Selander. Peripheral nerve damage and regional anaesthesia. Br J Anaesth. 1995;75(1):116-117.
[12] D. Selander, S. Edshage, T. Wolff. Paresthesiae or no paresthesiae? Nerve lesions after axillary blocks. Acta Anaesthesiol Scand. 1979;23(1):27-33.
[13] M.E. Goldberg, C. Gregg, G.E. Larijani, et al. A comparison of three methods of axillary approach to brachial plexus blockade for upper extremity surgery. Anesthesiology. 1987;66(6):814-816.
[14] W.F. Urmey, J. Stanton. Inability to consistently elicit a motor response following sensory paresthesia during interscalene block administration. Anesthesiology. 2002;96(3):552-554.
[15] W.F. Urmey. Using the nerve stimulator for peripheral or plexus nerve blocks. Minerva Anestesiol. 2006;72(6):467-471.
[16] V.W. Chan, R. Brull, C.J. McCartney, et al. An ultrasonographic and histological study of intraneural injection and electrical stimulation in pigs. Anesth Analg. 2007;104(5):1281-1284. [tables of contents]
[17] P. la Grange, P.A. Foster, L.K. Pretorius. Application of the Doppler ultrasound bloodflow detector in supraclavicular brachial plexus block. Br J Anaesth. 1978;50(9):965-967.
[18] P.L. Ting, V. Sivagnanaratnam. Ultrasonographic study of the spread of local anaesthetic during axillary brachial plexus block. Br J Anaesth. 1989;63(3):326-329.
[19] S. Kapral, P. Krafft, K. Eibenberger, et al. Ultrasound-guided supraclavicular approach for regional anesthesia of the brachial plexus. Anesth Analg. 1994;78(3):507-513.
[20] P. Marhofer, K. Schrogendorfer, H. Koinig, et al. Ultrasonographic guidance improves sensory block and onset time of three-in-one blocks. Anesth Analg. 1997;85(4):854-857.
[21] P. Marhofer, K. Schrogendorfer, T. Wallner, et al. Ultrasonographic guidance reduces the amount of local anesthetic for 3-in-1 blocks. Reg Anesth Pain Med. 1998;23(6):584-588.
[22] A. Perlas, V.W. Chan, M. Simons. Brachial plexus examination and localization using ultrasound and electrical stimulation: a volunteer study. Anesthesiology. 2003;99(2):429-435.
[23] W.F. Urmey. Interscalene block: the truth about twitches. Reg Anesth Pain Med. 2000;25(4):340-342.
[24] B.D. Sites, V.W. Chan, J.M. Neal, et al. The American Society of Regional Anesthesia and Pain Medicine and the European Society of Regional Anaesthesia and Pain Therapy joint committee recommendations for education and training in ultrasound-guided regional anesthesia. Reg Anesth Pain Med. 2009;34(1):40-46.
[25] B.D. Sites, J.D. Gallagher, J. Cravero, et al. The learning curve associated with a simulated ultrasound-guided interventional task by inexperienced anesthesia residents. Reg Anesth Pain Med. 2004;29(6):544-548.
[26] B.D. Sites, R. Brull, V.W. Chan, et al. Artifacts and pitfall errors associated with ultrasound-guided regional anesthesia. Part I: understanding the basic principles of ultrasound physics and machine operations. Reg Anesth Pain Med. 2007;32(5):412-418.
[27] B.D. Sites, J.M. Neal, V. Chan. Ultrasound in regional anesthesia: where should the “focus” be set? Reg Anesth Pain Med. 2009;34(6):531-533.
[28] B.D. Sites, R. Brull. Ultrasound guidance in peripheral regional anesthesia: philosophy, evidence-based medicine, and techniques. Curr Opin Anaesthesiol. 2006;19(6):630-639.
[29] V.W. Chan, A. Perlas, R. Rawson, et al. Ultrasound-guided supraclavicular brachial plexus block. Anesth Analg. 2003;97(5):1514-1517.
