Chapter 64 Obstructive sleep apnea in children with adenotonsillar hypertrophy
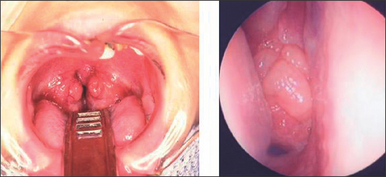
Obstructive sleep apnea (OSA) is a common and serious cause of morbidity during childhood. It affects 1−3% of children of 2−8 years old. However, habitual snoring during sleep is a much more frequent occurrence and affects up to 27% of children, with a decrease in frequency in 9 to 14 year olds. OSA in children presents some characteristics which differ from those in adults. Adenotonsillar hypertrophy (Fig. 64.1) is the most frequent causative disease according to our recent experience (Table 64.1). In addition, OSA results in some specific features (Table 64.2), which may only be observed in children. Furthermore, the correlation between OSA and sudden infant death syndrome (SIDS), and ALTE (apparent life-threatening event) in infants should be addressed further.
Table 64.1 The causative diseases of obstructive sleep dyspnea in children
| Hypertrophy of tonsil and adenoid | 88.9% |
| Habitual angina | 3.7% |
| Nasal allergy | 2.5% |
| Sudden infant death syndrome | 1.2% |
| Hunter–Hurler syndrome | 1.2% |
| Niemann–Pick’s disease | 1.2% |
| Prader–Willi syndrome | 1.2% |
Table 64.2 Typical features of OSA in children
| Adenoid face |
| Mouth-breathing |
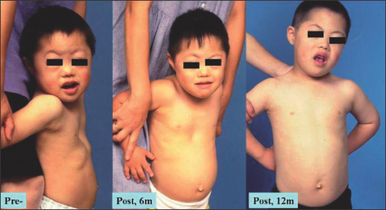
| Chest deformity (Fig. 64.2) |
| Snoring and apnea |
| Supraclavicular and intercostals retractions |
| Sweating |
| Late awaking, or forced awaking |
| Longer daytime sleep, sleepiness |
| Late asleep |
| Sudden awakening |
| Bed wetting or its recurrence |
| Abnormal behavior |
| Poor academic achievement |
1 DIAGNOSIS OF DYSPNEA IN CHILDREN
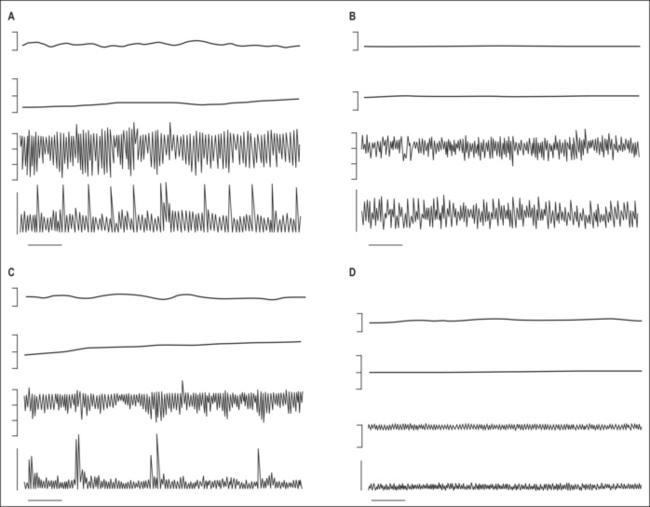
Polysomnographic diagnosis is usually necessary for adults, in whom clinical symptoms will be presented when there are more than five apneas per hour, or over 30 times in 7 hours of sleep. In the case of children, apnea-like symptoms may be observed even when there is continuous hypoventilation, but not a typical apnea. We measured the esophageal pressure (Peso) to evaluate the respiratory efforts in children with adenotonsillar hypertrophy and OSA, and discovered that the degree of Peso increased even without apnea when in deep sleep (Fig. 64.3). Therefore, because the measurement of polysomnography (PSG) in a child is difficult, and also because of the specific characteristic of children’s OSA, the diagnostic criterion of PSG is still unclear in children, especially in infants.
