W1 Role of Advanced Imaging in Distal Radius Fractures
Distal radius fractures are the most common upper limb fractures and account for approximately one sixth of all fractures treated in emergency departments. These fractures are associated with significant patient morbidity1,2 and result in major economic impact, with loss of industrial manpower.3 Accurate assessment followed by appropriate management of these fractures is vital for optimizing function of the wrist and hand.
Conventional radiography is usually sufficient to diagnose simple and uncomplicated distal radius fractures. This modality is limited, however, by problems with patient discomfort, which cause degradation of image quality because of subsequent motion and loss of osseous detail owing to superimposition.4–6 The reliability of radiography is diminished in the evaluation of complex fractures and is inherently inferior to advanced cross-sectional imaging techniques, such as computed tomography (CT) and magnetic resonance imaging (MRI).
A greater understanding of the importance of accurate presurgical fracture characterization and follow-up has led to an increasing reliance on CT and, to a lesser extent, MRI. In particular, the advent of multidetector CT (MDCT) has ensured that CT remains the gold standard in the imaging of distal radial fractures, particularly in clinical scenarios where plain radiographs yield insufficient information.
A single set of axial images acquired from an MDCT scanner has the capability of providing multiplanar reformatted images in the sagittal and coronal planes, offering superb cortical and trabecular bone resolution and accurate fracture characterization. MDCT also allows for rapid image acquisition times, minimizing motion artifact. The configuration of the fracture fragments involving the distal radial articular surface may be directly visualized, as may the degree of diastasis of the radioscaphoid and radiolunate fossae fragments, degree of articular incongruity, and possible ventral or dorsal cortical comminution. The sagittal and coronal planes are useful for showing the articular congruity and angulation, with step and gap deformity assessed in any of the three planes. The tendons may be assessed on soft tissue windows, allowing for their gross assessment. MDCT also allows for accurate postoperative fracture assessment because it effectively reduces beam hardening artifact resulting from metal to a minimum, a significant limitation of prior standard helical scanners.
MRI plays a specific role and is reserved for the assessment of concomitant soft tissue injuries, often suspected on presentation of ongoing postsurgical pain. MRI also may be used in circumstances where clinical suspicion for a fracture remains high, but radiographs and CT scans are negative. Technetium-99m MDP bone scintigraphy also may be used in similar circumstances, accurately identifying occult fractures and post-traumatic reflex sympathetic dystrophy.
Computed Tomography
CT is the modality of choice in characterizing the morphological characteristics of distal radius fractures. Unless the degree of fracture displacement on radiography is equivocal, simple displaced fractures traditionally do not require CT. CT is particularly useful, however, in the evaluation of complex comminuted distal radius fractures, serving as a preoperative road map in patients who have been selected for open reduction and internal fixation. CT also has an important role in the diagnosis of occult fractures, and is invaluable in postfracture healing assessment and in the evaluation of the postsurgical wrist, effectively excluding many potential complications.
Although several parameters have an impact on postfracture functional outcome, after correcting for severity of the initial fracture of the distal radius, the degree of intra-articular step and gap deformity correlates most strongly with prognosis, whereas this is not the case with dorsal and radial tilt.7 Fractures that heal with radiocarpal or distal radioulnar joint (DRUJ) step or gap deformities greater than 1 to 2 mm strongly correlate with premature arthrosis shown on radiographs.7–10 Conversely, almost all patients achieve an excellent result with less than 1 mm of articular incongruity.8 This finding has been supported by animal models of articular fractures, where cartilage remodeling provides a congruent articular surface when displacement is less than 1 mm, whereas a step-off of greater than 1 mm typically does not.11
CT scanning has been shown to be the most reliable method for identifying the extension of distal radial fractures to involve the articular surface, and accurately quantifies the degree of articular surface incongruity (Fig. W1-1).12–15 CT reliably distinguishes between patients for whom surgery is indicated, preventing accelerated osteoarthritis in this group, from patients in whom only a conservative approach is required. Comparative studies between plain radiographs and CT scans not only reveal CT to be accurate at measuring the step and gap deformity, but also show that plain radiographs are 30% more likely to overestimate or underestimate displacement compared with CT.11 CT is of particular benefit in evaluating the injured wrist in the presence of a plaster cast16 because osseous detail is not obscured to the same extent as it is with radiography. Accurate postreduction assessment for residual angulation and displacement is possible. The degree of comminution and size of fragments also are important considerations when assessing distal radial fractures, in planning management and predicting long-term outcome. CT accurately quantifies comminuted fragments and their size.16,17
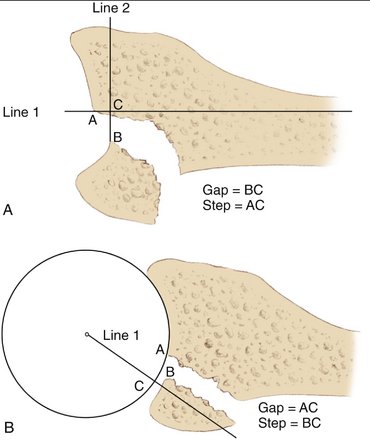
FIGURE W1-1 Method for assessing intra-articular gap and step deformity. The degree of intra-articular step deformity is represented by a line connecting points A and C on the longitudinal reformatted image (A) and line BC and the coronal image (B). The degree of gap deformity is defined as line BC (A) and line AC (B), respectively. CT allows for improved visualization of the fracture fragments compared with plain radiographs, as seen in the sagittal reformatted image (C).
