23 Ocular motor nerves
The Nerves
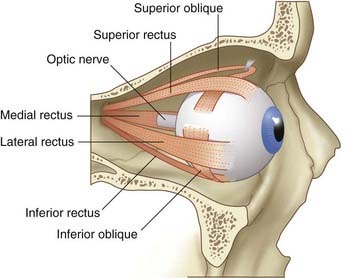
The ocular motor nerves comprise the oculomotor (III cranial), trochlear (IV cranial), and abducens (VI cranial) nerves. They provide the motor nerve supply to the four recti and two oblique muscles controlling movements of the eyeball on each side (Figure 23.1). The oculomotor nerve contains two additional sets of neurons: one to supply the levator of the upper eyelid, the other to control the sphincter of the pupil and the ciliary muscle.
Oculomotor nerve
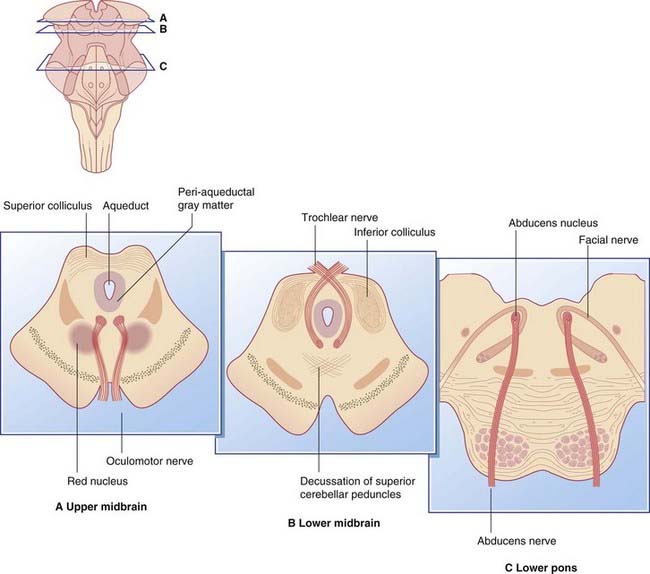
The nucleus of the third nerve is at the level of the superior colliculus. It is partly embedded in the peri-aqueductal gray matter (Figure 23.2A). It is composed of five individual nuclei for the supply of striated muscles, and one parasympathetic nucleus.
Trochlear nerve
The nucleus of the fourth nerve is at the level of the inferior colliculus. The nerve itself is unique in two respects (Figure 23.2B): it is the only nerve to emerge from the back of the brainstem; and it decussates with its opposite number.
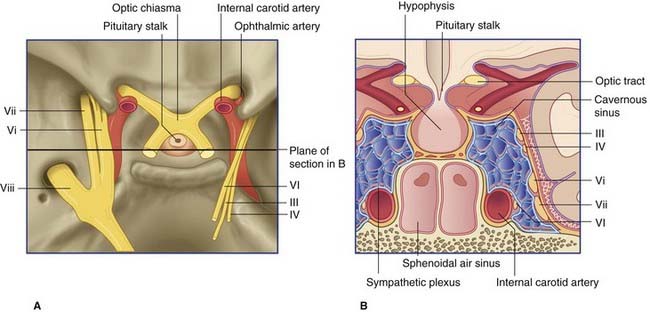
The IV nerve winds around the crus of the midbrain and travels through the cavernous sinus in company with the III nerve (Figure 23.3). It passes through the superior orbital fissure and supplies the superior oblique muscle.
Abducens nerve
The nucleus of the sixth nerve, in the floor of the fourth ventricle, is at the level of the facial colliculus, in the lower pons (Figure 23.2C). The nerve descends, to emerge at the lower border of the pons, and runs up the pontine subarachnoid cistern beside the basilar artery. It angles over the apex of the petrous temporal bone and passes through the cavernous sinus beside the internal carotid artery (Figure 23.3). It enters the orbit through the superior orbital fissure and supplies the lateral rectus muscle, which abducts the eye.
