O
object 1. Something that has a fixed shape or form that you can touch or see. 2. Anything from which an image is formed by an optical system.
extended o. An object consisting of many point objects separated laterally to form a certain shape (e.g. trees, people).
See light, beam of; light, pencil of; source, extended.
point o. A small component of an extended object, in relation to an optical system. If the point object is situated on the axis of an optical system it gives rise to the axial ray and it is referred to as the axial point object.
real o. An object from which emergent rays diverge.
o. of regard See fixation, point of.
virtual o. One towards which incident rays are converging after refraction or reflection. Example: a positive lens forms an image of an object placed beyond its anterior focal point. Introducing a mirror between the lens and the image makes that image become a virtual object.
objective An optical system or a lens used to provide a real image of an object. In cameras this image is situated on the film but in viewing instruments (telescopes, microscopes, etc.) this image is seen through an eyepiece. Syn. objective lens.
See aperture, numerical.
oblique astigmatism; effect See under the nouns.
oblique illumination shadow test See test, shadow.
oblique muscles See muscle, superior oblique; muscle, inferior oblique.
obliquely crossed cylinders See crossed cylinders, obliquely.
occipital cortex; lobe See under the nouns.
occluder A device placed before an eye to block vision or to partially obscure vision. Syn. eye shield.
occluder, Bangerter See Bangerter foils.
occlusion The act of blocking or the state of being blocked. Examples: vision with an occluder, a vessel with an embolus.
o. amblyopia See amblyopia; occlusion treatment.
o nystagmus See nystagmus, occlusion.
punctal o. Sealing of the lacrimal punctum, temporarily (e.g. with a plastic plug) or permanently (e.g. by heat cauterization), to preserve the natural tears or prolong the effect of artificial tears. This method is commonly used in the management of keratoconjunctivitis sicca. Occasionally a plug made of collagen is used prior to insertion of a more permanent type of punctal plug, because it dissolves within a week. This is done to determine whether permanent or semipermanent occlusion (as with a silicone plug) is likely to succeed.
See keratopathy, neurotrophic.
retinal arterial o. See retinal arterial occlusion.
retinal vein o. See retinal vein occlusion.
o. treatment A method of treating amblyopia or strabismus by covering the good eye. Such a method is most effective below the age of four years and with little effect after the age of nine years, that is beyond the critical period of development. However, this technique must be used with caution as prolonged occlusion in very young children can lead to a reversal of eye dominance in which the previously good eye becomes amblyopic (called occlusion amblyopia). Moreover, it has been shown that the effect of occlusion does not improve beyond six hours at a time. Alternate occlusion is preferred as both eyes are thus stimulated.
Syn. patching
See myopia, form-deprivation; penalization; period, critical; pleoptics.
octave The interval between two frequencies having a ratio of two to one. Example: from 4 to 8 c/deg. Two octaves is a quadrupling of frequencies, and so on. Octaves are commonly used in specifying the bandwidth of the frequencies (e.g. spatial frequencies) to which cells in the visual pathway respond.
See cycle per degree.
ocular 1. See eyepiece. 2. Appertains to eye.
ocular adnexa See appendages of the eye.
ocular albinism; appendages; apraxia; bobbing; column; cup; decongestant; dominance; dysmetria; flutter; fundus; headache; hypertension; hypotonia; impression; media; myoclonus; pathology; pemphigoid; prosthesis See under the nouns.
ocular lubricant See tears, artificial.
ocular myopathy See ophthalmoplegia.
ocular refraction See refractive error.
ocular tension See pressure, intraocular.
ocular tremors of fixation See movements, fixation.
ocularist One who designs and fits artificial eyes. See eye, artificial; prosthesis, ocular.
oculist See ophthalmologist.
oculoauriculovertebral dysplasia See syndrome, Goldenhar’s.
oculocardiac reflex See reflex, oculocardiac.
oculocentre Pertaining to the eye as a centre of reference.
See direction, oculocentric; egocentre; localization.
oculocentric direction; localization See under the nouns.
oculocutaneous albinism See albinism.
oculocutaneous melanosis; melanocytosis See naevus of Ota.
oculogyric Pertaining to movement of the eye about the anteroposterior axis.
oculogyric crisis (OCG) Sudden involuntary contractions of some eye muscles resulting in repetitive, conjugate ocular deviations, usually, though not always, in an upward direction. The attack or crisis may last from seconds to minutes. It occurs most frequently after the use of neuroleptic medication, but it may be precipitated or accompany, emotional stress, alcohol or general fatigue.
oculomotor Pertaining to movement of the eyes, or to the oculomotor nerve.
oculomotor nerve; nucleus See under the nouns.
oculomotor paralysis See paralysis of the third nerve.
oculomycosis Any disease of the eye caused by a fungus.
See antifungal agent; keratitis; keratomycosis.
oculorotary muscles See muscles, extraocular.
oculus Latin for eye. Plural: oculi.
oculus dexter (OD) Latin for right eye.
oculus sinister (OS) Latin for left eye.
oculus uterque (OU) Latin for both eyes.
oedema The presence of an excessive amount of fluid in or around cells, tissues or serous cavities of the body. In the eye oedema can occur in the cornea, the conjunctiva, the uvea, the retina, the choroid, and the ciliary body. Corneal oedema usually accompanies eye diseases, or contact lens wear with low oxygen transmissibility. Corneal oedema is easily seen with a slit-lamp using retroillumination or sclerotic scatter illumination. Quantitatively, it can be assessed with the addition of a pachometer that measures corneal swelling. Beyond about 4% swelling, there appear striae (wispy greyish-white lines usually vertical) in the stroma. Beyond about 8% swelling, there appear folds (dark lines) believed to represent physical buckling of the posterior corneal layers. Corneal swelling of 15% or greater, which indicates a gross separation of the collagen fibres of the stroma, results in a hazy or cloudy appearance of the cornea. There is a physiological oedema occurring during sleep in every human cornea amounting to an increase in thickness of about 4%. Corneal oedema gives rise to the appearance of haloes around lights, photophobia, spectacle blur, losses in corneal transparency and sometimes stinging. Management depends on the cause and tissue involved. If due to contact lenses, refitting with daily wear lenses of higher oxygen transmissibility and reducing wearing time usually solves the problem. Note: also spelt edema.