Involvement of the DRUJ in distal radius fractures is similarly underestimated on radiographs compared with CT.13,14 Sigmoid notch fracture step-off and articular gapping also are assessed with a greater degree of accuracy with CT.18 Subluxation or dislocation of the DRUJ with distal radius fractures may be overlooked. On a posteroanterior radiograph, the DRUJ space should measure approximately 2 mm; however, even a small degree of supination or pronation of the wrist from the neutral position renders analysis of the DRUJ on plain film inaccurate.18,19 This limitation of patient positioning is overcome with CT scanning, which is the modality of choice in assessing the DRUJ. Apart from assessing fracture extension into the joint space, static and dynamic DRUJ instability can be assessed by obtaining CT images of the wrist in various positions of forearm rotation.20
Postfracture assessment of the distal radius, including postsurgical change and complications, is improved with CT versus plain radiography owing to the avoidance of overlapping bone surfaces and plaster casts.17 This includes improved evaluation of bone bridging and graft incorporation.20 The position of metal fixation devices, even when artifact is present, also is more accurately evaluated with CT, particularly with MDCT. Malunited distal radius fractures may be complicated by intra-articular incongruity and ulnar-positive variance, findings easily assessed with MDCT. Patients requiring additional treatment usually are managed with corrective wedge osteotomy and placement of an autogenous bone graft.21 MDCT with three-dimensional surface rendered images is increasingly used not only for appreciation of malunion, but also as a road map for surgery (Fig. W1-2). CT virtual preoperative planning, including virtual osteotomy of the distal radius, prediction of final positioning, and computer-assisted manufacturing of repositioning devices, has shown promising results for guiding surgical management.22,23

FIGURE W1-2 Anterior volume-rendered 3D reformatted image from a multidetector CT examination allows improved appreciation of the degree of fracture displacement of the distal radius, allowing the clinician to anticipate surgical findings.
Frequently, subtle radiographic lucencies of the distal radius may simulate fractures and are a cause for inconclusive, or even incorrect, reporting. Similarly, occult fractures of the wrist are sometimes suspected on the basis of physical examination or focal areas of increased scintigraphic uptake on bone scintigrams, despite normal plain films. CT has the capability of providing additional specificity to these findings, particularly with the use of three-dimensional reconstructions.20,24,25
Limited interobserver reliability has been observed with most fracture classification systems,12,13,26 including the classification systems of the distal radius. More recent literature has aimed at assessing the potential added value of three-dimensional CT reconstructions over conventional two-dimensional CT for distal radial fracture classification. Although these studies reveal improved intraobserver agreement on fracture classification, conflicting data surround the added benefit on interobserver reliability.27,28
Despite the numerous benefits, CT scanning in the assessment of distal radius fractures is not without its limitations. Metal artifact, which is not observed with conventional plain film, remains a major factor with helical CT, but is no longer an issue with most modern MDCT systems (Fig. W1-3). Direct assessment of articular cartilage requires intra-articular contrast injection, whereas soft tissue contrast is poor. Increased cost associated with CT compared with plain radiography is well recognized, with three-dimensional imaging increasing technician time.27,28 Although the effective radiation dose is limited when scanning the extremities, this always warrants consideration, particularly when a multidetector scanner is used in younger patients.

FIGURE W1-3 Sagittal reformatted image from a multidetector CT examination demonstrates the relative decrease in beam hardening artifact due to metallic hardware. This advantage of CT allows for accurate post-operative assessment of the degree of fracture healing and reliably excludes complications such as loosening.