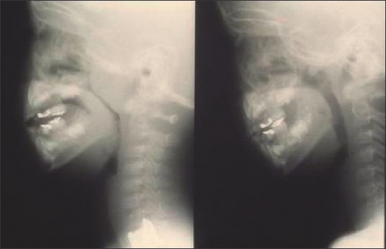
Monitoring oxygen saturation during sleep seems to be valid. The degree of stenosis in airways can be detected by profile roentgen film (Fig. 64.4), or by direct observation under a thin flexible fiberscope. A video camera is nowadays available in many families. A video record is also useful in observing respiratory situations, and even in cases without obvious desaturation, apnea could be found.
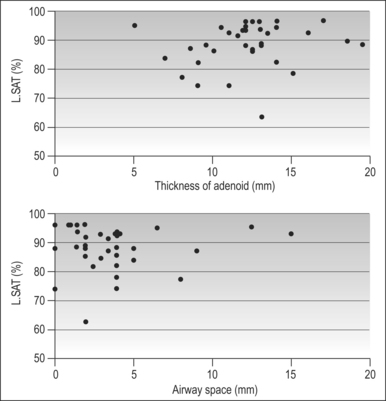
In 37 children with adenotonsillar hypertrophy, we inv estigated the thickness of adenoid, size of the airway space, and the lowest saturation during sleep. The lowest saturation was correlated to neither adenoid thickness nor airway space (Fig. 64.5). The grade of upper airway stenosis by adenoid or tonsillar hypertrophy on profile roentgen films could not predict the severity of apnea during sleep. For precise diagnosis of respiratory severity caused by adenoid–tonsillar hypertrophy, video observation with simultaneous SpaO2 monitoring is necessary. However, this result did not suggest that roentgenic measurement of stenosis is meaningless. When severe hypertrophy of the tonsil and adenoid is recognized, the possible existence of respiratory impairment should be investigated out of caution. Even in cases with moderate hypertrophy, severe apnea could be a possible accompaniment.
On the other hand, the adenoid and tonsil keep growing after birth until around 8 years old. Although the airway space in the pharynx also becomes larger, the ratio of adenotonsillar thickness to airway space reaches its peak at 4–6 years old. A previous study pointed out that children with OSA showed severe hypertrophy at younger ages (less than 3 years), which differed significantly compared to physiological hypertrophy of normal children (Fig. 64.6). Earlier surgical treatments are necessary for these cases.
3 RECENT ADVANCEMENTS IN ADENOIDECTOMY AND TONSILLECTOMY
3.1 MICRODEBRIDER ADENOIDECTOMY
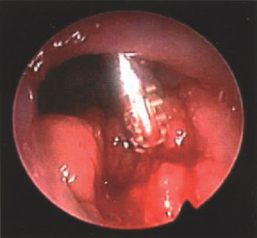
The microdebrider system (Fig. 64.7) was applied in adenoidectomy. The probe of the microdebrider is curved about 30° ahead and is inserted through an oral approach, with access to the adenoid from behind the soft palate. The operation is carried out under direct vision using an endoscope from a nasal approach. Numerous advantages of microdebrider over traditional techniques have been cited, including reduced operation time (by nearly 5 minutes), decreased intraoperative and postoperative bleeding, improved visualization and precision for tissue removal, and an overall faster wound healing. The soft tissues around the torus tubalis and posterior nasal aperture could be ablated more easily and safely than in the traditional approach.