See blebs, endothelial; clouding, central corneal; hypoxia; lens, silicone hydrogel; oxygen permeability; oxygen requirement, critical; pachometer; syndrome, overwear.
oedema, cystoid macular (CMO) Oedema and cyst formation of the macular area of the retina. It may occur as a result of, or be associated with, systemic vascular disease, retinal vein occlusion, diabetic retinopathy, uveitis, hypertensive retinopathy, retinitis pigmentosa and following some ocular surgery such as vitreoretinal, photocoagulation, glaucoma procedures and especially cataract surgery. When cystoid macular oedema follows cataract surgery it is called the Irvine–Gass syndrome and it is sometimes accompanied by intraoperative vitreous loss or vitreous adhesion to the iris or to the corneoscleral wound. Visual acuity is affected initially but recovers in the majority of cases. In some cases antiinflammatory therapy may help in restoring visual acuity and in other cases the vitreous adhesion may be disrupted with a Nd-Yag laser.
ofloxacin See antibiotic.
Oguchi’s disease See disease, Oguchi’s.
olopatadine hydrochloride See antihistamine; mast cell stabilizers.
ommatidium One of the visual elements of the compound eye of arthropods. It is hexagonal in shape and about ten times longer than its diameter. It consists of a corneal facet below which is a crystalline cone which collects light and a sensory area called the rhabdom, all of it being enclosed in a dark pigment.
onchocerciasis A disease caused by infestation with the filarial worm (Onchocerca volvulus) spread by blackflies. It is common in tropical Africa and Central America, especially in areas near rivers. Large numbers of microfilariae are present on the skin and often enter the eye. The patient initially complains of itching, but blindness occurs as a result of chorioretinitis and optic neuritis. The disease is treated successfully with ivermectin. Syn. onchocercosis; river blindness.
‘one and one half’ syndrome See syndrome, ‘one and one half’.
opacity The condition of a tissue or structure which is not transparent, or being opaque. The location of an opacity within the eye can be determined with a slit-lamp. It can also be determined using an ophthalmoscope and asking the patient to look up or down. If the opacity moves very little, or not at all, it is situated in the lens. If the opacity moves in the same direction as the eye it is situated in front of the lens and if it moves in the opposite direction it is situated in the vitreous humour.
See cataract; muscae volitantes; ulcer, corneal.
opaque Impervious to the passage of light. See transparent.
operculum A flap of detached retina which projects forward, or is totally free in the vitreous. It can happen as a result of a retinal tear (break).
ophryosis Spasmodic twitching in the region of the eyebrow.
See eyebrow.
ophthalmagra A sudden pain in the eye.
ophthalmia Severe inflammation of the eye, especially, but not exclusively, one involving the conjunctiva.
See conjunctivitis.
o. neonatorum An acute conjunctivitis that occurs in the first month of life as a result of infection acquired in the birth canal. The most common causes are Chlamydia trachomatis, Streptococcus pneumoniae, Neisseria gonorrhoeae, Staphylococcus aureus and herpes simplex virus. The eyelids are swollen and stuck together by purulent discharge. If the cause is gonococcal, loss of the eye is a real and immediate threat. A gonococcal infection develops within 2–4 days after birth, whereas a chlamydial infection normally appears 5–14 days after birth. Differential diagnosis is facilitated by laboratory tests (e.g. Gram staining of conjunctival scrapings). Management depends on the cause: systemic erythromycin and topical tetracycline for chlamydial infection, ceftriaxone or cefotaxime for gonococcal infection, and eye irrigation with saline solution. Syn. blennorrhoea neonatorum; gonococcal ophthalmia; neonatal conjunctivitis.
See conjunctivitis, acute; conjunctivitis, adult inclusion.
sympathetic o. A rare, bilateral granulomatous inflammation of the uveal tract that usually follows perforation of one eye due to trauma, or more rarely intraocular surgery. The inflammation occurs first in the injured eye (called the exciting eye) and follows in the other eye (called the sympathetic eye). It usually occurs within 2 to 12 weeks, although some cases may appear later. The condition is believed to be a T-lymphocyte-mediated delayed hypersensitivity. Treatment usually involves enucleation of the exciting eye and high doses of systemic and topical corticosteroids in the sympathetic eye. Syn. sympathetic ophthalmitis.