Magnetic Resonance Imaging
Although CT is conventionally used to supplement plain film evaluation of distal radius fractures, the value of MRI in assessing associated soft tissue injuries is becoming increasingly recognized. Although osseous congruity is the most important factor in determining outcome, soft tissue injury is a significant contributor to long-term morbidity. It has been reported that grip strength averages only 69% and wrist movement 75% that of the uninjured opposite hand, despite accurate restoration of skeletal integrity after an intra-articular distal radius fracture.29 This finding has been further supported arthroscopically, confirming that 68% of patients with displaced intra-articular fractures had associated soft tissue injuries.30 MRI plays its primary role in the early and accurate diagnosis of these injuries. MRI also may detect fractures, particularly in cases of subtle trabecular disruption and intra-articular extension, which may not be visualized radiographically,31 and occasionally may be occult on CT.
Ulnocarpal impaction syndrome is a common MRI finding after a distal radius fracture.24,25,32 In the normal joint, approximately 80% of mechanical forces are transmitted across the radius, and 20% are transmitted across the ulna. A change of only 1 mm of relative ulnar-positive variance owing to radial shortening alters the load distribution through the ulnocarpal joint by more than 25%.33 This alteration ultimately results in triangular fibrocartilage complex (TFCC) degeneration and tearing, and chondromalacia of the distal ulna head and lunate.34,35 Early findings of ulnocarpal impaction on plain radiographs are typically negative or subtle.36 Changes such as sclerosis, demineralization, and cyst formation in the distal ulna and proximal ulnar aspect of the lunate are seen radiographically only in the later stages of the condition.37 On MRI, the presence of bone marrow edema of the lunate is a reliable finding.24,25,32 As opposed to fracture-related edema, which is readily seen on MRI and shows healing within 8 weeks, these patients show persisting or increasing marrow edema within the lunate beyond this period.24
Of the numerous soft tissue injuries associated with distal radius fractures, scapholunate ligament injuries are of particular significance. The scapholunate ligament and the lunotriquetral ligament are two intrinsic ligaments of the wrist that are critical to wrist stability. Complete scapholunate ligament tears are usually associated with fractures through the junction of the scaphoid and lunate articular facets of the distal radius. On plain radiographs, injury to either of these ligaments is assumed indirectly by the presence of a widened scapholunate (or lunotriquetral) interspace of 4 mm or greater, volar tilt of the scaphoid, and dorsal tilt of the lunate. In particular, tears of the larger scapholunate ligament may be confirmed with direct visualization on MRI as discrete fiber disruption with high sensitivity and specifity.31,34,35 Complete lunotriquetral ligament tears are more difficult to confirm with MRI,34,35 as are partial tears of both ligaments.36
Distal radius fractures are commonly associated with TFCC injuries. MRI is particularly useful at diagnosing these injuries, with reported detection rates of 45% to 66%.37,38 The TFCC is best seen on coronal images, appearing as a bowtie structure, whereas the supporting volar and dorsal bands of the radioulnar ligament are ideally seen in the axial plane.39 Plain radiographs are not helpful in the evaluation of TFCC injuries, unless there is marked diastasis or dislocation of the DRUJ. Studies comparing MRI with wrist arthrography and arthroscopy have shown high sensitivity and specificity in predicting TFCC tears, but poorer accuracy in defining tear location.40,41 Apart from direct injury at the time of fracture, increased mechanical load on the ulnocarpal joint caused by postfracture ulnar-positive variance also leads to the delayed development of TFCC lesions.42
Tendon injuries, including rupture (Fig. W1-4) and entrapment (Fig. W1-5), are another well-recognized complication after distal radius fractures, with extensor pollicis longus tendon rupture commonly seen with Colles’ fractures.1 This tendon rupture also can be seen in non-Colles’ fracture of the distal radius, where the fracture extends to Lister’s tubercle and may cause the extensor pollicis longus to rupture acutely. This injury is usually recognized at the time of fracture because of reduced function of the thumb; however, clinical examination in the setting of an acute fracture may be unreliable.43 Direct visualization with MRI allows for the accurate assessment of tendon integrity. Complete tendon rupture manifests as loss of continuity of the homogeneously low signal intensity of a normal tendon. More subtle incomplete ruptures or chronic tears may manifest as irregular thinning or thickening of the tendon as areas of increased signal intensity on fluid-weighted sequences. MRI also provides useful information for planning of the tendon repair, particularly the degree and level of retraction. Postoperatively, low signal adhesions and scar tissue around a tendon, which can result in ongoing functional impairment,44 also may be detected, as may stenosing tenosynovitis.
