13 Nutritional Requirements and Growth
Nutritional Requirements
Calories
Neonates need approximately 110 to 120 kcal/kg/d for appropriate growth. Calorie requirements steadily decrease to approximately 90 kcal/kg/d in toddlers. After 3 years of age, calorie requirements vary by gender, age, weight, and activity. Children with very low levels of activity, such as children with profound mental or motor disability who receive tube feedings, usually have significantly lower energy requirements than healthy children. When offered but not forced to take food, most infants and children are able to self-regulate their calorie, or energy, intake to optimal levels over time. Children are generally able to increase their calorie intake when needed, such as during brief periods of rapid weight gain in infancy and pubertal growth spurt and then decrease their intake back to appropriate levels for typical growth. If a toddler is gaining weight well, parents of picky eaters should provide healthy food options and can be reassured that the child is appropriately regulating his or her calorie intake (Figure 13-1).
Micronutrients
This section briefly discusses three of the most important micronutrients and the problems that can arise when they are deficient. Chapter 16 addresses these and other deficiencies in more detail.
Vitamin D
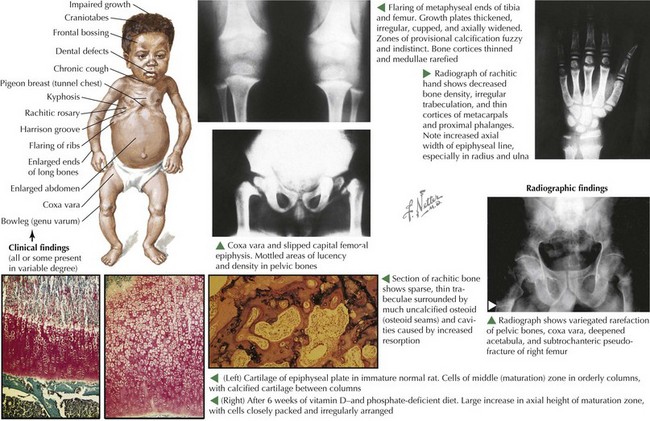
Adequate vitamin D intake is also important for long-term bone health, and recent research has shown its importance in a wide variety of other functions (Figure 13-2). Vitamin D can be ingested or synthesized when the skin is exposed to ultraviolet light. Vitamin D deficiency in infants causes rickets and when very severe can lead to hypocalcemic seizures. Vitamin D deficiency is relatively common in the United States. Risk factors include breastfeeding, darker skin, little sun exposure, and fat malabsorption. Infant formula is supplemented with vitamin D, but breastfed infants are at risk for rickets without vitamin D supplementation. Infants who are breastfed should receive a vitamin D supplement with 400 IU of vitamin D per day to prevent rickets. Children who do not receive at least 400 IU of vitamin D in their diets should also receive a supplement. Future research may show that the current recommendations for vitamin D are too low and should be revised.
Counseling
Infants
The AAP recommends breastfeeding for at least the first year of life, with exclusive breastfeeding for the first 6 months (Figure 13-3). Solid foods should be introduced at age 6 months, including iron-rich high protein foods and iron-fortified cereals and pureed fruits, vegetables, and meats. Infants diets can be slowly expanded to more complex textures as tolerated, always avoiding foods that could cause choking. When breastfeeding is not an option, infants should be given properly prepared commercial iron-fortified infant formula with introduction of solid foods between 4 and 6 months of age. Juice, with its high sugar content, should be avoided or limited to no more than 4 oz/d.
Children
Beverages
Fluids can be a good source of nutrients or a large source of empty calories. Recommended beverages change with age (Table 13-1). Parents should choose nutrient-rich liquids or water and avoid empty-calorie options such as soda.
Table 13-1 Recommended Fluids by Age for Healthy, Typically Growing Children
| Age | Fluid Recommendations |
|---|---|
| 0-6 months |
Growth
During well-child visits, assessment of growth serves as a screening tool for a wide variety of medical problems that may need further evaluation. In children presenting with an illness, assessment of growth can provide clues about the nature and time course of the illness. Because there is such wide variation in the distribution of normal growth, the challenge for clinicians is to determine whether children with unusual growth patterns are unhealthy or if they are healthy patients with a less common growth pattern. This segment focuses on how to assess growth and growth patterns seen in healthy patients. Further information on disorders of growth can be found in this section, as well as the chapter on disorders of growth in the endocrinology section (Chapter 73), and disease-specific chapters.
Use of Growth Curves
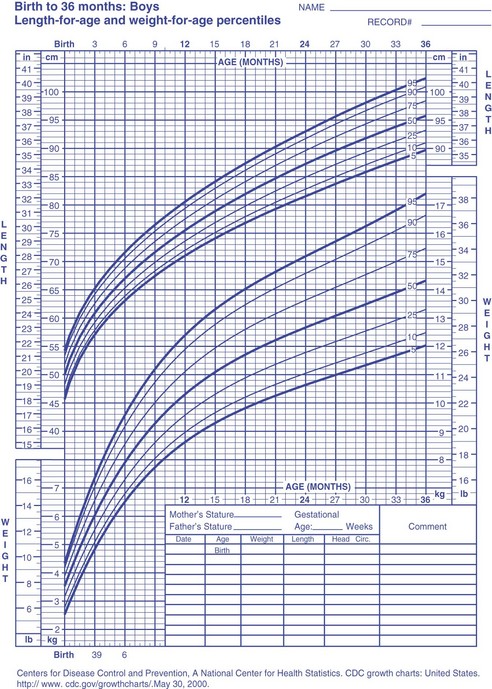
Growth in children is typically assessed by plotting a child’s measurement and age on a gender-specific growth curve (Figure 13-4). Growth curves allow clinicians to compare a child’s measurements with those of other children of the same age and to evaluate patterns in an individual child’s growth if measurements from multiple points in time are plotted on the same curve. On weight and BMI charts, the upper lines are not true percentiles; they have been adjusted so that the increasing prevalence of obesity does not lead to the classification of overweight children as having a healthy weight.
Assessing a Child’s Growth
Weight for Height and Body Mass Index
For infants and young children, weight relative to length can be evaluated with weight-for-length percentiles on the CDC 2000 or WHO growth curves or with the WHO curves for BMI. For older children, weight relative to height should be evaluated using BMI percentile. These charts are helpful when evaluating children who have familial short or tall stature. If these children are out of the normal range on the weight growth curve but have a normal weight for height, one can be reassured that their abnormal weight is likely proportional to their height. Overweight and obesity are discussed further in the Chapter 15.
Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(suppl 4):S164-S192.
Kleinman R, editor. Pediatric Nutrition Handbook, ed 6, Elk Grove, IL: American Academy of Pediatrics, 2009.
Kramer MS, Kakuma R. The optimal duration of exclusive breastfeeding: a systematic review. Adv Exp Med Biol. 2004;554:63-77.
Roche A. Human Growth. New York: Cambridge University Press; 2003.
Summerbell CD, Waters E, Edmunds L, et al: Interventions for preventing obesity in children. Cochrane Database Syst Rev (3):CD001871, 2005.
U.S. Preventive Services Task Force. Screening for Iron Deficiency Anemia—Including Iron Supplementation for Children and Pregnant Women: Recommendation Statement. Rockville, MD: Agency for Healthcare Research and Quality; 2006.