See enucleation; immunosuppressants; uveitis.
ophthalmic Pertaining to the visual apparatus and its function.
ophthalmic crown See glass, crown.
ophthalmic cup See cup, optic.
ophthalmic Graves’ disease See disease, Graves’.
ophthalmic lens; nerve See under the nouns.
ophthalmic optician See optician; optometrist.
ophthalmic optics See optics, ophthalmic.
ophthalmic zoster See herpes zoster ophthalmicus.
ophthalmitis, sympathetic See ophthalmia, sympathetic.
ophthalmodynamometer (ODM) 1. Instrument for measuring the near point of convergence of the eyes. 2. Instrument for measuring the blood pressure of the central retinal artery. There are two types: the compression type (e.g. Bailliart’s ophthalmodynamometer) in which the pressure is raised by pressing on the eye, the force being produced by a spring-loaded plunger resting on the temporal bulbar conjunctiva of the anaesthetized eye, while the examiner observes the optic nerve through an ophthalmoscope. The other type is by suction in which negative pressure is applied to the eye using a scleral vacuum cup near the limbus (e.g. Doppler’s ophthalmodynamometer). The diastolic pressure is read from the gauge provided with the instrument when the central retinal artery is seen to pulsate on the optic disc and the systolic pressure is read when all arterial pulsations just cease (the instrument should be removed immediately afterwards). A low systolic pressure is indicative of an occlusive disease of the carotid artery (a comparison between the two eyes is also very informative) as such disorders are responsible for a significant percentage of ocular symptoms and strokes.
See amaurosis fugax; plaques, Hollenhorst’s.
ophthalmologist A medical specialist who practises ophthalmology. Syn. oculist (this term is rarely used nowadays); ophthalmic surgeon.
ophthalmology Part of medical science concerned with the medical and surgical care of the eye and its appendages.
ophthalmometer See keratometer.
ophthalmopathy Any eye disease. External ophthalmopathy refers to any disease of the conjunctiva, cornea, eyelids or the appendages of the eye. Internal ophthalmopathy refers to any disease of the lens, retina or other internal structures of the eye.
ophthalmopathy, thyroid Disease of the thyroid gland which leads to ocular manifestations. There are two main types: mild and severe. The mild type occurs in Graves’ disease in which most or some of the typical signs may be present and to a different extent (e.g. retraction of the eyelids, exophthalmos, defective eye movements and optic neuropathy). The severe type is much less common and affects the sexes equally in middle age. All the signs of Graves’ disease are present but are more pronounced with the addition of oedema of the eyelids and of the conjunctiva, conjunctival injection, enlargement of the extraocular muscles and in a few cases there is also optic neuropathy due to compression of the optic nerve or its blood supply with consequent visual loss, colour vision impairment and often diplopia. Syn. dysthyroid eye disease; thyroid eye disease.
See accommodative insufficiency; keratoconjunctivitis, superior limbic; neuropathy, optic.
ophthalmophakometer Optical instrument designed by Tscherning in 1892.
See phakometer.
ophthalmoplegia Paralysis of the ocular muscles. External ophthalmoplegia refers to paralysis of one or more extraocular muscles. If the levator palpebrae muscle is also involved, the condition is usually referred to as ocular myopathy. Internal ophthalmoplegia refers to a paralysis of the muscles of the iris and the ciliary muscle. Total ophthalmoplegia refers to a paralysis of all the muscles in the eye, which results in ptosis, immobility of the eye and pupil, and loss of accommodation.
See disease, Graves’; paralysis of the third nerve.
chronic progressive external o. (CPEO) A rare disorder characterized by a progressive, bilateral ptosis and a loss of ocular motility. It is associated with mutation of mitochondrial DNA, which results in abnormalities in highly oxidative tissues such as the muscles and the brain. The initial sign is bilateral ptosis, followed later by strabismus. A related mitochondrial myopathy is the Kearns–Sayre syndrome in which there is CPEO, a type of retinitis pigmentosa characterized by coarse pigment clumping which principally affects the central retina, and cardiac conduction defects. This syndrome presents before age 20 years.
See myasthenia gravis.
internuclear o. (INO) An eye movement disorder resulting from a lesion in the medial longitudinal fasciculus, which disrupts the coordination between the oculomotor nucleus and the abducens nucleus. It is characterized by a limited adduction by the eye on the same side of the body as the lesion, and a jerky, horizontal nystagmus and overshoot by the other eye on abduction, when moving the eyes towards the side of the body opposite to that of the lesion. Convergence is usually intact, unless the lesion is widespread. Vertical gaze gives rise to nystagmus and oscillopsia. The condition is associated with multiple sclerosis, vascular disease, tumour of the brainstem or encephalitis.
See dysmetria, ocular; palsy, supranuclear gaze; syndrome, ‘one and one half’.
ophthalmorrhagia Ocular haemorrhage.
ophthalmorrhoea A discharge of mucus, pus or blood from the eye. Note: also spelt ophthalmorrhea.
ophthalmoscope An instrument for viewing the media and fundus of the eye. It consists essentially of: (1) a light source (a halogen or tungsten bulb), a condenser system, a lens and a reflector (a prism, mirror, or metallic plate) to illuminate the interior of the eye, and (2) a viewing system comprising a sight hole and focusing system (usually a rack of lenses of different powers) to compensate for the combined errors of refraction of the patient and practitioner.
See transillumination; Visuscope.
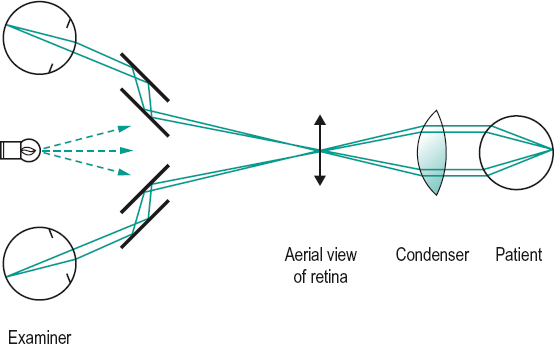
binocular indirect o. (BIO) An indirect ophthalmoscope with a binocular viewing system for obtaining a magnified, inverted, stereoscopic image of the fundus. It consists of a light source mounted above and between the examiner’s eyes on a headset. This illuminates a handheld condensing lens of high positive power close to the patient’s eyes, which forms an image of the patient’s pupil in both of the examiner’s pupils. An aerial image of the patient’s fundus is formed between the condensing lens and the examiner (if the patient is emmetropic the image will be formed in the focal plane of the condensing lens). It appears inverted and stereoscopically through the oculars attached to the headset. Stereopsis is obtained by reducing the interpupillary distance by means of mirrors or prisms within the headset of the instrument. This ophthalmoscope allows examination of a wide area of fundus and perception of depressed and raised areas (Fig. O1).