[30] S.R. Williams, P. Chouinard, G. Arcand, et al. Ultrasound guidance speeds execution and improves the quality of supraclavicular block. Anesth Analg. 2003;97(5):1518-1523.
[31] A. Perlas, G. Lobo, N. Lo, et al. Ultrasound-guided supraclavicular block: outcome of 510 consecutive cases. Reg Anesth Pain Med. 2009;34(2):171-176.
[32] B.C. Tsui, K. Doyle, K. Chu, et al. Case series: ultrasound-guided supraclavicular block using a curvilinear probe in 104 day-case hand surgery patients. Can J Anaesth. 2009;56(1):46-51.
[33] S.S. Liu, V.M. Zayas, M.A. Gordon, et al. A prospective, randomized, controlled trial comparing ultrasound versus nerve stimulator guidance for interscalene block for ambulatory shoulder surgery for postoperative neurological symptoms. Anesth Analg. 2009;109(1):265-271.
[34] S.S. Liu, M.A. Gordon, P.M. Shaw, et al. A prospective clinical registry of ultrasound-guided regional anesthesia for ambulatory shoulder surgery. Anesth Analg. 2010;111(3):617-623.
[35] S. Kapral, M. Greher, G. Huber, et al. Ultrasonographic guidance improves the success rate of interscalene brachial plexus blockade. Reg Anesth Pain Med. 2008;33(3):253-258.
[36] F.V. Salinas, J.M. Neal. A tale of two needle passes. Reg Anesth Pain Med. 2008;33(3):195-198.
[37] M.L. Beach, B.D. Sites, J.D. Gallagher. Use of a nerve stimulator does not improve the efficacy of ultrasound-guided supraclavicular nerve blocks. J Clin Anesth. 2006;18(8):580-584.
[38] R. Brull, M. Lupu, A. Perlas, et al. Compared with dual nerve stimulation, ultrasound guidance shortens the time for infraclavicular block performance. Can J Anaesth. 2009;56(11):812-818.
[39] M. Taboada, J. Rodriguez, M. Amor, et al. Is ultrasound guidance superior to conventional nerve stimulation for coracoid infraclavicular brachial plexus block? Reg Anesth Pain Med. 2009;34(4):357-360.
[40] A.R. Sauter, M.S. Dodgson, A. Stubhaug, et al. Electrical nerve stimulation or ultrasound guidance for lateral sagittal infraclavicular blocks: a randomized, controlled, observer-blinded, comparative study. Anesth Analg. 2008;106(6):1910-1915.
[41] Y. Gurkan, T. Hosten, M. Solak, et al. Lateral sagittal infraclavicular block: clinical experience in 380 patients. Acta Anaesthesiol Scand. 2008;52(2):262-266.
[42] E. Dingemans, S.R. Williams, G. Arcand, et al. Neurostimulation in ultrasound-guided infraclavicular block: a prospective randomized trial. Anesth Analg. 2007;104(5):1275-1280. [tables of contents]
[43] Z.J. Koscielniak-Nielsen, H.L. Stens-Pedersen, F.K. Lippert. Readiness for surgery after axillary block: single or multiple injection techniques. Eur J Anaesthesiol. 1997;14(2):164-171.
[44] C. Morros, M.D. Perez-Cuenca, X. Sala-Blanch, et al. [Contribution of ultrasound guidance to the performance of the axillary brachial plexus block with multiple nerve stimulation]. Rev Esp Anestesiol Reanim. 2009;56(2):69-74. [in Spanish]
[45] V.W. Chan, A. Perlas, C.J. McCartney, et al. Ultrasound guidance improves success rate of axillary brachial plexus block. Can J Anaesth. 2007;54(3):176-182.
[46] A. Casati, G. Danelli, M. Baciarello, et al. A prospective, randomized comparison between ultrasound and nerve stimulation guidance for multiple injection axillary brachial plexus block. Anesthesiology. 2007;106(5):992-996.
