Chapter 42 Nonpharmacologic Control of Pain
 Introduction
Introduction
When treating a patient for pain, the clinician must first determine the primary cause, the pathogenesis, and the secondary or contributing factors. The relief of pain may then be achieved by removal of the primary cause (e.g., cure of an infection), neutralization of the effect of the stimulus (e.g., emollients for an ulcer), relief of discomfort (e.g., biofeedback), suppression of the disease process (e.g., anti-inflammatory agents), and dulling or obliteration of the sense of pain (e.g., analgesics or acupuncture).1
 The Experience of Pain
The Experience of Pain
A Psychological Model
In the psychological model, the brain infers information from bodily signs and integrates it with existing personal and situational variables to direct behavior. When consideration must also be given to the interactions with interested observers, such as physicians, family members, and birth attendants, who influence the interpretation with their own experiences and attitudes about pain, the complexity becomes even greater.
According to this model, which does not differ in essence from a general model of stress, a primary appraisal of the personal danger or threat posed by the painful stressor is followed by a secondary appraisal of one’s ability to cope, based on emotional feedback and contributions of situational and sociocultural response factors. On this basis, a woman in labor could choose to regard pain as “positive,” “functional,” or “creative”; “pain with a purpose”; or, alternatively, “part of a process involving injury.”2 In the course of a pain management program carried out in 84 patients with low back pain, those who more strongly endorsed “organic” concepts about the nature and treatment of pain reported higher levels of disability, whereas reductions in reported “organic” pain beliefs improved reported disability, and endorsement of “psychological” concepts about the nature and treatment of pain was not associated with disability.3 Several studies indicated that “catastrophizing” predicted pain or was associated with lower pain tolerance.4,5 This conceptualization of painful stress suggests that intervention could be successful at several levels: cognitive patterning, physiologic arousal associated with emotional stress, and control of environmental stimuli. Examples of appropriate strategies are cognitive coping skills such as restructuring and utilization of preparatory information and attention shifts; muscular relaxation, physical or electrical stimulation, and biofeedback techniques; and structuring of the environment in a way conducive to effective coping (such as by making it nonthreatening and comfortable).6
Neuropsychological Mechanisms of Pain
According to research on the mechanisms of pain, pain can be treated not only by anesthetic blocks, surgical intervention, and the like, but also by influencing the motivational, affective, and cognitive factors.7 The traditional specificity theory of pain, first enunciated by Descartes in the seventeenth century, holds that pain messages are conducted from specific pain receptors at the periphery through discrete pathways to pain centers in the brain. However, there are individual differences in pain responses; pain is not consistently stopped by cutting or blocking of the “pain pathway,” and it is now known that nonpainful types of stimulation activate the A-δ and C fibers (see next paragraph) that are associated with pain. Therefore, later modifications of pain theory took into account patterning of nerve impulses over time to reflect differences in degree and intensity of stimuli and summation of signals from an extended area.8
The currently accepted view of pain is the gate control theory, which Melzack and Wall9 formulated in 1965. Based on neurologic data and a categorization of the words used to describe pain, this theory conceptualizes the pain experience as having sensory discriminative, motivational affective, and cognitive evaluative components or modalities, corresponding to different patterns of nervous impulses. Neurologically, a specialized cluster of nerve cells in the substantia gelatinosa of the spinal column is thought to operate like a valve or gate, controlling nerve signals before they evoke the perception of, and response to, pain. Besides this monitoring of sensory data in the central nervous system, gating is also influenced by the relative amount of activity in large (A-β) and small diameter (A-δ and C) nerve fibers. The large fibers tend to inhibit transmission, or close the gate, preventing pain, and the small fibers tend to facilitate transmission, or open the gate, resulting in pain. The fact that large fibers are activated by pressure, touch, massage, and vibration suggests a mechanism for such pain control techniques as acupressure, acupuncture, and transcutaneous electrical nerve stimulation (TENS). Such stimulation apparently closes the spinal gate via the large fiber system. Melzack and Casey7 expanded this theory by proposing the possibility of a higher level gate, in the reticular or limbic structures of the brain, that probably mediates the drive to escape from unpleasant stimuli. At central nervous system levels, the biochemical mechanisms of gate control may involve the endorphins, natural morphine-like substances that have been implicated in the pain controlling effects produced by acupuncture.10
Pain in Childbirth
A psychological and/or social learning approach to pain emphasizes control of motivation, expectation, focus of attention, stress, and feelings of anxiety, depression, and helplessness. Factors specifically operative in labor pain involve these as well as social support and the physiologic factors of hunger, rest, and muscular tension.11All of these factors can contribute to the interpretation of pain being placed on the nociceptive message provided by uterine contractions. The influence of motivation on labor pain was effectively demonstrated in a prospective study of maternal attitudes toward pregnancy in 8000 American women. One of the factors found to be strongly related to maternal attitude toward having a baby was the need for analgesics in labor.12
Cultural conditioning may also be fundamental to the labeling of childbirth as painful. Throughout most of the world, analgesics are not required for labor; a Japanese anesthesiologist suggested that the idea of “painless delivery” is a strange one to his culture.13 American women, in contrast, “live through a largely self-fulfilling prophecy of birth as a painful, terrifying ordeal, and/or as a medical, drugged process over which they have no control.”11 This idea relates to body fantasies of injury, brought about in a hospital environment where distress is an expected response to the expulsive reflex.2
 Pain Control
Pain Control
Moderating Variables and Psychological Techniques
Psychological Strategies
For example, on the repression–sensitization axis, repressors may be characterized as people who avoid having to cope with pain. Sensitizers, however, have an obsessive need to cope; they like to be informed in advance about the situation and to have control over it. The superior initial tolerance exhibited by repressors in response to heat and pressure stimuli disappeared in repeated trials, showing that the sensitizers’ predilection for challenge enabled them to endure long-term pain better.