confocal scanning laser ophthalmoscope (CSLO) An instrument using a confocal laser system to provide and analyse a three-dimensional image of the optic nerve head, peripapillary retina and macular region. The instrument uses a 670 nm diode laser and measures the amount of light reflected from a series of 16–64 optical sections in depth and reconstructs them to show the topography of the optic nerve head and a measure of the thickness of the retinal nerve fibre layer (RNFL). The RNFL thickness is compared with an age-matched normative database. The instrument is used to analyse RNFL defects, to detect damage to the optic nerve head and progressive changes over time in glaucomatous eyes, as well as retinal oedema, which occurs in the early stages of diabetic retinopathy. Syn. confocal scanning laser tomograph.
See glaucoma detection; microscope, confocal.
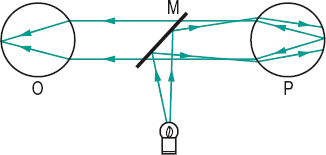
direct o. An ophthalmoscope that provides a virtual, erect image with a magnification of about × 15 of the fundus, formed by the patient’s eye in combination with whatever focusing lenses are needed to correct for the refractive errors of the observer and patient. The instrument is held at close range to the patient’s eye and the field of view is small (less than 10°) (Fig. O2). The magnification M of a direct ophthalmoscope is equal to
< ?xml:namespace prefix = "mml" />

where Fe is the power of the eye. Example: the magnification of the fundus of an aphakic eye of +40.00 D is equal to 40/4 = 10×.
indirect o. An ophthalmoscope that provides an aerial image of the fundus (and not the fundus itself as with a direct ophthalmoscope), which is real, inverted, with a magnification of × 5 to × 7 and formed at approximately arm’s length from the practitioner. This aerial image is usually produced by a strong positive lens ranging in power from +13 D to +30 D that is held in front of the patient’s eye. The practitioner views this aerial image through a sight hole with a focusing lens to compensate for ametropia and accommodation. This instrument provides a large field of view (25–40°) and allows easier examination of the periphery of the retina. This instrument has been supplanted by the binocular indirect ophthalmoscope. The magnification of an indirect ophthalmoscope M is equal to

where Fe and Fc are the powers of the eye and of the condensing lens, respectively. Example: using a condensing lens of +15.00 D to view the fundus of an emmetropic eye yields a magnification of 60/15 = 4×.
See camera, fundus; image, inverted.
scanning laser o. (SLO) An ophthalmoscope that provides a continuous image of the ocular fundus on a TV monitor. It consists of a narrow laser beam, which is scanned horizontally and vertically to produce a rectangular area (called a raster) on the retina. A small beam of light is reflected back out of the eye to a light detector, which monitors the brightness of each point on the raster and relays the information to the corresponding element on a TV monitor where the image can be viewed and/or stored. Low illumination is used to make this procedure more comfortable than conventional photography and mydriatics are usually unnecessary. The field of view extends up to 40 degrees. The instrument has been especially valuable in diagnosing glaucoma and in research.
ophthalmoscopy Method of examination of the interior of the eye with an ophthalmoscope.
ophthalmoscopy, red-free Method of ophthalmoscopy using a blue-green filter in the illumination system. This gives a better contrast between the retinal vessels and the background and helps to differentiate more easily between retinal and choroidal lesions: retinal lesions appear black while choroidal ones appear grey. However, in most ophthalmoscopes that use tungsten filament bulbs, the amount of light of short wavelength is so small that the observation is difficult and a filter that lets more long wavelengths pass is used, such as a yellow-green one. As a result of this compromise there is only a slight increase in contrast between the retinal vessels and the background.
Oppel–Kundt visual illusion See illusion, Oppel–Kundt visual.
opponent-colour cells See cells, colour-opponent.
opponent-colour theory See theory, Hering’s of colour vision.
opsin See rhodopsin.
opsoclonus Involuntary, chaotic movements of both eyes in horizontal and vertical directions. It may be a sign of cerebellar disease.
Table O1
Comparison between direct and indirect ophthalmoscopes
| ophthalmoscope | form | image | field of view (in degrees) | magnification |
| direct | monocular | erect | 8 | ×15 |
| indirect | monocular | inverted | 20–40° | ×5 to ×7 |
| indirect | binocular | inverted | 40–75 | ×1.5 to ×4.5* |
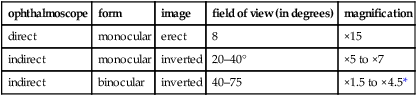
*Varies according to the power of the condensing lens.
See flutter, ocular; myoclonus, ocular.
optic Pertaining to light or to vision.
optic atrophy; canal; chiasma; cup; disc; disc coloboma See under the nouns.
optic fibre See optics, fibre.
optic foramen See canal, optic.
optic nerve head See disc, optic.
optic nerve; neuritis; neuropathy; neuropathy, anterior ischaemic; pit See under the nouns.
optic portion of a scleral lens See transition.
optic radiations See radiations, optic.
optic tracts; vesicle See under the nouns.
optic tectum See tectum of the mesencephalon.
optic zone, central Central region of a contact lens that has a prescribed optical effect where there is a peripheral optic zone or zones (British Standard).
optic zone diameter Diameter of the optic zone (front or back) of a contact lens measured to the surrounding junction. It is commonly specified in millimetres. Specifically, there are the back optic zone diameter (BOZD), formerly called back central optic diameter (BCOD), and the front optic zone diameter (FOZD). It is often difficult to measure these dimensions due to the blending of the line separating the zones, especially for the back optic zone diameter. The region surrounding the central optic zone is the peripheral zone. If there is more than one, the zones will be numbered first, second, etc., beginning with the zone immediately surrounding the central optic zone. The diameter of each peripheral zone is referred to as the back (or front) peripheral zone diameter (BPZD).
