42 Obturator Nerve Block
The obturator nerve arises from the lumbar plexus and innervates most of the adductors of the medial compartment of the thigh. The other adductors are the pectineus (innervated by the femoral nerve) and the adductor magnus (partially innervated by the sciatic nerve). The abundance of motor fibers makes the obturator nerve a frequent choice for electromyographic recording of compound motor action potentials (CMAPs).1
The cutaneous innervation by the obturator nerve is variable.2 However, there are morphine-sparing effects of obturator nerve block after major surgical procedures of the lower extremity. In blocks in which multiple lower extremity nerves are targeted (e.g., the posterior lumbar plexus block or the anterior 3-in-1 block), the obturator nerve has a relatively low block success rate. Therefore, obturator nerve block is an important adjunct for lower extremity analgesia. Other indications for obturator nerve block include relief of hip pain, treatment of adductor spasticity, and prevention of obturator stimulation during transurethral resection of lateral bladder wall tumors. Change in adduction strength is the best method for assessing obturator nerve block. However, even with complete obturator nerve block, there is some residual adduction strength because the pectineus (femoral nerve innervation) and the hamstring component of the adductor magnus (sciatic nerve innervation) muscles remain intact.
Suggested Technique
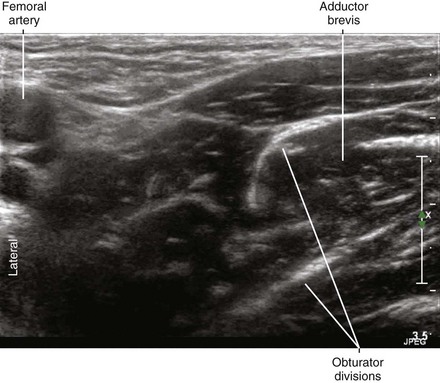
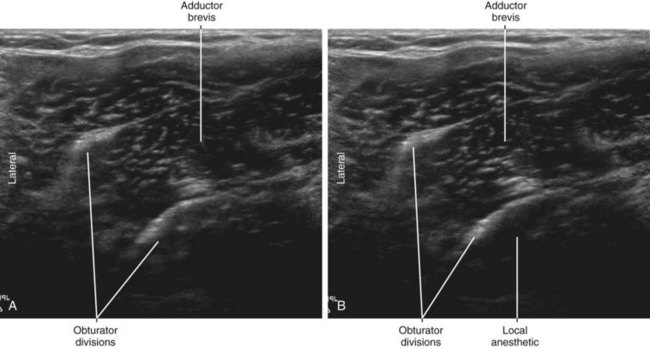
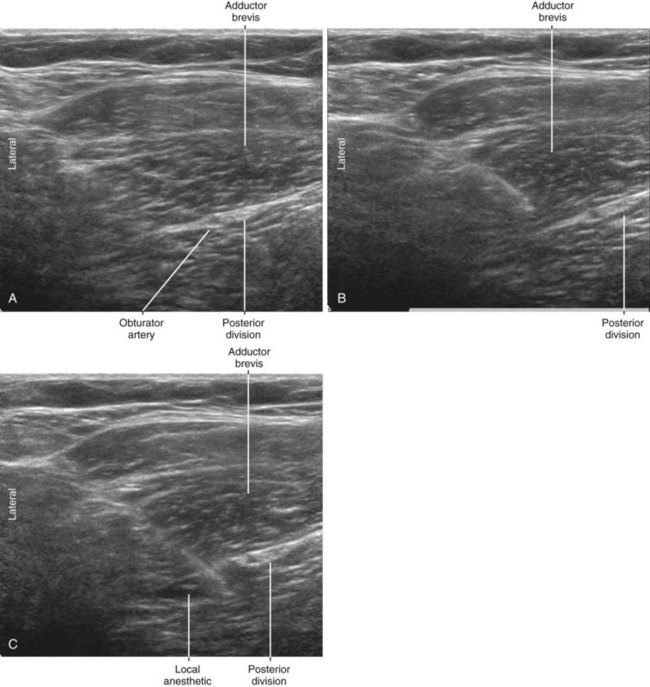
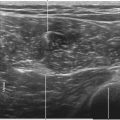
The anterior and posterior divisions of the obturator nerve converge proximally along the rounded lateral border of the adductor brevis muscle. The obturator nerve divisions are thin and flat as the fascicles disperse to the muscle groups. The obturator nerve divisions have a “white bands” appearance on sonography.3 It is important that the flat surfaces of the obturator nerve divisions are perpendicular to the sound beam to enhance their echo brightness. Note that although the anterior and posterior divisions converge along the lateral border of the adductor brevis, they do not actually meet there in most (75%-80%) subjects because the divisions remain separated by the obturator externus muscle proximally.4 Therefore, the obturator nerve block is usually performed as a multiple-injection technique targeting each of the two divisions separately.