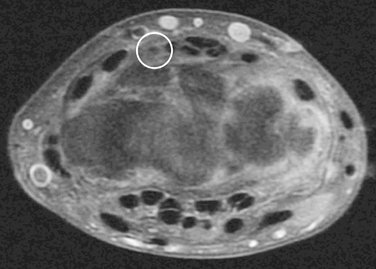
FIGURE W1-4 Coronal T2 fat-saturated MR image through the wrist demonstrates the most distal extent of a full-thickness tear of the extensor pollicis longus tendon (circle), retracted proximal to Lister’s tubercle.
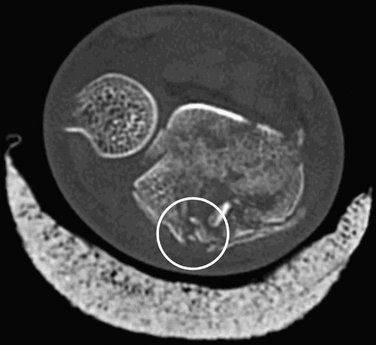
FIGURE W1-5 Coronal reformatted image from a multidetector CT examination demonstrates extension of a distal radius fracture posteriorly to Lister’s tubercle, resulting in encasement and the clinical findings of entrapment of the extensor pollicis longus tendon (circle).
In a skeletally immature patient, fractures involving the epiphyseal growth plate can result in bony bridge formation during healing. These physeal bridges can result in growth retardation or arrest, potentially causing limb-length discrepancies or angular deformities.45 The size and location of the bone bar are important in deciding operative management and prognosis.46,47 Accurate interpretation of plain films is often difficult, especially because the irregular three-dimensional nature of the physis limits the interpretation of two-dimensional planar images.48 MRI easily distinguishes between the hypointense signal of a bone bridge from the hyperintense (cartilage) signal of the normal growth plate. Apart from the ossified bridges, this technique also allows for the detection of nonossified bridges that are not seen on CT, especially with the use of fat-suppressed three-dimensional spoiled gradient-recalled echo imaging.49,50
Limitations of MRI include the lack of cortical osseous detail, which is surpassed by CT; the latter modality allows for improved fracture characterization. Artifact from metallic internal fixation devices, in the form of blooming artifact, can significantly distort image acquisition. Lengthy scanning times, lack of availability, and increased cost compared with CT and plain radiography limit the regular use of MRI as a routine modality for radius fracture assessment.
Nuclear Medicine
Radionuclide bone scans play a limited role in the evaluation of a patient with a suspected acute distal radius fracture. Scintigraphy may be used where a lucency of the distal radius is equivocal, possibly representing either a fracture or a normal finding, such as a vascular channel. Bone scans also may be used by the clinician after trauma when initial plain films are normal. Intense focal tracer uptake on delayed images in the context of trauma is consistent with an occult fracture. Mildly increased focal uptake on the earlier (blood pool) phases is suspicious for soft tissue injury (ligamentous or cartilaginous). The presence of a positive bone scan correlates highly with the presence of a fracture on conventional modalities51; however, bone scintigraphy has poor anatomical localization, and a positive result warrants further advanced imaging with CT or MRI. A scan with negative scintigraphic uptake reliably excludes the presence of an acute bone abnormality.51
Reflex sympathetic dystrophy is a post-traumatic condition caused by alteration in the sympathetic nervous system, resulting in regional hyperemia, secondary osteoporosis, soft tissue atrophic changes, and altered temperature control. This condition is a well-recognized complication of distal radius fractures. Reflex sympathetic dystrophy is diagnosed with high sensitivity and specificity using bone scintigraphy,52 manifesting as diffuse increased activity in a periarticular distribution on the delayed images.
Conclusion
Although plain radiographs are the initial modality for the diagnosis of fracture of the distal radius, CT may provide further reliable fracture characterization. In particular, MDCT with its multiplanar capability is the gold standard for assessing the main determinants of patient outcome—the degree of intra-articular step and gap deformity. MRI may show similar findings and associated soft tissue injuries of the intrinsic wrist ligaments, TFCC, and flexor and extensor tendons.