3.2 SUCTION COAGULATOR ADENOIDECTOMY
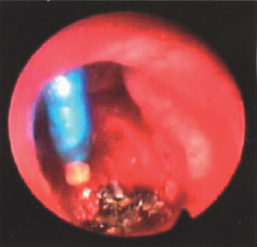
The suction coagulation system was another recommended method. In this approach, the soft palate should be elevated first by a catheter. The operation is under direct observation by 70° endoscope. The probe is appropriately angled in the tip (Fig. 64.8), and is inserted into the adenoid from an oral approach. After several seconds of electrification (with output being regulated between 30 and 45 W), the adenoid tissue is then coagulated and sucked out. The probe is pulled out after stopping the electrical charge, and then inserted again for coagulation. Coagulation should be performed from lateral to midline when around the torus tubalis, and from superior to inferior when near the posterior nasal aperture. Thus, a thorough removal of the adenoid can be ensured with little injury to the surrounding tissue. The operation may be completed when the epipharynx can be viewed from the posterior nasal aperture after careful hemostasis.
3.3 COBLATION TONSILLECTOMY
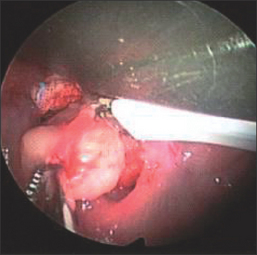
The conventional management of tonsillectomy was performed. Nowadays, intracapsular tonsillectomy can be performed by a variety of technical means, such as cold dissection, electrocautery, microbipolar and radiofrequency. Coblation tonsillectomy has been recently introduced in clinical practice. Using this method, only the mucosa at the superior pole is to be incised by a surgical knife. Afterwards, dissection of the tonsil can be performed by alternatively applying dissection and coagulation models of the coblation system (Fig. 64.9).
4 EFFICACY OF SURGICAL TREATMENT
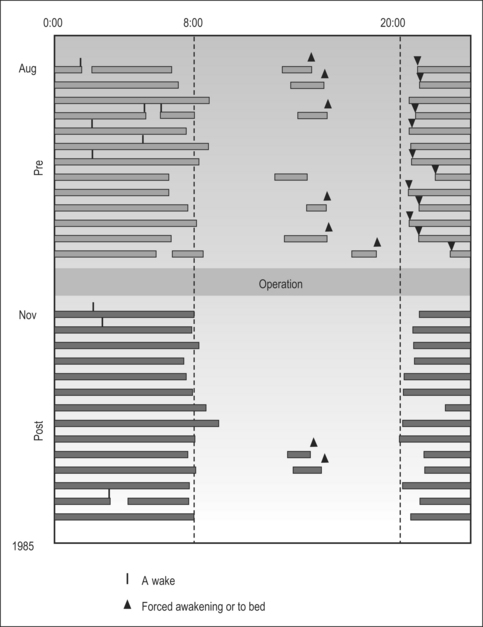
We use a sleep diary to evaluate the efficacy of the treatment. Figure 64.10 is a typical sleep diary of a boy with moderate OSA, pre- and postoperation. Before surgery, the boy consistently avoided going to bed at night, fighting desperately against sleep. As a consequence, his mother usually had to force him to go to bed at night. He sometimesawoke during the night. His time of awakening was very irregular in the morning. In the day time, he often took long naps. After surgery, many of these problems disappeared and his night sleep became undisturbed.
Figure 64.11 shows the Peso pattern according to sleep stages in 15 cases of adenoid–tonsillar hypertrophy. Six of them underwent tonsillectomy adenoidectomy. Their postoperative Peso levels decreased significantly in comparison with preoperative levels. Figure 64.3 shows typical changes of respiratory dynamics in different sleep stages in a boy with severe OSA.
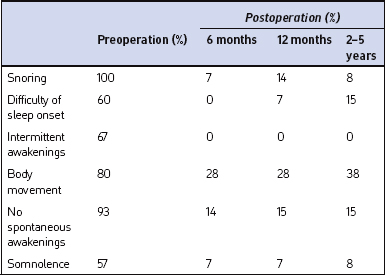
Long-term surgical effects in the sleep situation were noted (Table 64.3). Before the operation, 90–100% of patients showed difficulty in spontaneous awakening, reporting snoring or impaired breathing. These symptoms decreased to 10–20% after surgery. Improvement of chest deformity could also be observed (see Fig. 64.2).