The block is performed in supine position with the leg slightly abducted. The obturator divisions and adductor brevis are visualized in short-axis view in the medial thigh. This is best accomplished by sliding the transducer between proximal and distal locations to observe the convergence of the divisions along the lateral border of the adductor brevis. An out-of-plane approach is often used because of the proximity of the femoral vessels to the needle path for an in-plane approach. The block is usually performed where the anterior and posterior divisions are just separated by the adductor brevis, with the deeper posterior division targeted first. The local anesthetic distribution should be within the fascia that invests the adductor brevis and the obturator divisions. If the obturator nerve divisions cannot be visualized, a trans–adductor brevis injection can be performed. Care is taken to avoid puncture of the adjacent obturator arteries because puncture of these vessels can cause hemorrhage.5
Key Points
| Obturator Nerve Block | The Essentials |
|---|---|
| Anatomy | The ON divisions lie on the anterior and posterior sides of the adductor brevis muscle. The ON divisions are often accompanied by their respective arteries. |
| Image orientation | The ON divisions converge along the squared lateral edge of the adductor brevis muscle. |
| Positioning | Supine with leg slightly abducted |
| Operator | Standing on the side of the patient |
| Display | Across the table |
| Transducer | Medium- to high-frequency linear, 38- to 50-mm footprint |
| Initial depth setting | 40 to 50 mm (the posterior division of the obturator nerve lies at about twice the depth of the femoral nerve) |
| Needle | 20 to 21 gauge, 70 mm in length |
| Anatomic location | Begin by scanning the thigh medial to the femoral vessels. |
| Approach | SAX view of the ON divisions, in-plane from the lateral side Place the needle tip through the adductor brevis muscle and inject as the needle is slowly withdrawn. Local anesthetic should layer over posterior and anterior surfaces of the adductor brevis muscle. |
| Sonographic assessment | The injection should track along the ON divisions (SAX slide). |
| Anatomic variation | Relation of the ON divisions with obturator arteries is variable. ON divisions may be seen entering the adductor brevis muscle. |
Clinical Pearls
• An accessory obturator nerve is present in about 8.7% of subjects.6 When present, this nerve partially contributes to motor innervation of the pectineus.
• In some patients, branches entering the adductor brevis can be visualized, giving the appearance of three divisions to the obturator nerve. Position of the obturator arteries with respect to the obturator divisions is variable.

FIGURE 42-1 External photograph showing an out-of-plane approach to obturator nerve block in the medial thigh.

FIGURE 42-4 External photograph showing an in-plane approach to obturator nerve block in the medial thigh.
1 Atanassoff PG, Weiss BM, Brull SJ, et al. Compound motor action potential recording distinguishes differential onset of motor block of the obturator nerve in response to etidocaine or bupivacaine. Anesth Analg. 1996;82:317–320.
2 Bouaziz H, Vial F, Jochum D, et al. An evaluation of the cutaneous distribution after obturator nerve block. Anesth Analg. 2002;94:445–449.
3 Soong J, Schafhalter-Zoppoth I, Gray AT. Sonographic imaging of the obturator nerve for regional block. Reg Anesth Pain Med. 2007;32:146–151.
4 Choquet O, Capdevila X, Bennourine K, et al. A new inguinal approach for the obturator nerve block: anatomical and randomized clinical studies. Anesthesiology. 2005;103:1238–1245.
5 Akata T, Murakami J, Yoshinaga A. Life-threatening haemorrhage following obturator artery injury during transurethral bladder surgery: a sequel of an unsuccessful obturator nerve block. Acta Anaesthesiol Scand. 1999;43:784–788.
6 Woodburne RT. The accessory obturator nerve and the innervation of the pectineus muscle. Anat Rec. 1960;136:367–369.