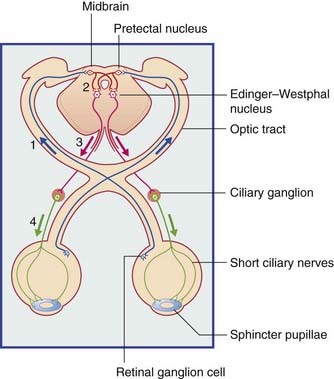
Pupillary Light Reflex (Figure 23.4)
Constriction of the pupils in response to light involves four sets of neurons, as follows:
Accommodation
The near response
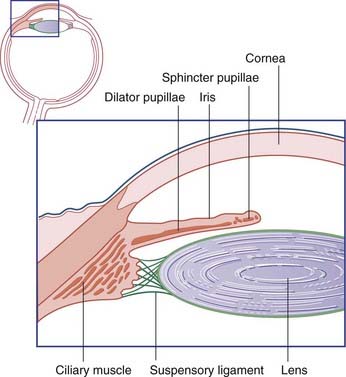
When the eyes view an object close up, the ciliary muscle contracts reflexly, thereby relaxing the suspensory ligament of the lens (Figure 23.5). Since the lens at rest is somewhat compressed (flattened) by tension exerted on the lens capsule by the suspensory ligament, the lens bulges passively when the ciliary muscle contracts. The thicker lens has the greater refractive power required to bring close-up objects into focus on the retina. The response of the lens is one of accommodation.
The three features described are also known as the near response.
Notes on the Sympathetic Pathway to the Eye
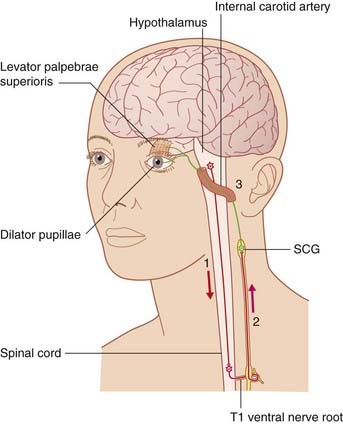
The great length of the sympathetic pathway to the eye is indicated in Figure 23.6.
Interruption of the postganglionic fibers at the jugular foramen (see jugular foramen syndrome, Ch. 18), or in the cavernous sinus, produces anhidrosis (loss of sweating) on the forehead and scalp.
Ocular Palsies
The effects of paralysis of the motor nerves to the eye are described in Clinical Panel 23.1.
Clinical Panel 23.1 Ocular palsies
Oculomotor nerve
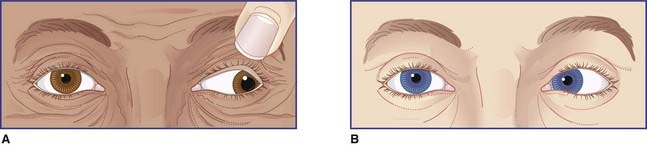
Complete III nerve palsy
Characteristic signs of complete third nerve paralysis are shown in Figure CP 23.1.1A. They are:
Partial III nerve palsy
The pupils are always monitored when cases of head injury come to medical attention. Rapidly increasing intracranial pressure, resulting from an acute extradural or subdural hematoma (Ch. 4), often compresses the third nerve against the crest of the petrous temporal bone. The parasympathetic fibers are superficially placed and are the first to suffer, and the pupil dilates progressively on the affected side. Pupillary dilatation is an urgent indication for surgical decompression of the brain.
Abducens nerve
The effect of a complete VI nerve paralysis is shown in Figure CP 23.1.1B. The eye is fully adducted by the unopposed pull of the medial rectus.