See blending; diameter, total; edge lift.
optic zone radius, back (BOZR) Radius of curvature of the back optic zone of a contact lens. (It was formerly called the back central optic radius (BCOR or BC) or posterior central curve radius (PCCR).) If the optic zone is surrounded by a peripheral zone there will be a radius of curvature of a back peripheral zone (BPR). If there are several zones there will be BPR1, BPR2, etc., beginning with the zone immediately surrounding the central optic zone.
See method, Drysdale’s; radiuscope; Toposcope.
optical aid See appliance, optical.
optical anisotropy; axis; centre See under the nouns.
optical biopsy Any technique that provides imaging of tissue morphology without the need for excision of the tissue. Example: optical coherence tomography (OCT).
optical centre position, standard See centre, standard optical position.
optical coherence tomography; density; dispensing; illusion; interface; medium See under the nouns.
optical microspherometer See radiuscope.
optical surface; system; system, compound; wedge See under the nouns.
optical zone of cornea A theoretical zone of about 4 mm in diameter in the centre of the cornea. It is assumed to be spherical for clinical purposes. Syn. corneal cap.
optician 1. One who designs and makes optical instruments or lenses. 2. Dispensing optician. 3. Ophthalmic optician.
optician, dispensing One who fits and adapts spectacles and contact lenses on the basis of a prescription by an ophthalmologist or optometrist (or ophthalmic optician). In many countries dispensing opticians cut and edge lenses and fit them into a frame.
See dispensing, optical; glazing.
optician, manufacturing One who makes optical or ophthalmic instruments, lenses, prisms or spectacles.
optician–optometrist See optometrist.
optics 1. The branch of physics which deals with the phenomena of light. 2. The elements and/or design of an optical instrument, including the eye (optics of the eye).
See theory, gaussian; theory, Newton’s; theory, quantum; theory, wave.
dispensing o. See optics, ophthalmic.
fibre o. A fine flexible glass or plastic rod that transmits light longitudinally by repeated total internal reflection. By using a bundle of such fibres in a fixed array, a complete image can be transmitted. As total internal reflection can occur even if the fibres are curved, the system is of great value for viewing or photographing inaccessible objects, such as internal organs of the body. Syn. fibre optic (although strictly this term is an adjective, e.g. a fibre optic cable, whereas the term fibre optics is a noun).
Table O2
Common optical symbols
| f, f’ | primary and secondary focal lengths |
| h, h’ | object and image sizes |
| i, i’ | angles of incidence or reflection |
| k, k’ | and refraction distances from the corneal pole |
| l, l’ | to the far point and to the retina, respectively distances of object and image from |
| n, n’ | the optical system refractive indices of object and |
| u, u’ or w, w’ or α, α’ | image space angular size of object and image |
| x, x’ | distances between object and first |
| r | focal point, and image and second focal point, respectively radius of curvature |
| c | centre of curvature |
| A | ocular accommodation |
| As | spectacle accommodation |
| Amp | amplitude of accommodation |
| Add | addition for near vision |
| B | dioptric distance to near point of |
| D | accommodation, measured from the eye dioptre |
| d | vertex distance |
| d or dec | decentration |
| F | power |
| Fc | power of a contact lens correction |
| Fe | equivalent power; power of the eye |
| Fsp | power of a spectacle lens |
| Fv, Fv’ | correction front and back vertex power |
| K | ocular correction |
| K’ | vergence of the retina or dioptric |
| E, E’ | length of the eye centres of entrance and exit pupils |
| L, L’ | object and image vergences |
| M or m | magnification |
| F, F’ | first and second focal points |
| N, N’ | first and second nodal points |
| P, P’ | first and second principal points |
| RSM | relative spectacle magnification |
| SM | spectacle magnification |
| ε or P | refractive power of a prism |
| Δ | prism dioptre |
See angle, critical; endoscope.
first-order o. See optics, paraxial.
gaussian o. See optics, paraxial.
geometrical o. The branch of optics that deals with the tracing of light rays through optical systems.
See sign convention; theory, gaussian.
mechanical o. See optics, ophthalmic.
ophthalmic o. 1. The branch of optics which deals with the design, measurement, assembly and fitting of lenses, spectacles, contact lenses, as well as optical aids for low vision patients. Syn. dispensing optics; mechanical optics. 2. In the UK and the Republic of Ireland it is used as a synonym for optometry.
See dispensing, optical; optometry.
o. of the eye The eye considered as an optical system composed of several elements, the two aspherical surfaces of the cornea (total power about +42 D), the two aspherical surfaces of the lens (total power +21 D), the depth of the anterior chamber (a change of 1 mm in depth corresponds to a change of about 0.7 D in the total power of the eye) and the refractive indices of the various media (it is a gradient in the lens) and their role in the formation of a retinal image. The total power of the eye is about +60 D. Syn. dioptric system of the eye.
See constants of the eye; Table P5.
paraxial o. A simplified representation of geometrical optics which deals only with paraxial rays and in which the law of refraction and the fundamental paraxial equation are applicable. Syn. first-order optics; gaussian optics.