Wynn R, Rosenfeld RM, et al. Outcomes in suction coagulator adenoidectomy. Arch Otolaryngol Head Neck Surg. 2003;129:182-185.
Anand A, Vilela RJ, Guarisco JL. Intracapsular versus standard tonsillectomy: review of literature. J La State Med Soc. 2005;157:259-261.
Bellosa A, Chidambaram A, Morar P, et al. Coblation tonsillectomy versus dissection tonsillectomy: postoperative hemorrhage. Laryngoscope. 2003;113:450-452.
Cohen SR, Simms C, Burstein FD. Mandibular distraction osteogenesis in the treatment of upper airway obstruction in children with craniofacial deformities. Plast Reconstr Surg. 1998;101:312-318.
Coticchia JM, Yun RD, Nelson L, Koempel J. Temperature-controlled radiofrequency treatment of tonsillar hypertrophy for reduction of upper airway obstruction in pediatric patients. Arch Otolaryngol Head Neck Surg. 2006;132:425-430.
Friedman M, LoSavio P, Ibrahim H, Ramakrishnan V. Radiofrequency tonsil reduction: safety, morbidity, and efficacy. Laryngoscope. 2003;113:882-887.
Hoffmann HJ, Damus K, Hillman L, et al. Risk factors for SIDS: results of the National Institute of Child Health and Human Development SIDS cooperative epidemiological study. Ann NY Acad Sci. 1988;533:13-30.
Hultcrantz E, Linder A, Markstrom A. Long-term effects of intracapsular partial tonsillectomy (tonsillotomy) compared with full tonsillectomy. Int J Pediatr Otorhinolaryngol. 2005;69:463-469.
Koltai PJ, Solares CA, Koempel JA, et al. Intracapsular tonsillar reduction (partial tonsillectomy): reviving a historical procedure for obstructive sleep disordered breathing in children. Otolaryngol Head Neck Surg. 2003;129:532-538.
Lister MT, Cunningham MJ, Benjamin B, et al. Microdebrider tonsillotomy vs. electrosurgical tonsillectomy: a randomized, double-blind, paired control study of postoperative pain. Arch Otolaryngol Head Neck Surg. 2006;132:599-604.
Mandell DL, Yellon RF, Bradley JP, et al. Mandibular distraction for micrognathia and severe upper airway obstruction. Arch Otolaryngol Head Neck Surg. 2004;130:344-348.
Miyazaki S. Sleep-induced respiratory disturbance in children with adenotonsillar hypertrophy: the obstructive sleep dyspnea syndrome. Operat Tech Otolaryngol Head Neck Surg 1991;2:69–72
Miyazaki S, Itasaka Y, Yamakawa K, et al. respiratory disturbance during sleep due to adenoid–tonsil hypertrophy. Am J Oto. 1989;10:143-149.
Nunez DA, Provan J, Crawford M. Postoperative tonsillectomy pain in pediatric patients: electrocautery (hot) vs. cold dissection and snare tonsillectomy – a randomized trial. Arch Otolaryngol Head Neck Surg. 2000;126:837-841.
Shintani T, Asakura K, Kataura A. Evaluation of the role of adenotonsillar hypertrophy and facial morphology in children with obstructive sleep apnea. ORL. 1997;59:286-291.
Temple RH, Timms MS. Paediatric coblation tonsillectomy. Int J Pediatr Otorhinolaryngol. 2001;61:195-198.
Timms MS, Temple RH. Coblation tonsillectomy: a double blind randomized controlled study. J Laryngol Otol. 2002;116:450-452.
Wynn R, Rosenfeld RM. Outcomes in suction coagulator adenoidectomy. Arch Otolaryngol Head Neck Surg. 2003;129:182-185.