Operative Setup and Entry Into the Retropubic Space
Operations involving the retropubic space are best done with the patient in the supine position and the patient’s legs in a frogleg position or, preferably, in low Allen stirrups. Many of these operations are best performed with a hand in the vagina, which allows easy access to the vaginal area. The vagina, perineum, and abdomen are all sterilely prepped and draped in a fashion that permits easy access to the lower abdomen and the vagina. We prefer to use a three-way Foley catheter with a 30-mL balloon that is inserted sterilely into the bladder and kept in the sterile field. This allows easy palpation of the bladder neck, and in situations where the edges of the bladder are not clearly delineated, one can easily fill the bladder in a retrograde fashion to help in dissection or to help diagnose a small cystotomy or inadvertent suture placement in the bladder. The drainage port of the catheter is left to gravity drainage, and the irrigation port is connected to sterile water that is placed on an IV pole. One perioperative IV dose of an appropriate prophylactic antibiotic is given for retropubic operations.
A Pfannenstiel or Cherney incision (Figs. 32–1 and 32–2) (also see Chapter 8) is used to gain entry to the retropubic space. If intraperitoneal surgery is also being performed, the peritoneum is left open until the retropubic repair is completed. Routine assessment and, if appropriate, obliteration of the cul-de-sac are performed in these situations (see Chapter 41). The retropubic space is exposed by staying close to the back of the pubic bone (Fig. 32–3). The surgeon’s hand is used to gently displace the bladder and urethra downward (Fig. 32–4). As was previously mentioned, the presence of a large Foley balloon helps facilitate this dissection (Fig. 32–5). Sharp dissection usually is not necessary in primary cases. If a previous retropubic or needle suspension procedure or suburethral sling procedure has been performed, or in rare situations when pelvic surgery has led to dense suprapubic adhesions, sharp dissection should be utilized to enter the space. Adhesions should be dissected sharply from the pubic bone until the anterior bladder wall, urethra, and vagina are free of adhesions and are mobile. If identification of the urethra or lower border of the bladder is difficult, one may perform a high cystotomy, which, with a finger inside the bladder, helps to define the bladder’s lower limits for easier dissection, mobilization, and subsequent elevation of the paravaginal tissue (see Chapter 30).
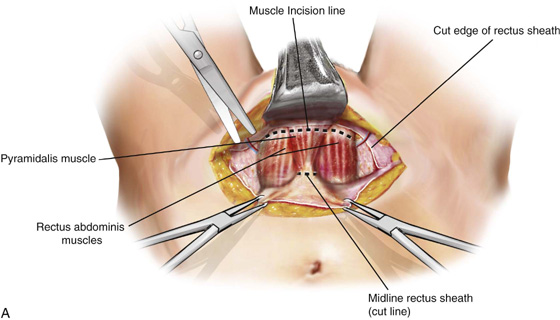
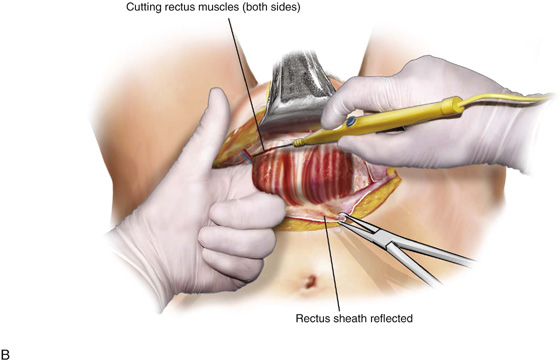
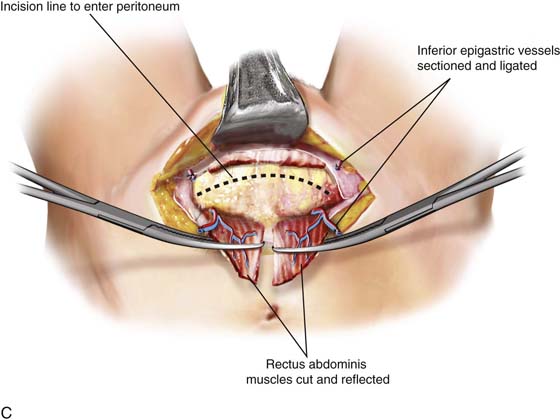
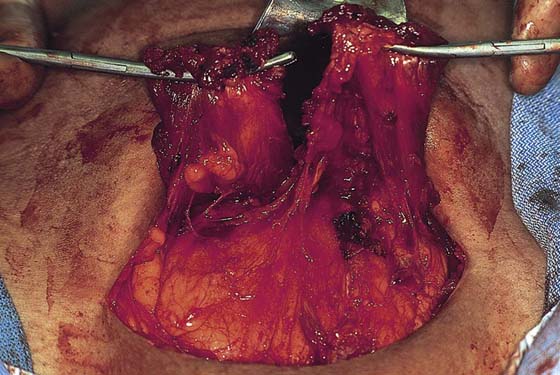
FIGURE 32–1 Technique of performing a Cherney incision to facilitate entrance into the retropubic space. A. Rectus muscle isolated and exposed very low near its insertion into the pubic bone. B. Monopolar cautery is used to cut through the lowest portion of the rectus muscle. C. The rectus muscle is reflected back, allowing easy access to the retropubic space. Note that if the peritoneum is going to be entered, it should be opened with a transverse incision.