[47] Z.J. Koscielniak-Nielsen, P. Rotboll-Nielsen, H. Rassmussen. Patients’ experiences with multiple stimulation axillary block for fast-track ambulatory hand surgery. Acta Anaesthesiol Scand. 2002;46(7):789-793.
[48] B.S. Frederiksen, Z.J. Koscielniak-Nielsen, R.B. Jacobsen, et al. Procedural pain of an ultrasound-guided brachial plexus block: a comparison of axillary and infraclavicular approaches. Acta Anaesthesiol Scand. 2010;54(4):408-413.
[49] S. Bloc, L. Mercadal, T. Garnier, et al. Comfort of the patient during axillary blocks placement: a randomized comparison of the neurostimulation and the ultrasound guidance techniques. Eur J Anaesthesiol. 2010;27(7):628-633.
[50] F.V. Salinas. Ultrasound and review of evidence for lower extremity peripheral nerve blocks. Reg Anesth Pain Med. 2010;35(Suppl 2):S16-S25.
[51] H. Gurnaney, F. Kraemer, A. Ganesh. Ultrasound and nerve stimulation to identify an abnormal location of the femoral nerve. Reg Anesth Pain Med. 2009;34(6):615.
[52] B.D. Sites, M.L. Beach, C.D. Chinn, et al. A comparison of sensory and motor loss after a femoral nerve block conducted with ultrasound versus ultrasound and nerve stimulation. Reg Anesth Pain Med. 2009;34(5):508-513.
[53] A. Nader, K. Malik, M.C. Kendall, et al. Relationship between ultrasound imaging and eliciting motor response during femoral nerve stimulation. J Ultrasound Med. 2009;28(3):345-350.
[54] A. Casati, M. Baciarello, S. Di Cianni, et al. Effects of ultrasound guidance on the minimum effective anaesthetic volume required to block the femoral nerve. Br J Anaesth. 2007;98(6):823-827.
[55] E.R. Mariano, V.J. Loland, N.S. Sandhu, et al. Ultrasound guidance versus electrical stimulation for femoral perineural catheter insertion. J Ultrasound Med. 2009;28(11):1453-1460.
[56] G. Danelli, D. Ghisi, A. Fanelli, et al. The effects of ultrasound guidance and neurostimulation on the minimum effective anesthetic volume of mepivacaine 1.5% required to block the sciatic nerve using the subgluteal approach. Anesth Analg. 2009;109(5):1674-1678.
[57] J. Bruhn, N. Moayeri, G.J. Groen, et al. Soft tissue landmark for ultrasound identification of the sciatic nerve in the infragluteal region: the tendon of the long head of the biceps femoris muscle. Acta Anaesthesiol Scand. 2009;53(7):921-925.
[58] P. Di Benedetto, A. Casati, L. Bertini, et al. Posterior subgluteal approach to block the sciatic nerve: description of the technique and initial clinical experiences. Eur J Anaesthesiol. 2002;19(9):682-686.
[59] A. Wadhwa, H. Tlucek, D. Sessler. A simple approach to the sciatic nerve that does not require geometric calculations or multiple landmarks. Anesth Analg. 2010;110(3):958-963.
[60] S. Abbas, R. Brull. Ultrasound-guided sciatic nerve block: description of a new approach at the subgluteal space. Br J Anaesth. 2007;99(3):445-446. [author reply: 445–6]
[61] G. Danelli, A. Fanelli, D. Ghisi, et al. Ultrasound vs nerve stimulation multiple injection technique for posterior popliteal sciatic nerve block. Anaesthesia. 2009;64(6):638-642.
[62] E.R. Mariano, G.S. Cheng, L.P. Choy, et al. Electrical stimulation versus ultrasound guidance for popliteal-sciatic perineural catheter insertion: a randomized controlled trial. Reg Anesth Pain Med. 2009;34(5):480-485.
[63] A. Perlas, R. Brull, V.W. Chan, et al. Ultrasound guidance improves the success of sciatic nerve block at the popliteal fossa. Reg Anesth Pain Med. 2008;33(3):259-265.
