127 Nutritional Dermatoses
Clinical Presentation
Zinc Deficiency
Zinc is an element that is a required component of many enzymes involved in the synthesis and degradation of lipids, protein, and nucleic acid. Classic skin findings of zinc deficiency include erythematous and slightly eroded plaques involving the extremities, diaper area, and periorificial area. The facial involvement often involves the lower cheeks and chin but spares the skin above the upper lip, giving a “U” appearance. The rash can present with exudate, crust, vesicles, and bullae (Figure 127-1). Chronic zinc deficiency often manifests with lichenified plaques. Candida spp. and Staphylococcus aureus superinfections are common in this disorder. Other cutaneous findings of zinc deficiency include stomatitis, angular chelitis, blepharitis, nail-fold inflammation with possible nail dystrophy, and hair thinning with areas of complete alopecia. In addition to dermatitis, diarrhea is a commonly associated symptom. The severity is highly variable and does not correlate with the development of cutaneous findings. Children with zinc deficiency also characteristically are irritable, have problems eating and sleeping, and are growth impaired.
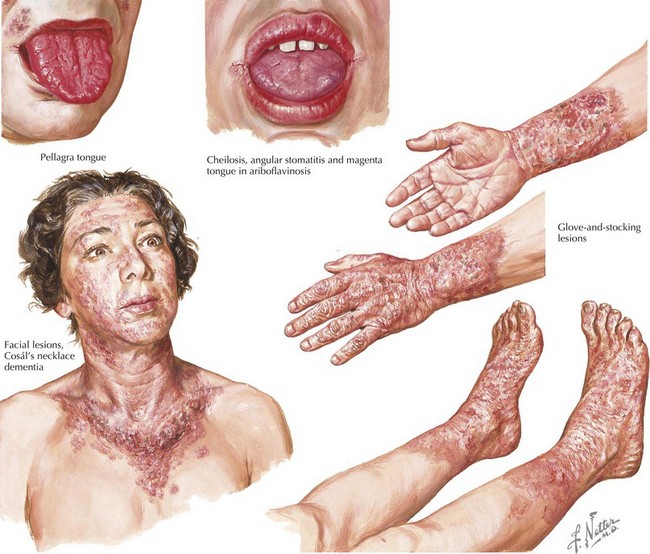
Niacin Deficiency
Niacin is a water-soluble nutrient that is part of the vitamin B complex. Deficiency of niacin, also known as vitamin B3, leads to pellagra. The classic skin manifestations of pellagra are symmetric erythema typically occurring on sun-exposed sites associated with itching and burning that can form blisters and crusts after sunlight exposure. The lesions later become coarse, dry, and hyperpigmented. On the upper chest, keratotic hyperpigmented plaques associated with pellagra are commonly known as Casal’s necklace. Oral findings include edema, atrophic glossitis, and stomatitis (Figure 127-2). Patients with niacin deficiency also develop GI symptoms, such as abdominal pain, vomiting, and diarrhea, and neurologic complaints, such as vertigo. Although the symptoms of pellagra are often summarized into the three Ds—dermatitis, diarrhea, and dementia—the full spectrum of the disease is not usually seen during the early stages and is rare in pediatric patients. Although niacin is found in most foods, it is not absorbed well from corn, and thus children whose diet is almost entirely corn are at high risk of developing pellagra. Tryptophan can be converted to niacin in the body; therefore, conditions associated with tryptophan malabsorption increase the risk of developing pellagra-like symptoms. Hartnup’s disease is a genetic condition in which patients have a genetic mutation in the neutral amino acid transporter gene (SLC6A19), resulting in poor intestinal tryptophan absorption and the potential for developing symptoms of pellagra. Drugs such as isoniazid and 5-fluorouracil that inhibit the conversion of tryptophan to vitamin B3 or phenytoin that can decrease total serum tryptophan also increase susceptibility to development of pellagra.
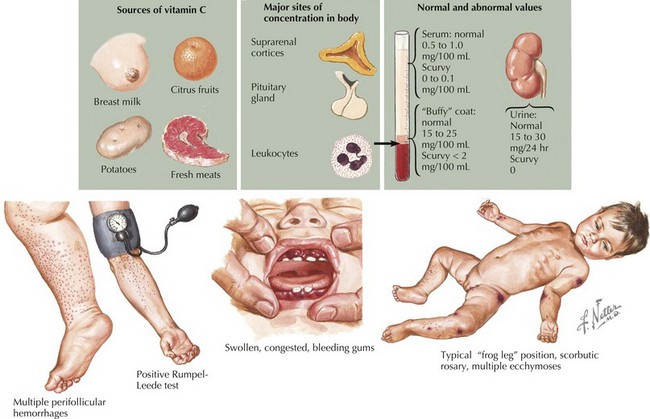
Vitamin C Deficiency
Vitamin C, also known as ascorbic acid, is commonly found in fresh fruit and vegetables. Scurvy, a deficiency in vitamin C, occurs in children almost exclusively because of poor dietary habits or if parenteral nutrition is exposed to light for too long because ascorbic acid is broken down by light. Follicular hyperkeratosis and abnormally curly hairs known as corkscrew hairs typically on the forearms, legs, and abdomen are observed in patients with scurvy. Other characteristic skin findings are perifollicular hemorrhage, ecchymoses, loosening of teeth, gingival hyperplasia, and bleeding gums (Figure 127-3). Subperiosteal bleeding can cause epiphyseal separation, resulting in a paucity of spontaneous limb movements (pseudoparalysis). Vitamin C is important in collagen biosynthesis; however, the mechanism of bleeding susceptibility in scurvy is not entirely known.
Heath ML, Sidbury R. Cutaneous manifestations of nutritional deficiency. Curr Opin Pediatr. 2006;18:417-422.
Maverakis E, Fung MA, Lynch PJ, et al. Acrodermatitis enteropathica and an overview of zinc metabolism. J Am Acad Dermatol. 2007;56:116-124.
Ruiz-Maldonado R, Orozco-Covarrubias L. Nutritional diseases. In Bolognia JL, Jorizzo JL, Rapini RP, editors: Dermatology, ed 2, St. Louis: Elsevier, 2008.