Obliterative Procedure for the Correction of Pelvic Organ Prolapse
Obliterative Procedure
LeFort Partial Colpocleisis
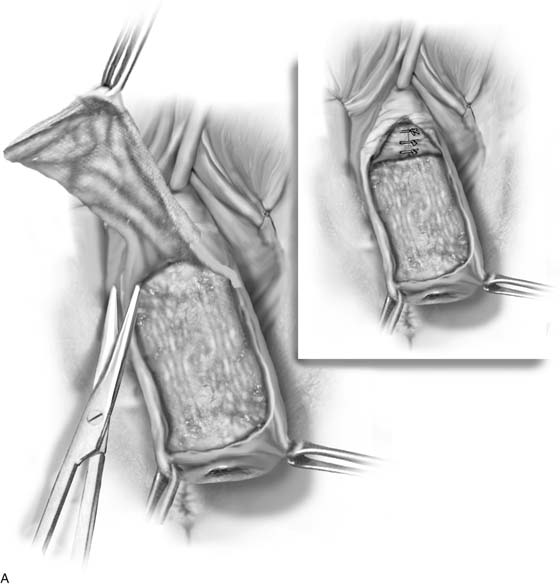
In elderly, fragile, or medically compromised patients with advanced prolapse, the best management option is sometimes an obliterative procedure. The advantages of these procedures are that they can be performed quickly with minimal morbidity, often with the patient under a local anesthetic. When a uterus is present, a LeFort partial colpocleisis (Fig. 56–1) is performed as follows:
1. Traction is placed on the cervix to evert the vagina completely, and a 0.5% solution of lidocaine or bupivacaine (marcaine) with epinephrine is used to inject the vaginal tissue below the epithelium. A pudendal nerve block can be used if the procedure is being performed with the patient under local anesthetic. A Foley catheter with a 30-mL balloon is placed for easy identification of the bladder neck.
2. A dilatation and curettage should be performed if it was not performed preoperatively to ensure that no premalignant or malignant process is present in the uterus.
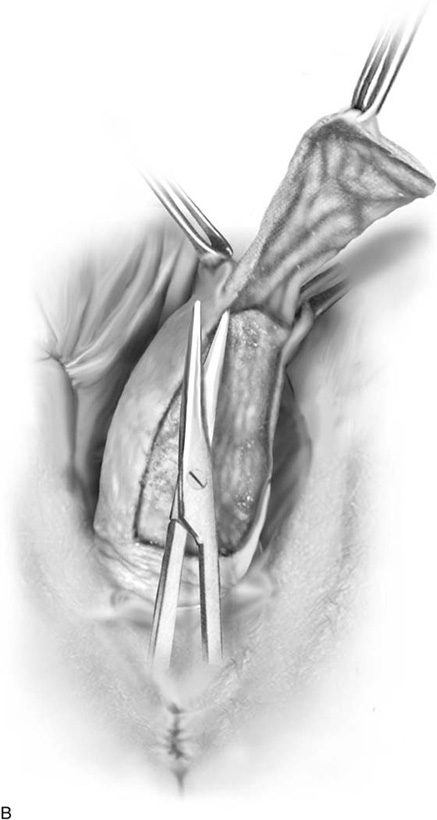
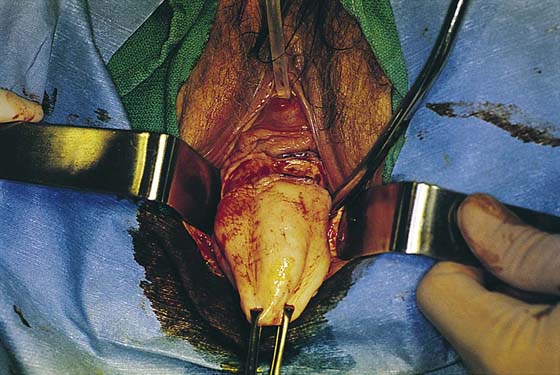
3. Areas to be denuded anteriorly and posteriorly are marked out with a scalpel or a marking pencil, as indicated in Figure 56–2. The rectangular piece of anterior vaginal wall should extend from 2 cm proximal to the tip of the cervix to approximately 5 cm below the external urethral meatus (see Fig. 56–2).