The importance of individual difference variables is also illustrated by the observation that one third of patients undergoing surgical operations do not request pain-killing medication.23 This common ability to suppress pain indicates that not all surgical patients consider themselves passive victims. During the postoperative period, pain persists longer for those who accept medication.
Cognitive Strategies
The impetus for devising cognitive strategies to promote tolerance of pain has been particularly supported by investigations showing that pain tolerance increases with greater predictability and perception of control.24–28 Similarly, preparatory communications and information received before the onset of experimental or surgical pain consistently decreases the subjects’ perception of pain.29–31 Animal studies have demonstrated higher rates of instrumental responses when painful shocks are signaled than when they are unsignaled.32 Kanfer and Seidner33 found that subjects who could advance slides of travel pictures at their own rate tolerated ice water immersion of the hand longer than yoked subjects whose slides were changed by the experimenter.
When surgical patients were given a sense of control by being provided with preparatory information about postoperative discomforts and operative care, in combination with training in rehearsal of realistic, positive aspects of the surgical experience, they showed a significant reduction in postoperative anxiety (as indicated by nurses’ observations), requests for sedatives, and length of hospital stay.34
A typical cognitive behavioral procedure utilizes “stress inoculation,” beginning with an educational phase (in which the client is given a conceptual framework for understanding the nature of his or her stressful reactions), followed by rehearsal of behavioral and cognitive coping skills, based on a set of coping self-statements generated by the client in collaboration with the therapist. Such cognitive-behavioral techniques, sometimes in combination with electromyographic biofeedback control, have been found successful in treatment of chronic low back pain.35–37 Also, cognitive-behavioral strategies have been effective in alleviating the pain of irritable bowel syndrome,38 temporomandibular joint syndrome,39,40 cancer,41 migraine headaches,42 rheumatic conditions,43–45 fibromyalgia,46 and complex regional pain syndrome.47 This emphasis on conceptualization, preparatory information, and cognitive transformation seems to have been incorporated into the Read method of natural childbirth, which replaces fear with knowledge about birth.12 Sheila Kitzinger,2 in her method of prepared childbirth, similarly emphasizes the necessity of “acquiring knowledge and understanding of what labor involves, the terminology used by obstetricians and midwives, and information about what happens in hospitals.”
A study by Stevens and Heide48 conducted at the University of Wisconsin used iced water to test perception and endurance of pain in subjects who had been taught methods used in childbirth education classes. Control subjects for this training and an additional control group were offered only distraction during the tests. Those who had been taught the techniques reported only about half the pain of that reported by control subjects and endured it 2.5 times longer. The prepared childbirth strategies improved with practice, were effective for pain lasting longer than most contractions in labor, and were more effective than distraction techniques.48
Attention-Focusing
Distraction or focused attention, mostly utilizing the rhythms of the breath, is essential to the Lamaze method, the most popular prepared childbirth program in America, and is important in the Bradley and other methods. Sheila Kitzinger2 described the controlled attention focusing as:
Stevens and Heide48 found that attention-focusing functions effectively as an analgesia for labor pain. Such strategies are strongly supported by much psychological research. Hospitalized children with chronic illnesses who were taught distraction techniques were able to reduce measures of distress before and during medical procedures such as intramuscular and intravenous injections.49 In a study of patients with burn pain, sensory-focusing techniques were more successful than distraction techniques in controlling pain, and both were more successful than standard care.50 The focus may be on a competing response, as in a study by Kanfer and Goldfoot,51 which showed that when attention was directed to self-presented external slides, individuals were able to increase their tolerance of the pain of cold water. Focus on a competing response was also shown in the use of hypnosis as an analgesic and in the meditative states of Raj yogis, who pinpointed attention on the tip of the nose or a point on the back of the skull, and then did not react physiologically to cold water, bright lights, or sudden sounds.52,53 Other adepts in unusual feats of pain tolerance, such as having spikes stuck through the skin, either maintained an unfocused attitude, without evaluation, or pinpointed attention totally on the pain, but without evaluation.54 In such cases, the attitude of detachment from the pain can be reflected by an undisturbed electroencephalography (EEG) pattern of α- or β-waves throughout performance of the feat.