1. Cooney WPIII, Dobyns JH, Linschield RL. Complications of Colles’ fractures. J Bone Joint Surg. 1980;62:613-618.
2. Field J, Warwick D, Bannister GC, et al. Long-term prognosis of displaced Colles’ fracture: a 10-year prospective review. Injury. 1992;23:529-532.
3. Palmer AK. The distal radioulnar joint. In: Lichtman DM, editor. The Wrist and Its Disorders. Philadelphia: WB Saunders, 1988.
4. Quinn SF, Murray W, Watkins T, et al. CT for determining the results of treatment of fractures. AJR Am J Roentgenol. 1987;149:109-111.
5. Muren C, Nygren E, Svartengren G. Computed tomography of the scaphoid in the longitudinal axis of the bone. Acta Radiol. 1990;31:110-111.
6. Friedman L, Yong-hing K, Johnston GH. Forty degree angled coronal CT scanning of scaphoid fractures through plaster and fiberglass casts. J Comput Assist Tomogr. 1989;3:1101-1104.
7. Trumble TE, Schmitt SR, Vedder NB. Factors affecting functional outcomes in displaced intra-articular distal radius fractures. J Hand Surg. 1994;19:325-340.
8. Fernandez DL, Geissler WB. Treatment of displaced articular fractures of the radius. J Hand Surg. 1991;16:375-384.
9. Bradway JK, Amadio PC, Cooney WP. Open reduction and internal fixation of displaced comminuted fractures of the distal end of the radius. J Bone Joint Surg. 1989;71(6):839-847.
10. Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg. 1986;68:647-659.
11. Llinas A, Mckellop HA, Marshall GJ, et al. Healing and remodeling of articular fractures incongruities in a rabbit fracture model. J Bone Joint Surg. 1993;75:1508-1523.
12. Cole RJ, Bindra RR, Evanoff BA, et al. Radiographic evaluation of osseous displacement following intra-articular fractures of the distal radius: reliability of plain radiograph versus computed tomography. J Hand Surg [Am]. 1997;22:792-800.
13. Katz MA, Beredjikilian PK, Vresilovic EJ, et al. Computer tomographic scanning of cervical spine fractures: does it influence treatment? J Orthop Trauma. 1999;13:338-343.
14. Pruitt DL, Gilula LA, Manske PR, et al. Computer tomography scanning with image reconstruction in evaluation of distal radius fractures. J Hand Surg [Am]. 1994;19:720-727.
15. Johnston GH, Friedman L, Kriegler JC. Computerized tomographic evaluation of acute distal radius fractures. J Hand Surg [Am]. 1992;17:738-744.
16. Metz VM, Gilula LA. Imaging techniques of distal radius fractures and related injuries. Orthop Clin North Am. 1993;24:217-228.
17. Mino DE, Palmer AK, Levinsohn EM. The role of radiography and computed tomography in the diagnosis of incongruity of the distal radio-ulnar joint: A prospective study. J Hand Surg. 1983;8:23-31.
18. Frahm R, Saul O, Drescher E. CT Diagnostik bei fehlstellung nach distaler Radiusfracktur. Radiologe. 1989;29:68.
19. Rozental TD, Beredjiklian PK, Bozentka DJ. Instability of the distal radioulnar joint: current diagnosis and treatment methods. Curr Opin Orthop. 2003;14:245-251.
20. Nakamura R, Horii E, Tanaka Y, et al. Three dimensional CT imaging for wrist disorders. J Hand Surg. 1989;14:53-58.
21. Melendez EM. Opening-wedge osteotomy, bone graft and external fixation for correction of radius malunion. J Hand Surg. 1997;22:785-791.
22. Athwal GS, Ellis RE, Small CF, et al. Computer assisted osteotomy. J Hand Surg. 2003;28:951-958.
23. Reiger M, Gabl M, Gruber H, et al. CT virtual reality in the preoperative workup of malunited distal radius fractures: preliminary results. Eur Radiol. 2005;15:792-797.
24. Wainwright AM, Williams JR, Carr AJ. Interobserver and intraobserver variation in classification systems for fractures of the distal humerus. J Bone Joint Surg Br. 2000;82:625-626.
25. Doornberg J, Lindenhovius A, Kloen P, et al. Two and three-dimensional computed tomography for the classification and management of distal humerus fractures: evaluation of reliability and diagnostic accuracy. J Bone Joint Surg Am. 2006;88:1795-1801.
