Oedema
Oedema is the accumulation of excessive fluid in the subcutaneous tissue. When oedema results from lymphatic stasis, the term lymphoedema is used. Oedema may be pitting or non-pitting. Subcutaneous oedema is referred to as pitting when, after pressure is applied to a small area, the indentation persists for some time after release of the pressure (Fig. 49). Pitting oedema is caused by either systemic diseases (generalised) or local conditions involving just the affected extremities. The most common systemic diseases involve the heart, liver and kidneys. In these diseases, oedema occurs primarily because of water retention or fluid leaking into the interstitial spaces. The most common local conditions that cause oedema involve venous obstruction, e.g. varicose veins, DVT. Non-pitting oedema is observed when the indentation does not persist, e.g. lymphoedema, myxoedema.
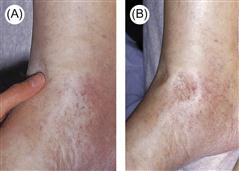
Figure 49 (A,B) Pitting oedema in a patient with cardiac failure.
A depression (‘pit’) remains in the oedema for some minutes after firm fingertip pressure is applied.
History
Site and distribution
Enquiries should be made regarding the site of oedema, as localised and demarcated sites of oedema are usually due to trauma or infection. Oedema may be confined to both lower limbs, for example with IVC obstruction and pregnancy, or affect only a single limb, such as the leg with unilateral DVT or arm following axillary lymph node clearance.
Precipitating factors
Precipitating factors such as trauma and infection may be obvious from the history, and should be excluded. Angio-oedema may be precipitated by a known allergen. Lymphoedema may result as a complication of infection with filarial nematodes while travelling in endemic areas such as Africa, Asia and Australia. Lymphoedema may also be congenital, occurring shortly after birth (Milroy’s disease) or at puberty (lymphoedema praecox) or in the third decade (lymphoedema tarda).
Past medical and drug history
Interruption to lymphatic drainage may result as a complication of irradiation or surgery, especially in the region of the axilla and groin. Obstruction of lymphatic flow can also result from direct involvement of the lymph nodes by lymphoma, or secondary to metastatic lymphatic infiltration from tumours. A detailed drug history will identify any offending drug.
Associated symptoms
If there is no obvious precipitating factor in the history, then specific enquiries should be undertaken for each system. Symptoms suggestive of malignancy, in particular, should be sought. In addition, it is important to exclude the following conditions.
Cardiac failure
Lethargy, dyspnoea, orthopnoea, paroxysmal nocturnal dyspnoea, cough, ankle oedema and abdominal distension from ascites may be some symptoms experienced by patients with cardiac failure.
Liver disease
Symptoms of jaundice, pruritus, ankle oedema, abdominal distension, haematemesis and confusion (encephalopathy) should be sought to determine the presence of liver disease.
Renal disease – nephrotic syndrome
Severe generalised oedema is the prominent feature with nephrotic syndrome. Patients may also complain of frothy urine due to proteinuria.
Malabsorption
Weight loss, diarrhoea and steatorrhoea may be some of the features associated with malabsorption.
Venous thrombosis
Unilateral leg swelling and pain are the main symptoms of DVT. Occasionally with iliofemoral vein thrombosis, the entire leg may appear blue (phlegmasia cerulea dolens) or white (phlegmasia alba dolens). Bilateral leg oedema with the onset of dilated superficial collateral veins on the trunk and abdomen is suggestive of IVC obstruction.
Examination
Inspection
Assessment of the distribution of oedema may narrow the differential diagnosis. Generalised causes tend to present with dependent oedema, with fluid accumulating in the ankles in ambulant patients and the sacrum in recumbent patients.
Cardiovascular system
With cardiac failure, palpation of the pulse may reveal tachycardia with pulsus alternans. The measured blood pressure may be low due to systolic failure. The JVP is elevated and a third heart sound with bilateral coarse pulmonary crepitations may be auscultated. Hepatomegaly due to liver congestion and ascites may also be present.
Abdominal examination
Generalised wasting from malabsorption or malignancy may be appreciated on inspection. Clubbing, palmar erythema, Dupuytren’s contracture, jaundice, spider naevi and gynaecomastia are signs of liver disease. Dilated collateral veins on the abdomen may be due to portal hypertension or IVC obstruction; therefore, determine the direction of blood flow. Below the umbilicus, the direction of blood flow is inferior with portal hypertension, and superior with IVC obstruction. Organomegaly due to carcinoma may be present and predispose to venous thrombosis. Pelvic malignancy may also result in venous outflow obstruction.
Legs
Check if the oedema is pitting or non-pitting. The legs are examined for the presence of tenderness and swelling. Circumferences of both the thighs and calves are compared. Marked painful erythematous unilateral swelling may be indicative of a DVT.
General Investigations
Specific Investigations
■ 24-hour urine collection
>3.5 g of protein with nephrotic syndrome.
■ Renal biopsy
To determine the cause of nephrotic syndrome in adults.
■ Echocardiography
Ventricular dilatation and impaired function with cardiac failure.
■ Liver biopsy
Liver cirrhosis.
■ Faecal fat estimation
↑ malabsorption.
■ Duplex Doppler deep veins of the leg
DVT of the leg.
■ Venography
Below-knee DVT, IVC obstruction.