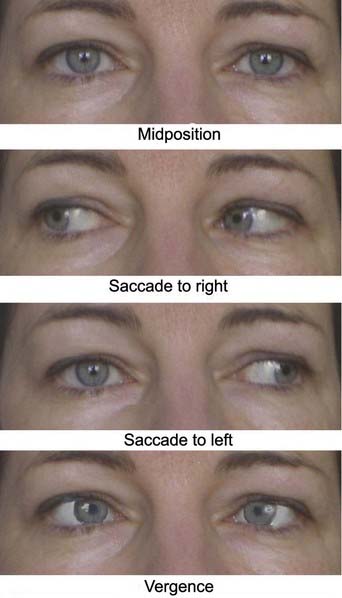
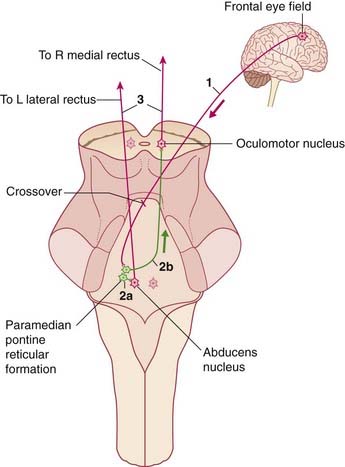
Internuclear ophthalmoplegia (Figure CP 23.1.2)
Interruption of the linkage between the abducens nucleus and the contralateral oculomotor nucleus gives rise to the condition known as internuclear ophthalmoplegia. As an example, a lesion of the VI–III connection shown in Figure 23.7 would leave a saccade to the right unaffected, whereas on attempting a saccade to the left, the paralyzed right medial rectus would create a divergent strabismus with accompanying diplopia. Integrity of the nucleus serving the right medial rectus is shown by its normal behavior during the vergence component of the near response.
Ocular sympathetic supply
Any one of the three sequential sets of neurons depicted in Figure 23.6 may be interrupted by local pathology.
Control of Eye Movements
Scanning
The paired centers (left and right) for horizontal saccades are in the paramedian pontine reticular formation (PPRF) (Figure 17.15). Each pulls the eyes to its own side (Figure 23.7). The midbrain contains a bilateral center for upward saccades located in the rostral end of the medial longitudinal fasciculus (MLF), at the level of the pretectal nucleus. It is called the rostral interstitial nucleus (riMLF). At the same level but a little ventral to this is a bilateral center for downward gaze (Figure 17.19).
Voluntary scanning movements are initiated in the frontal eye fields, located at the junction of motor and premotor cortex (Ch. 29). From each frontal eye field, a projection descends in the anterior limb of the internal capsule. Most of the fibers cross over before terminating in the gaze centers.
As explained in Chapter 29, the ipsilateral superior colliculus is activated at the same time, to reinforce the excitation of the appropriate gaze center.
The best-known afferents to the frontal eye field come from the parietal cortex, from cells concerned with visual attention. In monkeys, some cells in the posterior parietal cortex become active when an object of interest is seen. These cells project to the frontal eye field and are thought to facilitate eye movement in the direction of the object. In humans, neglect of the contralateral visual field is a well-known feature of damage to the posterior parietal lobe, especially on the right side (Ch. 32).
Tracking
The dynamic labyrinth and cerebellum cooperate to keep the eyes on target during movement of the head, as described in Chapter 19.
Brazis PW. Isolated palsies of cranial nerves III, IV, and VI. Semin Neurol. 2009;29:14-28.
Buttner-Ennever JA. Anatomy of the oculomotor system. Dev Ophthalmol. 2007;40:1-14.
Karatas M. Internuclear and supranuclear disorders of eye movements: clinical features and causes. Eur J Neurol. 16, 2009.
Keane JR. Internuclear ophthalmoplegia. Arch Neurol. 2005;62:714-717.
Miley JT, Rodriguez CJ, Hernandez EM, Bundlie SR. Teaching NeuroImage: traumatic internuclear ophthalmoplegia. Neurology. 2008;70:3-4.
Moschovakis AK. The neural integrators of the mammalian saccadic system. Front Biosci. 1997;15:D552-D557.
Papageorgiou E, Ticini LF, Hardiess G, Schaeffel F, Wiethoelter H, Mallot HA, Bahlo S, Wilhelm B, Fonthein R, Schiefer U, Karnath H-O. The pupillary light reflex pathway. Neurology. 2008;70:956-963.
Tilikete C, Pelisson D. Ocular motor syndromes of the brainstem and cerebellum. Curr Opin Neurol. 2008;21:22-28.
Wilhelm H. Neuro-ophthalmology of pupillary function. J Neurol. 1998;245:573-583.