FIGURE 32–2 A Cherney incision is commonly utilized for retropubic procedures, especially if lower abdominal or retropubic scarring is encountered. Note that the rectus abdominis muscles have been detached from the back of the symphysis pubis, very near their insertion. The muscles are then carefully dissected off the anterior peritoneum. Care must be taken to avoid the inferior epigastric vessels.
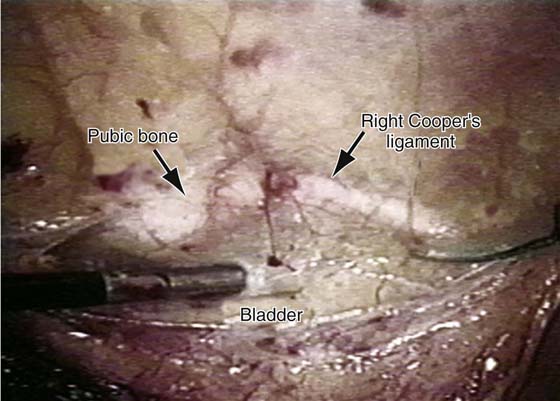
FIGURE 32–3 This figure demonstrates the upper portion of the retropubic space viewed laparoscopically. Note: In a patient who has not had any previous retropubic surgery, an avascular plane of dissection is initiated at the level of the pubic bone. The bladder is displaced in a downward direction, and the dissection instrument or finger is maintained in direct contact with the back of the pubic bone at the midline.
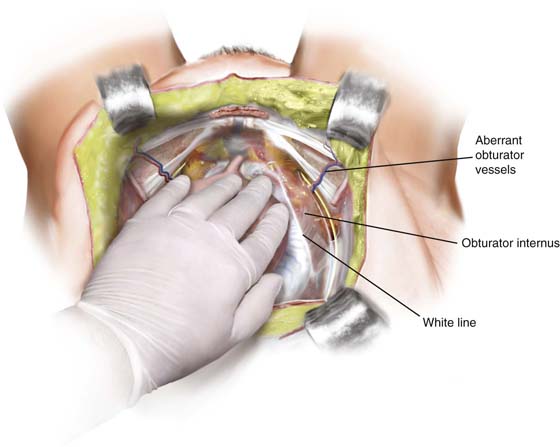
FIGURE 32–4 Technique used to expose the retropubic space. The surgeon’s hand is used to gently displace the bladder and urethra downward.
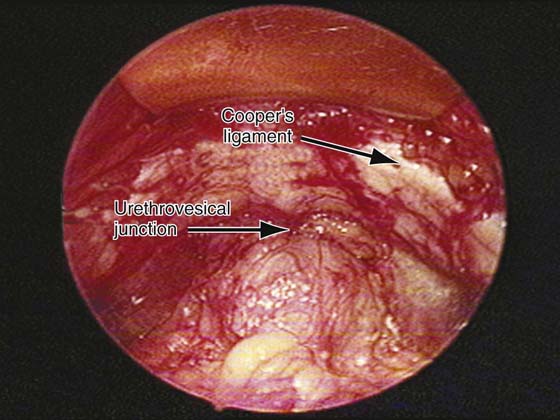
FIGURE 32–5 A view of the completely dissected retropubic space. A large Foley balloon facilitates this dissection, which can easily be done bluntly in the patient who has not had any previous retropubic procedures. Ideally, the dissection should be done down to the level of the urethrovesical junction at the midline and to the level of the arcus tendineus fasciae pelvis on each side.