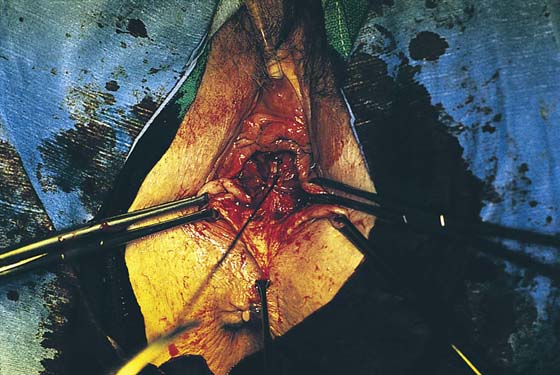
4. Sharp and blunt dissection is used to remove the vaginal epithelium. These flaps should be thin, leaving the maximum amount of fascia on the bladder and rectum. Sufficient vagina should be left bilaterally to form canals for draining cervical secretions or blood. We almost routinely perform a plication of the bladder neck (see Fig. 56–1). Posteriorly, the cul-de-sac peritoneum may be encountered when the vaginal mucosa is excised, but it does not have to be entered. Bleeding is controlled with fulguration. Absolute hemostasis is necessary to avoid a postoperative hematoma in the vaginal canal.
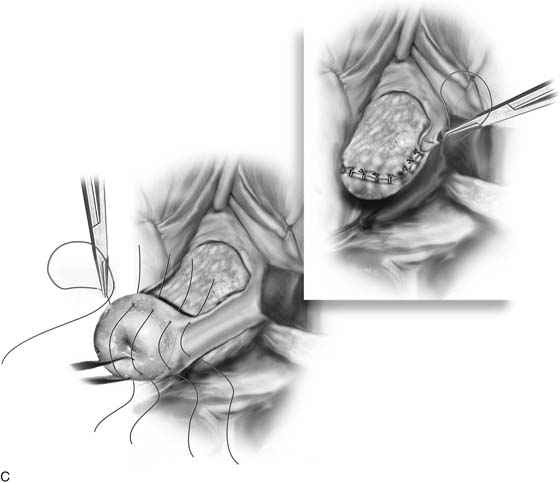
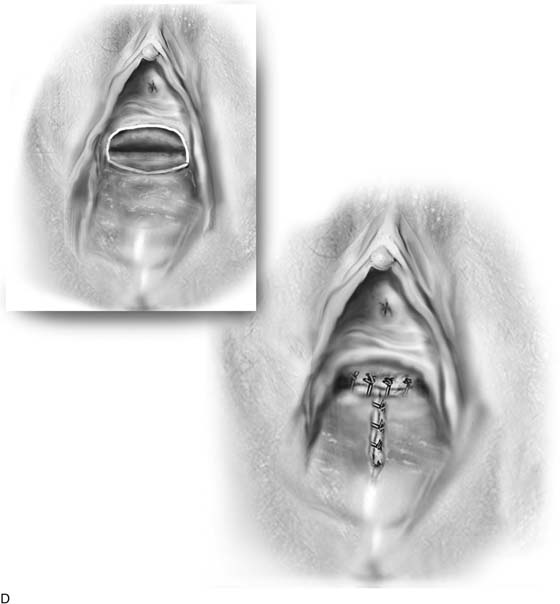
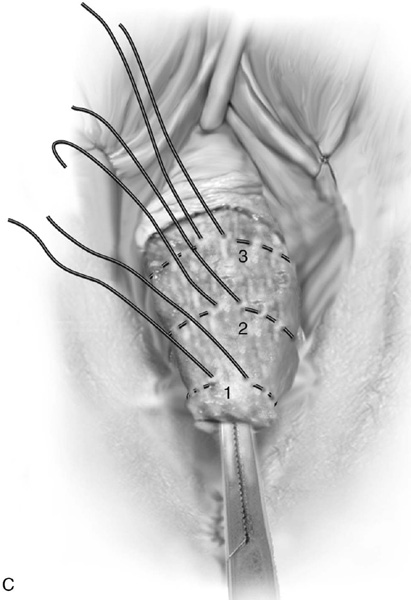
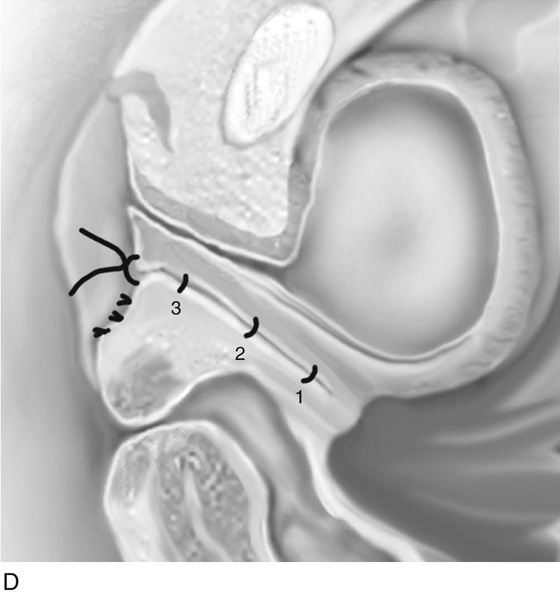
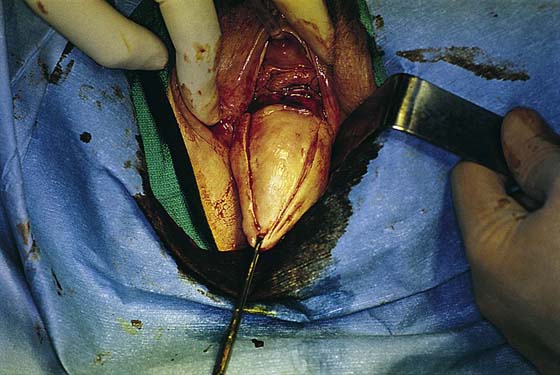
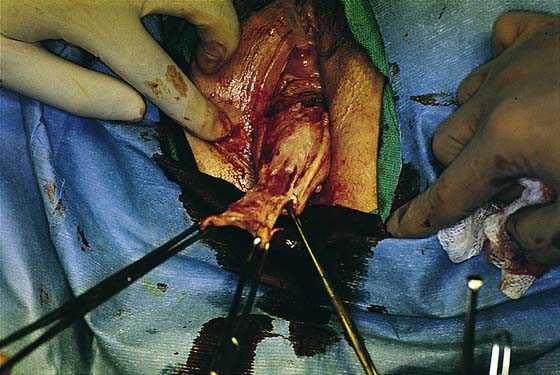