[64] G.J. van Geffen, E. van den Broek, G.J. Braak, et al. A prospective randomised controlled trial of ultrasound guided versus nerve stimulation guided distal sciatic nerve block at the popliteal fossa. Anaesth Intensive Care. 2009;37(1):32-37.
[65] J.D. Vloka, A. Hadzic, E. April, et al. The division of the sciatic nerve in the popliteal fossa: anatomical implications for popliteal nerve blockade. Anesth Analg. 2001;92(1):215-217.
[66] U. Schwemmer, C.K. Markus, C.A. Greim, et al. Sonographic imaging of the sciatic nerve division in the popliteal fossa. Ultraschall Med. 2005;26(6):496-500.
[67] J.M. Currie. Measurement of the depth to the extradural space using ultrasound. Br J Anaesth. 1984;56(4):345-347.
[68] D.H. Wallace, J.M. Currie, L.C. Gilstrap, et al. Indirect sonographic guidance for epidural anesthesia in obese pregnant patients. Reg Anesth. 1992;17(4):233-236.
[69] M. Bonazzi, L. Bianchi De Grazia, S. Di Gennaro, et al. [Ultrasonography-guided identification of the lumbar epidural space]. Minerva Anestesiol. 1995;61(5):201-205. [in Italian]
[70] T. Grau, R.W. Leipold, R. Conradi, et al. Efficacy of ultrasound imaging in obstetric epidural anesthesia. J Clin Anesth. 2002;14(3):169-175.
[71] T. Grau, R.W. Leipold, R. Conradi, et al. Ultrasound imaging facilitates localization of the epidural space during combined spinal and epidural anesthesia. Reg Anesth Pain Med. 2001;26(1):64-67.
[72] T. Grau, R.W. Leipold, R. Conradi, et al. Ultrasound control for presumed difficult epidural puncture. Acta Anaesthesiol Scand. 2001;45(6):766-771.
[73] T. Grau, E. Bartusseck, R. Conradi, et al. Ultrasound imaging improves learning curves in obstetric epidural anesthesia: a preliminary study. Can J Anaesth. 2003;50(10):1047-1050.
[74] M. Greher, G. Scharbert, L.P. Kamolz, et al. Ultrasound-guided lumbar facet nerve block: a sonoanatomic study of a new methodologic approach. Anesthesiology. 2004;100(5):1242-1248.
[75] S.H. Renes, H.C. Rettig, M.J. Gielen, et al. Ultrasound-guided low-dose interscalene brachial plexus block reduces the incidence of hemidiaphragmatic paresis. Reg Anesth Pain Med. 2009;34(5):498-502.
[76] S.H. Renes, H.H. Spoormans, M.J. Gielen, et al. Hemidiaphragmatic paresis can be avoided in ultrasound-guided supraclavicular brachial plexus block. Reg Anesth Pain Med. 2009;34(6):595-599.
[77] N.T. Jack, S.H. Renes, J. Bruhn, et al. Phrenic nerve-sparing ultrasound-guided interscalene brachial plexus block in a patient with a contralateral pneumonectomy. Reg Anesth Pain Med. 2009;34(6):618.
[78] M.J. Barrington, S.A. Watts, S.R. Gledhill, et al. Preliminary results of the Australasian Regional Anaesthesia Collaboration: a prospective audit of more than 7000 peripheral nerve and plexus blocks for neurologic and other complications. Reg Anesth Pain Med. 2009;34(6):534-541.
[79] A. Gnaho, S. Eyrieux, M. Gentili. Cardiac arrest during an ultrasound-guided sciatic nerve block combined with nerve stimulation. Reg Anesth Pain Med. 2009;34(3):278.
[80] C. Loubert, S.R. Williams, F. Helie, et al. Complication during ultrasound-guided regional block: accidental intravascular injection of local anesthetic. Anesthesiology. 2008;108(4):759-760.