26. Harness NG, Ring D, Zurakowski D, et al. The influence of three-dimensional computed tomography reconstructions on the characterization and treatment of distal radial fractures. J Bone Joint Surg Am. 2006;88:1315-1323.
27. Trumble TE, Schmitt SR, Vedder NB. Factors affecting functional outcome of displaced intra-articular distal radius fractures. J Hand Surg [Am]. 1994;19:325-340.
28. Geissler WB, Freeland AE, Savoie FH, et al. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg [Am]. 1996;78:357-364.
29. Spence L, Savenor A, Nwachuku I, et al. MRI of fractures of the distal radius: comparison with conventional radiographs. Skeletal Radiol. 1998;27:244-249.
30. Steinborn M, Schürmann M, Staebler A, et al. MRI imaging of ulnocarpal impaction after fracture of the distal radius. AJR Am J Roentgenol. 2003;181:195-198.
31. Escobedo EM, Bergman AG, Hunter JC. MR imaging of ulnar impaction. Skeletal Radiol. 1995;24:85-90.
32. Imaeda T, Nakamura R, Shionoya K, et al. Ulnar impaction syndrome: MR imaging findings. Radiology. 1996;201:495-500.
33. Palmer A, Werner F. Biomechanics of the distal radioulnar joint. Clin Orthop. 1984;187:26-35.
34. Palmer AK. Triangular fibrocartilage lesions: a classification. J Hand Surg [Am]. 1989;14:594-606.
35. Palmer AK. Triangular fibrocartilage disorders: injury patterns and treatment. Arthroscopy. 1990;6:125-132.
36. Cerezal L, del Pinal F, Abascal F, et al. Imaging findings in ulnar sided wrist impaction syndromes. RadioGraphics. 2002;22:105-121.
37. Uchiya S, Terayam K. Radiographic changes in wrists with ulnar plus variance observed over a ten-year period. J Hand Surg [Am]. 1991;16:45-48.
38. Schweitzer ME, Brahme SK, Hodler J, et al. Chronic wrist pain: spin-echo and short TR inversion recovery MR imaging and conventional and MR arthrography. Radiology. 1992;182:205-211.
39. Zlatkin MB, Chao PC, Osterman AL, et al. Chronic wrist pain: evaluation with high resolution MR imaging. Radiology. 1989;173:723-729.
40. Manton GL, Schweitzer ME, Weishaupt D, et al. Partial ligamentous tears of the wrist: difficulty in utilizing either primary or secondary MRI signs. J Comput Assist Tomogr. 2001;25:671-676.
41. Fontes D, Lenoble E, De Somer B, et al. Lesions ligamentaires associees aux fractures distales du radius: à propos de cinquante-huit arthrographies peroperatoires. Ann Chir Main. 1992;11:119-125.
42. Mohanti RC, Kar N. Study of triangular fibrocartilage of the wrist in Colles’ fracture. Injury. 1980;11:321-324.
43. Steinbach LS, Smith DK. MRI of the wrist. Clin Imaging. 2000;24:298-322.
44. Potter HG, Asnis-Ernberg L, Weiland AJ, et al. The utility of high-resolution magnetic resonance imaging in the evaluation of the triangular fibrocartilage complex of the wrist. J Bone Joint Surg Am. 1997;79:1675-1684.
45. Blazer PE, Chan PS, Kneeland JB, et al. The effect of observer experience on magnetic resonance imaging interpretation and localization of triangular fibrocartilage complex lesions. J Hand Surg [Am]. 2001;26:742-748.
46. Palmer AK. Triangular fibrocartilage disorders: injury patterns and treatment. Arthroscopy. 1990;6:125-132.
47. Kumar A, Kelly C. Extensor pollicis longus entrapment after Smith’s fracture. Injury Int J Care Injured. 2003;34:75-78.
48. Beltram J, Mosure JC. Magnetic resonance imaging of tendons. Crit Rev Diag Imaging. 1990;30:111-182.
49. Ogden JA. The evaluation and treatment of partial physeal arrest. J Bone Joint Surg Am. 1987;69:1297-1301.
50. Peterson HA. Partial growth plate arrest and its treatment. J Pediatr Orthop. 1984;4:246-258.
51. Williamson RV, Staheli LT. Partial physeal growth arrest: treatment by bridge resection and fat interposition. J Pediatr Orthop. 1990;10:769-776.
52. Sailham F, Chotel F, Guibal AL, et al. Three dimensional MR imaging in the assessment of physeal growth arrest. Eur Radiol. 2004;14:1600-1608.