5. The cut edge of the anterior vaginal wall is sewn to the cut edge of the posterior vaginal wall with interrupted delayed absorbable sutures (Figs. 56–3 and 56–4). This is achieved in such a way that the knot is turned into and remains in the epithelium-lined tunnels that are created bilaterally (Fig. 56–5). Suturing in this way gradually pushes the uterus and the vaginal apex inward. When the entire vagina has been inverted, the superior and inferior margins over the rectangle can be sutured horizontally (Fig. 56–6).
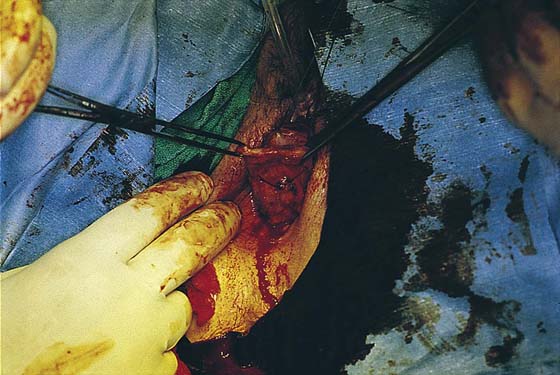
6. Perineorrhaphy and distal levatorplasty is usually performed to increase posterior pelvic muscle support and narrow the introitus. Postoperatively, the patient is mobilized early; however, heavy lifting is avoided for at least 2 months to prevent recurrence of the prolapse secondary to breakdown of the repair. Figure 56–7 reviews the technique of LeFort partial colpocleisis with perineorrhaphy.