See law, Lagrange’s; law of refraction; paraxial equation, fundamental; ray, paraxial.
physical o. The branch of optics that deals with the nature of light and with the phenomena of diffraction, interference, polarization and velocity of light.
See theory, quantum; theory, wave.
physiological o. The branch of optics concerned with physiological, psychological and optical aspects of visual perception.
visual o. Branch of optics and optometry which deals with the dioptric system of the eye and its correction.
See optics of the eye.
optogram Trace left on the retina by a retinal image due to the bleaching of rhodopsin.
optokinetic Term referring to movements of the eyes in response to the movement of objects across the visual field. Example: optokinetic nystagmus.
See reflex, vestibulo-ocular.
optokinetic drum; nystagmus test See test, optokinetic nystagmus.
optokinetic reflex See reflex, vestibuloocular.
optokinetoscope See test, optokinetic nystagmus.
optometer Instrument for measuring the refractive state of the eye. There are two main types of optometers: subjective and objective. Subjective optometers rely upon the subject’s judgment of sharpness or blurredness of a test object while objective ones contain an optical system which determines the vergence of light reflected from the subject’s retina. Electronic optometers in which all data appear digitally within a brief period of time after the operator has activated a signal can be of either type. Objective types (also called autorefractors or autorefractometers) have become very popular and several of these autorefractors are now providing both objective and subjective systems within the same instrument. Syn. refractometer.
See accommodation, objective; Analyser, Humphrey Vision; autorefraction; optometer, infrared; photorefraction; refractive error.
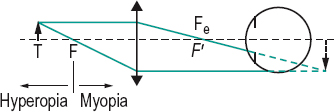
Badal’s o. A simple, subjective optometer consisting of a single positive lens and a movable target. The vergence of light from the target, after refraction through the lens, depends upon the position of the target. The patient is instructed to move the target towards the lens from a position where it appears blurred until it becomes clear. That point (converted in dioptric value) represents the refraction of the patient’s eye. This is a crude and inaccurate instrument, in which the measurement is marred by accommodation, variation in retinal image size with target distance, large depth of focus, non-linearity of the scale, etc. Badal’s improvement was to place the lens so that its focal point coincides with either the nodal point of the eye or the anterior focal point of the eye or the entrance pupil of the eye, thus overcoming the problems of the non-linear scale and the changing retinal image size (Fig. O3).
o. of Fincham, coincidence An objective optometer which forms the image of an illuminated fine line target on the retina by passing through a small, peripheral portion of the pupil. The examiner views through a telescope with an optical doubling system, which splits the visual field into two. If the incident beam of light is not in focus on the retina, the reflected beam will not be along the optical axis and the two half-lines will be seen out of alignment. Adjusting the dioptric value of the target in order to obtain alignment gives a measure of the ametropia.
infrared o. An optometer that uses infrared light rather than visible light. This is done so that the target used in the optometer is invisible to the patient. Otherwise when it is altered it tends to become a stimulus to accommodation. However, the instrument must be corrected for the chromatic aberration of the eye. Most modern optometers use infrared light. They are based on one of three principles: (1) retinoscopy, (2) Scheiner’s experiment, (3) ophthalmoscopy (indirect).
objective o.; subjective o. See optometer.
Young’s o. A simple optometer consisting of a single positive lens and using the Scheiner’s disc principle. The target is either a single point of light or a thread, which is moved back and forth until it is seen singly by the observer. When the target is out of focus, it is seen double and slightly blurred.
See experiment, Scheiner’s.
optometric physician See optometrist.
optometrist A person trained in the practice of optometry. The World Council of Optometry defines optometrists as ‘the primary healthcare practitioners of the eye and visual system who provide comprehensive eye and vision care, which includes refraction and dispensing, the detection/diagnosis and management of diseases in the eye, and the rehabilitation of conditions of the visual system’. Syn. ophthalmic optician (term used principally in the UK and the Republic of Ireland); optician-optometrist (term used in some European countries); optometric physician (term used in some US states, especially where therapeutic drugs are used).
optometry An autonomous, healthcare profession involved in the services and care of the eye and visual system, and the enhancement of visual performance. Syn. ophthalmic optics (term used principally in the UK and the Republic of Ireland).
See optometry, primary care.
behavioural o. A branch of optometry concerned with the diagnosis and treatment of visual problems taking into account not only the ocular history, signs and symptoms but also the whole person and his or her environment.
experimental o. The branch of optometry concerned with the scientific investigation of optometric problems by experimentation upon humans or animals, or by clinical research.
See psychophysics.
geriatric o. A branch of optometry concerned with the prevention, diagnosis and treatment of visual problems in old age.
paediatric o. A branch of optometry concerned with the prevention, development, diagnosis and treatment of visual problems in children.
primary care o. Term referring to the basic field of optometry to which patients usually come directly and are not usually referred by other professionals. Primary care optometric practitioners may refer some of their patients to other practitioners such as ophthalmologists, neurologists or to other optometric specialists for specialized services such as paediatric optometry, low vision aids or highly specialized aspects of contact lens fitting.
optotype Test type used for measuring visual acuity. See acuity, monotype visual; chart, Snellen; Jaeger test types; König bars; Landolt ring.
ora serrata The serrated anterior boundary of the retina located some 8 mm from the limbus. At the ora serrata, the retina is firmly adherent to the choroid, which is the reason why a retinal detachment ends here.
