4 Nutrition
Dietary requirements
Energy
Protein
Protein contains many amino acids.
Fat
Dietary fat provides 37 kJ (9 kcal) of energy per gram. A high fat intake has been implicated in the causation of cardiovascular disease, cancer (e.g. breast, colon and prostate), obesity and type 2 diabetes. It is suggested that the consumption of saturated fatty acids should be reduced, accompanied by an increase in monounsaturated fatty acids, e.g. oleic acids (the ‘Mediterranean diet’), or polyunsaturated fatty acids, e.g. linoleic acid. Any increase in polyunsaturated fats should not, however, exceed 10% of the total food energy, particularly as this requires a big dietary change.
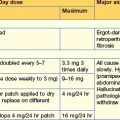
The current recommendations for fat intake for the UK are as follows:
Protein–energy malnutrition
The majority of the weight loss, leading to malnutrition, is due to poor intake secondary to the anorexia associated with the underlying condition. Disease may also contribute by causing malabsorption and increased catabolism, which is mediated by complex changes in cytokines, hormones, side-effects of drugs and immobility. The elderly are particularly at risk of malnutrition because they often suffer from diseases and psychosocial problems such as social isolation or bereavement.
Clinical features
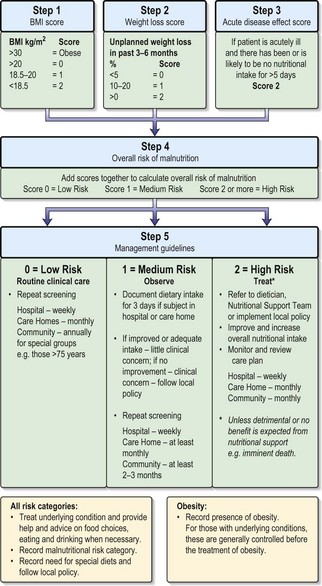
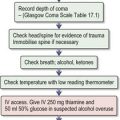
Patients are sometimes seen who have loss of weight or malnutrition as the primary symptom (failure to thrive in children). Mostly, however, malnourishment is only seen as an accompaniment of some other disease process, such as malignancy. Severe malnutrition is seen mainly with advanced organic disease or after surgical procedures followed by complications. Three key features that help in the detection of chronic PEM in adults are described below. These features are also used in the Malnutrition Universal Screening Tool (see Fig. 4.1):
Nutritional support in the hospital patient
Nutritional requirements for adults
Table 4.1 Daily dietary electrolyte and trace element requirements
| Electrolyte/trace element | Daily requirement |
|---|---|
| Na+ | 70–220 mmol |
| K+ | 60–120 mmol |
| Mg2+ | 5–20 mmol |
| Ca2+ | 15–20 mmol |
| Zn2+ | 50–100 µmol |
| Mn2+ | 120 µmol |
| Fe2+ | 70 µmol |
| Cu2+ | 20 µmol |
| Cl− | 70–220 µmol |
| PO−3 | 15–25 µmol |
| F− | 50 µmol |
| I− | 1 µmol |
Table 4.2 Daily requirements of fat-soluble and water-soluble vitamins
| Vitamin | Daily requirement |
|---|---|
| Fat-soluble | |
| A (retinol) | 700 mcg |
| D (cholecalciferol) | No dietary intake required (if fully ambulant) |
| K | 1 mcg/kg body weight |
| E (α-tocopherol) | 10 mg |
| Water-soluble | |
| B1 (thiamin) | 0.4 mg per 1000 kcal |
| B2 (riboflavin) | 1.3 mg |
| Niacin | 6.6 mg per 1000 kcal |
| B6 (pyridoxine) | 15 mcg per g of dietary protein |
| B12 (cobalamin) | 1.5 mcg |
| Folate | 200 mcg |
| C (ascorbic acid) | 40 mg |
Enteral nutrition (EN)
Feeds can be given by various routes:
Box 4.1 Enteral feeding via nasogastric tube
The procedure should be explained to the patient and consent taken.
Procedure
Diet formulation
A polymeric diet with whole protein and fat can be used (Box 4.2), except in patients with severely impaired gastrointestinal function who may require a predigested (i.e. elemental) diet. In these patients, the nitrogen source is purified low-molecular-weight peptides or amino acid mixtures, with the fat sometimes being given partly as medium-chain triglycerides. Appropriate diets can be used for patients with, for example, chronic kidney disease (low protein) or anorexia (e.g. high-nitrogen or high-calorie diets).
Parenteral nutrition
Total parenteral nutrition via a central venous catheter (TPN)
A silicone catheter is placed into a central vein, usually using the infraclavicular approach to the subclavian vein (Box 4.3). The skin-entry site should be dressed carefully and not disturbed unless there is a suggestion of catheter-related sepsis.
Box 4.3 Central catheter placement for parenteral nutrition
Give an explanation and obtain consent from the patient.
Nutrients
Nitrogen source
Most patients receive at least 11–15g N per day, in the form of synthetic L-amino acids.
Administration and monitoring
| Constituent | Amount | |
|---|---|---|
| Peripheral: all mixed in 3 L bags and infused over 24 hours | ||
| Nitrogen | L-amino acids 9 g/L | 1 L |
| Energy | Glucose 20% | 1 L |
| Lipid 20% | 0.5 L | |
| + Trace elements, electrolytes, water-soluble and fat-soluble vitamins, heparin 1000 U/L and hydrocortisone 100 mg; insulin is added if required. Nitrogen 9 g, non-protein calories 7206 kJ (1700 kcal) | ||
| Central: all mixed in 3 L bags and infused over 24 hours | ||
| Nitrogen | L-amino acids 14 g/L | 1 L |
| Energy | Glucose 50% | 0.5 L |
| Glucose 20% | 0.5 L | |
| + Lipid 10% | 0.5 L Fractionated soya oil 100 g/L, soya oil 50 g, medium-chain triglycerides 50 g/L |
|
| + Electrolytes, water-soluble and fat-soluble vitamins, trace elements, heparin and insulin may be added if required. Nitrogen 14 g, non-protein calories 9305 kJ (2250 kcal) | ||