Colpectomy and Colpocleisis
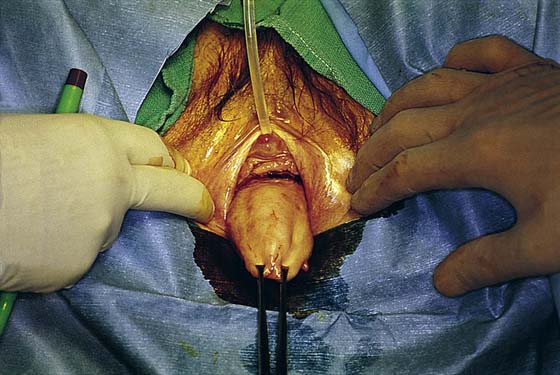
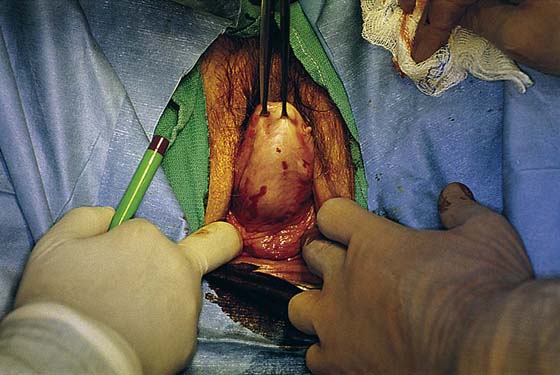
In cases of posthysterectomy vaginal vault prolapse in which obliteration of the vagina is chosen as the procedure of choice, it is best to proceed with a colpectomy and complete colpocleisis. This operation is performed in cases of vault prolapse when operating time is best kept at a minimum and future vaginal intercourse is not anticipated. This procedure can also be performed with the patient under local anesthetic. The operation is performed by completely excising the vaginal mucosa from the underlying vaginal or endopelvic fascia. It is not necessary to enter the peritoneum. A series of purse string delayed absorbable sutures are placed, slowly inverting the vaginal muscularis and fascia (Figs. 56–8 through 56–20). Similar to the LeFort procedure, bladder neck plication and perineorrhaphy with levatorplasty are often performed with a colpectomy.
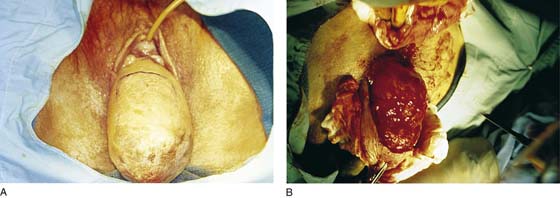
FIGURE 56–1 LeFort partial colpocleisis. A. A rectangular piece of anterior vaginal wall has been removed. Note in the inset that the dissection has been extended laterally at the level of the proximal urethra to perform a Kelly-Kennedy plication in the hope of providing preferential support to the bladder neck and thus preventing any occult or potential stress incontinence. B. A similar rectangular piece of posterior vaginal wall is removed. A portion of this posterior vaginal wall will usually lie over an enterocele, and one should attempt to avoid entering the peritoneal cavity if at all possible. C. The cut edge of the anterior incision, at the level of the cervix, is sewn to the distal cut edge of the posterior incision with interrupted 2-0 delayed absorbable sutures. Inset. Once the cervix is inverted, the interrupted sutures are taken through the cut edges of the lateral portions of the incision on each side. D. Once the entire vagina has been inverted, the superior and inferior margins over the rectangle can be sutured horizontally, thus completely obliterating the midportion of the vagina. Note: Draining channels are left in the lateral portions of the vagina to facilitate drainage of any cervical discharge. A levatorplasty is commonly performed to increase posterior pelvic muscle support and to narrow the introitus.
FIGURE 56–2 A. Complete procidentia. B. A rectangular piece of anterior vaginal wall has been excised.
FIGURE 56–3 Interrupted 2-0 absorbable sutures are placed initially, approximating the lower transverse edge of the anterior vaginal wall incision to the upper transverse edge of the posterior vaginal wall. This row of sutures reduces or buries the cervix.
FIGURE 56–4 Sutures are placed all the way to the distal incisions on the anterior and posterior vaginal walls.
FIGURE 56–5 As the uterus is reduced, draining channels are created on each side.
FIGURE 56–6 A. Once the uterus is reduced, the distal transverse incision on the anterior vaginal wall is sewn to the distal transverse incision on the posterior vaginal wall. B. Note the closed vagina with lateral draining channels.
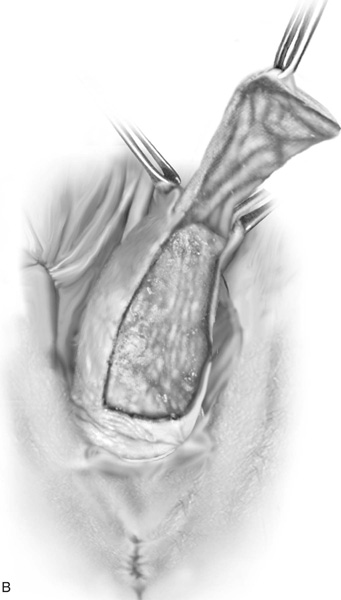
FIGURE 56–7 Technique of a LeFort partial colpocleisis in conjunction with a perineorrhaphy. A. A rectangular piece of anterior vaginal wall is being excised. B. The entire anterior dissection has been completed. Note that the rectangular piece of vagina has been removed to the level of the bladder neck to facilitate the performance of a Kelly-Kennedy plication. C. The dissection has been extended laterally at the level of the bladder neck, and the Kelly-Kennedy plication stitch has been placed. D. The cut edges of the anterior and posterior vaginal wall incisions have been sewn together as previously described. The completed LeFort is shown here. Note that the horizontal superior and inferior edges have been sewn in the midline and the Kelly clamp is placed in the left lateral draining channel. E. An incision has been made at the level of the perineum to identify the levator muscle. F. A levatorplasty has been performed by plicating the distal portions of the levator muscle across the midline to facilitate posterior vaginal wall support.