[81] Y. Auroy, P. Narchi, A. Messiah, et al. Serious complications related to regional anesthesia: results of a prospective survey in France. Anesthesiology. 1997;87(3):479-486.
[82] N. Moayeri, P.E. Bigeleisen, G.J. Groen. Quantitative architecture of the brachial plexus and surrounding compartments, and their possible significance for plexus blocks. Anesthesiology. 2008;108(2):299-304.
[83] M.J. Fredrickson, C.M. Ball, A.J. Dalgleish. A prospective randomized comparison of ultrasound guidance versus neurostimulation for interscalene catheter placement. Reg Anesth Pain Med. 2009;34(6):590-594.
[84] E.R. Mariano, V.J. Loland, B.M. Ilfeld. Interscalene perineural catheter placement using an ultrasound-guided posterior approach. Reg Anesth Pain Med. 2009;34(1):60-63.
[85] E. Silvestri, C. Martinoli, L.E. Derchi, et al. Echotexture of peripheral nerves: correlation between US and histologic findings and criteria to differentiate tendons. Radiology. 1995;197(1):291-296.
[86] U. Eichenberger, S. Stockli, P. Marhofer, et al. Minimal local anesthetic volume for peripheral nerve block: a new ultrasound-guided, nerve dimension-based method. Reg Anesth Pain Med. 2009;34(3):242-246.
[87] P. Marhofer, U. Eichenberger, S. Stockli, et al. Ultrasonographic guided axillary plexus blocks with low volumes of local anaesthetics: a crossover volunteer study. Anaesthesia. 2010;65(3):266-271.
[88] N.S. Sandhu, C.S. Bahniwal, L.M. Capan. Feasibility of an infraclavicular block with a reduced volume of lidocaine with sonographic guidance. J Ultrasound Med. 2006;25(1):51-56.
[89] N.S. Sandhu, B. Maharlouei, B. Patel, et al. Simultaneous bilateral infraclavicular brachial plexus blocks with low-dose lidocaine using ultrasound guidance. Anesthesiology. 2006;104(1):199-201.
[90] P.E. Soeding, S. Sha, C.E. Royse, et al. A randomized trial of ultrasound-guided brachial plexus anaesthesia in upper limb surgery. Anaesth Intensive Care. 2005;33(6):719-725.
[91] S. Dhir, S. Ganapathy. Use of ultrasound guidance and contrast enhancement: a study of continuous infraclavicular brachial plexus approach. Acta Anaesthesiol Scand. 2008;52(3):338-342.
[92] Q.H. De Tran, P. Bertini, C. Zaouter, et al. A prospective, randomized comparison between single- and double-injection ultrasound-guided infraclavicular brachial plexus block. Reg Anesth Pain Med. 2010;35(1):16-21.
[93] F.C. Liu, J.T. Liou, Y.F. Tsai, et al. Efficacy of ultrasound-guided axillary brachial plexus block: a comparative study with nerve stimulator-guided method. Chang Gung Med J. 2005;28(6):396-402.
[94] B.D. Sites, B.C. Spence, J.D. Gallagher, et al. On the edge of the ultrasound screen: Regional anesthesiologists diagnosing nonneural pathology. Reg Anesth Pain Med. 2006;31(6):555-562.
[95] W.P. Yu, X.Z. Xu, D.Z. Wu, et al. [Efficacy of axillary approach brachial plexus blocking by ultrasound-guided four points via one-puncture technique]. Zhonghua Yi Xue Za Zhi. 2007;87(11):740-745. [in Chinese]
[96] V. Domingo-Triado, S. Selfa, F. Martinez, et al. Ultrasound guidance for lateral midfemoral sciatic nerve block: a prospective, comparative, randomized study. Anesth Analg. 2007;104(5):1270-1274.
[97] S.L. Orebaugh, B.A. Williams, M.L. Kentor. Ultrasound guidance with nerve stimulation reduces the time necessary for resident peripheral nerve blockade. Reg Anesth Pain Med. 2007;32(5):448-454.