Optic Neuropathies and Papilledema
Optic Neuritis
Optic neuritis or inflammation of the optic nerve is the most common cause of optic neuropathy in young adults. Optic neuritis can be idiopathic or associated with demyelinating lesions (e.g. multiple sclerosis), infectious and para-infectious conditions, inflammatory and post-vaccination conditions and autoimmune diseases. OCT B-scans through the optic nerve head can document disc edema in acute optic neuritis. Optic nerve head and retinal nerve fiber layer thickening analysis can reflect changes related to optic disc edema, as well as progressive changes related to long-term axonal loss and optic atrophy (Fig. 6.2.1).
Disc Edema/Papilledema
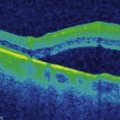
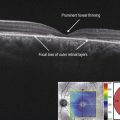
Optic nerve head swelling or disc edema occurs in many pathologic conditions of the optic nerve. It is thought to represent a stasis in axoplasmic flow through the retinal nerve fiber layer due to biochemical and structural reasons and manifests itself by swelling and thickening of the retinal nerve fiber layer. Papilledema is edema of the optic nerve due to elevated intracranial pressure (ICP). OCT features include increased total retinal thickness and retinal nerve fiber layer (RNFL) thickness on the optic nerve volumetric scan. The total retinal thickness is more sensitive than the RNFL thickness both in early cases of papilledema where RNFL thickness may miss some cases, as well as in cases of severe edema where software breakdown on retinal segmentation may give inaccurate values of RNFL thickness (Fig. 6.2.2). Recent studies suggest that increased thickening of the peripapillary RNFL is associated with increased ICP in newly diagnosed patients with papilledema. In patients with long-term severe papilledema, SD-OCT appears to be of limited value in predicting increased ICP. Interestingly, it has been shown on B-scans through the optic nerve head that some patients with papilledema may exhibit inward angulation of the peripapillary RPE/Bruch’s membrane (BM) layer at the neural canal opening, which does not occur in other causes of disc edema.
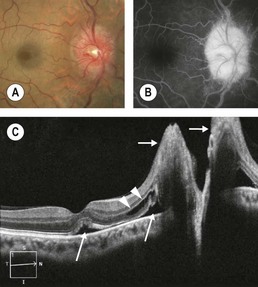
Figure 6.2.2 (A) Photograph of papilledema in the setting of increased ICP. (B) Fluorescein angiography shows significant late leakage from the optic nerve head. (C) OCT line scan shows profound optic disc thickening (short arrows), subretinal fluid (long arrows), and cystoid macular edema (arrowheads).
Optic Atrophy
This is the final common pathway for many optic nerve disorders. Nerve fiber layer scans show thinning of the RNFL. OCT measurements of peripapillary RNFL thickness and of macular retinal ganglion cell thickness can also be affected, starting in early stages of the disease (Fig. 6.2.3).
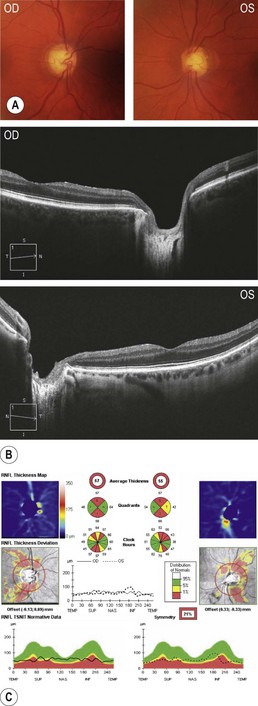
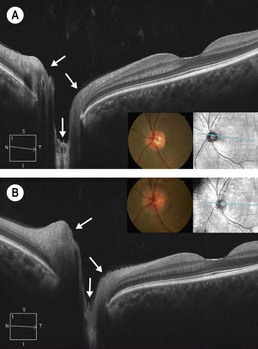
Figure 6.2.3 (A) Color fundus photographs and a (B) B-scan through the optic nerve head of a patient with optic atrophy. OCT B-scans through the optic nerve head show enlarged cupping in both eyes due to retinal ganglion cell’s axonal loss, and optic nerve head and (C) RNFL analysis shows abnormally reduced RNFL thickness in both eyes.