FIGURE 56–8 Colpectomy and complete colpocleisis. A and B. After subcutaneous infiltration with lidocaine or bupivacaine in 1:200,000 epinephrine solution, the vagina is circumscribed by an incision at the site of the hymen and is marked into quadrants. Each quadrant is removed by sharp dissection. C. Purse string delayed absorbable sutures are placed. The leading edge of the soft tissue is inverted by the tip of a forceps. Purse string sutures are tied 1 before 2 and 2 before 3, with progressive inversion of the soft tissue before the tying of each suture. D. The final relationship is shown in cross-section. A perineorrhaphy is also usually performed.
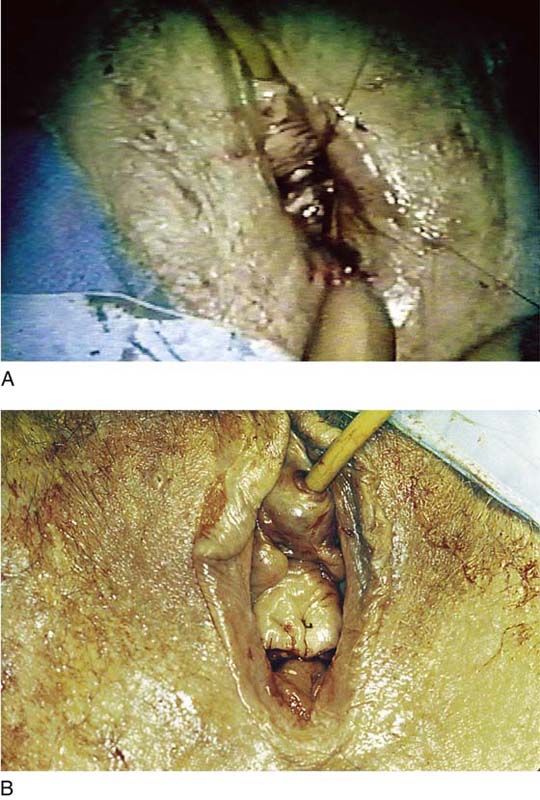
FIGURE 56–9 The base of the prolapse has been marked with a marking pencil.
FIGURE 56–10 The level of the posterior aspect of the incision is demonstrated.
FIGURE 56–11 An incision has been made at the base of the prolapse very near the hymenal ring.
FIGURE 56–12 An incision is made through the vaginal mucosa in preparation for removal of the first quadrant of the vagina.
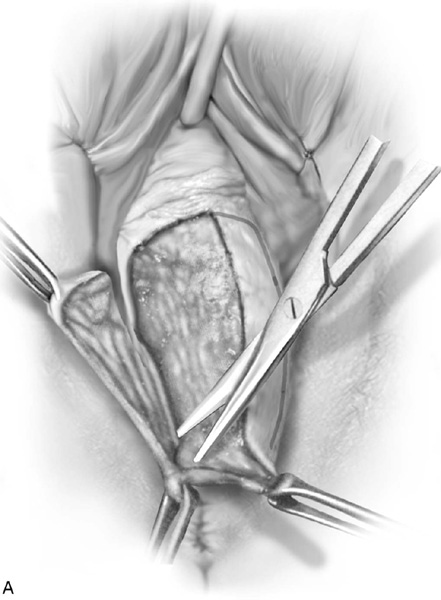
FIGURE 56–13 The first quadrant of the vagina over the prolapse is sharply removed from the underlying tissue.
FIGURE 56–14 The remainder of the vaginal epithelium has been removed.
FIGURE 56–15 The initial purse string 2-0 absorbable suture has been placed.
FIGURE 56–16 The first purse string suture has been tied, and the second purse string suture has been placed.
FIGURE 56–17 The second purse string suture has been tied.
FIGURE 56–18 The third purse string suture has been placed.
FIGURE 56–19 The third purse string suture has been tied.
FIGURE 56–20 The vaginal epithelium is closed, completing the repair.