See ciliary body; retinal dialysis; stria.
orange Hue corresponding to wavelengths between 590 and 630 nm.
orbicularis muscle See muscle, orbicularis.
orbicularis ciliaris See ciliary body.
orbit A rigid bony cavity in the skull which contains an eyeball, orbital fat, the extraocular muscles, the optic nerve, nerves and blood vessels, lacrimal system and fibrous tissue of various kinds. This packing serves to keep the eyeball reasonably well fixed in place as it rotates. The orbital cavity has the approximate form of a pyramid. The walls of the orbital cavity are formed by seven bones. The medial wall of the orbit consists of: (1) the frontal process of the maxilla (maxillary); (2) the lacrimal bone; (3) the lamina papyracea of the ethmoid; and (4) a small part of the body of the sphenoid. The floor of the orbit consists of: (1) the orbital plate of the maxilla; (2) the orbital surface of the zygomatic (malar) bone and (3) the orbital process of the palatine bone. The lateral wall of the orbit consists of (1) the orbital surface of the greater wing of the sphenoid, and (2) the orbital surface of the zygomatic. The roof of the orbit is made up mainly by the frontal bone and behind this by the lesser wing of the sphenoid. The orbit is lined with a membrane of tissue called the periorbita (or orbital periosteum) which extends to the orbital margin (anterior rim of the orbit) where it becomes continuous with the periosteum covering the facial bones. The periorbita is loosely attached to the bones except at sutures, foramina and the orbital margin where it is firmly attached. The bones are much thicker at the margin (rim) than they are along the walls of the orbital cavity. There are many apertures and gaps in the orbit through which blood vessels and nerves pass (see Table O4).
See axis, orbital; canal, optic; fissure, inferior orbital; fissure, superior orbital; fracture, orbital; haemangioma, cavernous; lamina papyracea.
Table O3
Bones forming the walls of the orbit
| roof | medial wall |
| 1. frontal | 1. maxilla |
| 2. lesser wing of sphenoid | 2. lacrimal |
| 3. ethmoid | |
| 4. sphenoid | |
| floor | lateral wall |
| 1. maxilla | 1. greater wing of sphenoid |
| 2. zygomatic | |
| 3. palatine | 2. zygomatic |
orbital cellulitis See cellulitis, orbital.
orbital fat Fat (e.g. adipose tissue) which fills all the space not occupied by the other structures of the orbit (eyeball, optic nerve, muscles, vessels, etc.). It extends from the optic nerve to the orbital wall and from the apex of the orbit to the septum orbitale.
orbital fissure See fissure, inferior orbital; fissure, superior orbital.
orbital inflammatory syndrome See syndrome, orbital inflammatory.
orbital margin See orbit.
orbital optic neuritis See neuritis, optic.
orbital septum A thin membrane containing collagenous and elastic fibres which is attached to the orbital margin at a thickening called the arcus marginale. It is continuous with the tarsal plates of the upper and lower eyelids except where it is pierced by the fibres of the levator palpebrae superioris muscle in the upper lid and the expansion from the inferior rectus in the lower lid. Syn. palpebral fascia; septum orbitale.
Table O4
Orbital apertures
| aperture | location | contents |
| optic canal | at the apex (in lesser sphenoid) | optic nerve ophthalmic artery sympathetic nerve fibres |
| superior orbital fissure | at the apex (gap between greater and lesser sphenoid) | III, IV, V, VI nerves sympathetic nerve fibres ophthalmic vein recurrent lacrimal artery |
| inferior orbital fissure | between lateral wall and posterior part of the floor | infraorbital nerve zygomatic nerve branch of inferior ophthalmic vein nerve fibres from the pterygopalatine (sphenopalatine) ganglion to orbital periosteum |
| ethmoidal foramina (anterior and suture) | medial wall (frontal/ethmoidal post.) | ethmoidal vessels ethmoidal nerve/external nasal nerve |
| zygomatic foramen | lateral wall | zygomatic nerve and vessels |
| nasolacrimal canal | medial wall (maxilla/lacrimal) | nasolacrimal duct |
See dermatochalasis; eyelids; tarsus.
orbital tubercle A small elevation on the orbital surface of the zygomatic bone which serves as a point of attachment to the cheek ligament of the lateral rectus muscle, the ligament of Lockwood, the lateral palpebral ligament and aponeurosis of the levator palpebrae muscle.
orbitotomy A surgical incision made into the orbit to allow the removal of a tumour or foreign body, to treat a lesion, or to drain an abscess.
ordinary ray See birefringence.
organ of sight; organ, visual See eye.
organic Pertaining to a disorder in which there is a lesion within the body.
See functional.
organic amblyopia See amblyopia.
orientation column See column, cortical.
orthokeratology Programmed application of contact lens fitting for the purpose of altering the curvature of the cornea, especially to reduce the eye’s refractive power in myopia.
See lens, ortho-k.
orthophoria The case when the two visual axes are directed towards the point of binocular fixation, in the absence of an adequate stimulus to fusion. It represents a perfect balance of the oculomotor system; and the active and passive positions coincide, unlike in heterophoria. Syn. phoria.
See orthophorization; position, active; position, passive.
orthophorization A process that is presumed to operate to produce a greater frequency of nearly orthophoric conditions (in distance vision) than would otherwise occur on the basis of chance. This process may also operate after prolonged occlusion of one eye or after the introduction of prisms in front of one eye or both eyes.
