148 Obesity
Salient features
History
• Family history of obesity (parental obesity more than doubles the risk of adult obesity among both obese and non-obese children under 10 years of age; N Engl J Med 1997;337:869–73)
• History of sleep apnoea, snoring and insomnia
• History of hypertension, diabetes, hyperlipidaemia, cardiovascular disease
• History of gallstones (cholesterol gallstones more prevalent in obesity)
• History of endometrial cancer in women (two to three times more common in obese than in lean women)
• History of breast cancer (risk increases with body mass index in postmenopausal women)
• Cancer of gallbladder and biliary system (obese women have a higher incidence)
• Cancer of colon, rectum, prostate and renal cell cancer (N Engl J Med 2000;343:1305–11) (higher in obese men)
• Medication history: antipsychotics, antidepressants, corticosteroids, oral contraceptives, beta-blockers, oral hypoglycaemic agents, insulin, anticonvulsants, antihistamines, pitzotifen.
Examination
• Measure the height and body weight (to determine body mass index (BMI))
• Check BP (the prevalence of hypertension is approximately three times higher for the obese than the non-obese)
• Examine the joints to exclude osteoarthrosis
• Examine skin for intertrigo in redundant folds of skin (fungal and yeast infections of skin are also common)
• Tell the examiner that you would like to:
Advanced-level questions
Mention some adverse health consequences of obesity
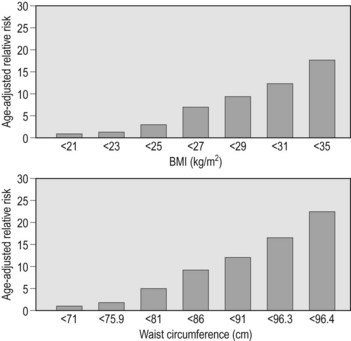
They have a greater risk for diabetes mellitus (Fig. 148.1), stroke, coronary artery disease, premature mortality, thromboembolism, gallstones, reflux oesophagitis, sleep apnoea, polycythaemia and cancer of the colon, rectum, prostate, uterus, breast and ovary. The risk of death from all causes is increased and the risk is associated with a high BMI is greater for whites than black. Also higher maternal weight before pregnancy increases the risk of late fetal death, although it protects against delivery of a small-for-gestational age infant.
How would you manage such patients?
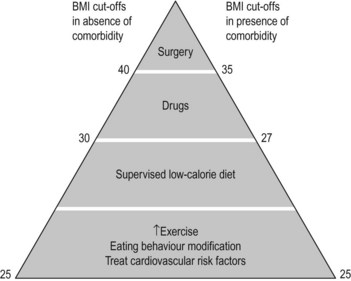
Approach is based on BMI and comorbidities such as cardiovascular disease (Fig. 148.2):
• Multidisciplinary approach to weight loss: hypocaloric diets, exercise, social support. Caloric restriction of 500 kcal daily would result in the loss of about 1 lb (0.5 kg) per week
• Behaviour modification and social support
• Drugs: Sibutramine (serotonin–norepinephrine reuptake inhibitor that reduces appetite) results in weight loss that is about 5% greater than in those taking placebo. Orlistat partially inhibits absorption of dietary fat (binds to pancreatic lipase in the GI tract; Lancet 1998;352:167–73). Side effects include oily spotting, flatus with discharge and faecal urgency. Rimonabant (a selective blocker of the cannabinoid receptor CB1) has shown to result in 5% weight loss when compared with placebo.
What are the mechanisms of obesity?
Mention some syndromes where obesity is a prominent feature
Cushing syndrome (p. 538), Laurence–Moon–Biedl syndrome (p. 724), Pickwickian syndrome (p. 410), Alstrom syndrome, Prader–Willi syndrome.