See adaptation, vergence; emmetropization.
orthopic fusion See fusion, orthopic.
orthoptics The study, diagnosis and nonoperative treatment of anomalies of binocular vision, strabismus and monocular functional amblyopia.
orthoptist A person who practises orthoptics.
orthoscope A device by which water is held in contact with the cornea and thereby neutralizes the refractive power of the front surface of the cornea.
orthoscopic eyepiece See eyepiece, orthoscopic.
orthoscopic lens See lens, orthoscopic.
orthotropia 1. Absence of strabismus. 2. The term is sometimes used following successful surgery or prism compensation of a strabismus, or when there is a vertical deviation with no deviation in the horizontal plane.
oscillation, saccadic See flutter, ocular; myoclonus, ocular; opsoclonus.
oscillopsia Vision in which objects appear to oscillate. It may be due to acquired nystagmus, loss of vestibular function, neurosis, multiple sclerosis, in superior oblique myokymia, etc.
osmosis A passive process of movement of water through a semipermeable membrane in response to a concentration gradient, from an area of low solute (e.g. glucose molecules) concentration (i.e. high water concentration) to one of high solute concentration (i.e. low water concentration). The membrane is permeable to water but relatively impermeable to solutes.
See pressure, osmotic; solution, hypertonic.
osmotic pressure See pressure, osmotic.
osteogenesis imperfecta See keratoconus; sclera, blue.
ostium lacrimale See lacrimal apparatus.
Ostwalt curve See ellipse, Tscherning.
Ota’s naevus See naevus of Ota.
otitis media See syndrome, Gradenigo’s.
outer segment See cell, cone; cell, rod.
overaction Term referring to the excessive action of an extraocular muscle as a consequence of palsy or limitation to the ipsilateral antagonist or the contralateral synergist.
See Table M5.
overcorrection A term applied to a corrective prescription of slightly higher power than required. It has occasionally been suggested as an attempt to slow the progression of myopia.
See myopia control.
over-refraction Determination of a residual error of refraction of the eye while the patient is wearing spectacles or contact lenses.
overall size lens See lens, aniseikonic.
overcorrected spherical aberration See aberration, spherical.
overcorrection, postoperative See strabismus, consecutive.
overwear syndrome See syndrome, overwear.
oxidative stress A term used to describe the effect of oxidation in which an abnormal level of reactive oxygen species (ROS), such as the free radicals (e.g. hydroxyl, nitric acid, superoxide) or the non-radicals (e.g. hydrogen peroxide, lipid peroxide) lead to damage (called oxidative damage) to specific molecules with consequential injury to cells or tissue. Increased production of ROS occurs as a result of fungal or viral infection, inflammation, ageing, UV radiation, pollution, excessive alcohol consumption, cigarette smoking, etc. Removal or neutralization of ROS is achieved with antioxidants, endogenous (e.g. catalase, glutathione, superoxide dismutase) or exogenous (e.g. vitamins A, C, E, bioflavonoids, carotenoids). Oxidative damage to the eye, particularly the retina and the lens, is a contributing factor to age-related macular degeneration and cataract.
oxyblepsia See oxyopia.
oxybuprocaine hydrochloride A topical corneal anaesthetic, generally used in 0.4% solution. It may be used to carry out tonometry, gonioscopy, to remove a foreign body, etc. Syn. benoxinate hydrochloride. When used for applanation tonometry it is combined with 0.25% sodium fluorescein.
oxygen permeability The degree to which a polymer allows the passage of a gas or fluid. Symbol: Dk. Oxygen permeability (Dk) of a material is a function of the diffusivity (D) (that is the speed at which oxygen molecules traverse the material) and the solubility (k) (or the amount of oxygen molecules absorbed, per volume, in the material). Values of oxygen permeability (Dk) typically fall within the range 10–150 × 10–11 (cm2 ml O2)/(s ml mmHg). A semi-logarithmic relationship has been demonstrated between hydrogel water content and oxygen permeability. Unit: Barrer.
The International Organization for Standardization (ISO) has specified the permeability of contact lenses using the SI unit hectopascal (hPa) for pressure. Hence Dk = 10–11 (cm2 ml O2) /(s ml hPa). The former unit can be converted to this new SI unit by multiplying it by the constant 0.75. The ISO has established a classification of contact lens materials based on a range of values of oxygen permeability Dk. Group 1: 1–15; group 2: 16–30; group 3: 31–60; group 4: 61–100; group 5: 101–150; group 6: 151–200; group 7: 201–250; higher codes can be added in bands of 50.
See Barrer; oedema; oxygen pressure, equivalent; oxygen requirement, critical; refractometer.
oxygen pressure, equivalent (EOP) A percentage value of the assumed oxygen pressure existing behind a contact lens. The oxygen pressure in the air corresponds to about 20.9% (or about 159 mmHg; that value is actually close to 155 mmHg because of the presence of water vapour) and each percentage point is equal to a pressure of about 7.4 mmHg.
oxygen requirement, critical (COR) The minimum oxygen pressure at the epithelial surface required to prevent corneal swelling during the day. This value was initially assumed to be between 11 and 19 mmHg but it is nowadays considered to be at least 74 mmHg near the centre of the cornea (or 10% EOP or a Dk/L of about 25 × 10–9 (cm2 ml O2)/(s ml mmHg) at 25°C for daily wear. This figure increases to at least 90 × 10–9 for overnight wear. Syn. critical oxygen tension.
See hypoxia.
oxygen tension, critical See oxygen requirement, critical.
oxygen toxicity See retinopathy of prematurity.
oxygen transmissibility The degree to which oxygen may pass through a particular material of a given thickness. It is equal to the oxygen permeability divided by the thickness of the measured sample under specific conditions. Symbol: Dk/t. Unit: Barrer/cm. See hypercapnia; oedema; oxygen permeability; syndrome, corneal exhaustion.
oxyopia Extreme acuteness of vision. Syn. oxyblepsia.
oxyphenbutazone eye ointment A non-steroidal antiinflammatory agent usually used in 10% concentration for non-purulent inflammatory anterior eye conditions. It does not have the side effects of topical steroid therapy.