Relaxation Training
Relaxation training, another essential element of pain control, is found in all childbirth training programs. A considerable body of literature supports its importance in pain control, because a state of lowered autonomic arousal is incompatible with anxiety. Although progressive muscular relaxation, systematic desensitization, and autogenic training are all well-established physiologic approaches to muscular relaxation, meditation traditions provide quicker methods to achieve what Benson55 called the “relaxation response.” One of the simplest meditation practices—maintaining a focal awareness of the flow of the breath—is taught by Rahima Baldwin11 in Special Delivery and is identical to the ancient Buddhist practice of vipassana, or insight meditation.
Hypnosis
Hypnosis or autohypnosis is another method utilized to induce deep relaxation for pain control. It incorporates many of the therapeutic elements already referred to—focused attention, positive expectation, and a supportive or permissive attitude—in making suggestions that alleviate anxiety. Thus, its success in pain management may be viewed from a cognitive-behavioral perspective.56 In one technique, “glove anesthesia” is induced in one hand and the “numb, heavy wooden feeling” so produced is transferred to the other hand, the face, and eventually to the abdomen to “relieve the discomfort” of uterine contractions (the word “pain” is never used, because its use would be countersuggestive).57 Pain modulation in “highly hypnotizable” subjects has been confirmed through brain measurement of somatosensory event-related potentials to noxious stimuli, with highest amplitudes for these subjects recorded at frontal and temporal scalp sites.58
Counterstimulus Methods: Massage, Acupuncture, Transcutaneous Electrical Nerve Stimulation
The hand reflexology method of grasping combs during labor to activate points on the fingertips and balls of the hand that relate to uterine functioning is one example of counterstimulus strategy.11 Foot reflexology, acupressure, acupuncture, and TENS might also share a common autonomic nervous mode of operation.
Transcutaneous Electrical Nerve Stimulation
In a controlled study of experimentally induced cold-pressor pain, the effect of electrical stimulation with TENS electrodes at two traditional acupoints in 20 subjects had an analgesic effect with statistical significance comparable to that of morphine, and the combined effect of TENS with morphine was stronger than TENS alone.59 A series of controlled randomized double-blind studies on carpal tunnel syndrome pain found that the combination of low-level laser and microcurrent TENS on distant and local points significantly decreased McGill Pain Questionnaire Score, sensory and motor latencies, and Phalen and Tinel signs, compared with sham treatment.60 A British study, investigating the relative hypoalgesic effects of different TENS parameters upon experimentally induced mechanical pain, found that low-frequency, high-intensity, extrasegmental stimulation (i.e., over an acupuncture point rather than over a nerve distribution) produced a rapid-onset hypoalgesic effect, which increased during the stimulation period and was sustained for 30 minutes after stimulation.61
The selection of this area for stimulation is based on Bonica’s account of the neurologic mechanism of delivery pain.62 During the first stage, pain receptors are assumed to be activated by contractions of the uterus and dilation of the cervix. The evoked impulses are mediated in afferents that run in the hypogastric nerves and reach the spinal cord via the dorsal roots T10-L1. The pain is referred to large areas of the abdomen and back. During the second stage, pain is also caused by distention and stretching of the delivery canal, the pelvic floor, the vulva, and the perineum. The pain is localized, and the impulses reach the spinal cord mainly via the pudendal nerves and the dorsal roots S2-S4. The pain during the first stage is characterized as an ache considered to be mediated in small-diameter C fibers. During the second stage, the pain has the more localized intensive nature usually identified with the δ-afferent fibers.62,63
In the typical application of this technique for control of pain during labor, low-intensity stimulation is given continuously and a high-intensity stimulation can be initiated by the parturient herself whenever pain increases. Stimulation via the thoracic electrodes is maintained throughout the delivery at an amplitude that is maximal for a pleasant sensation, whereas sacral stimulation is added from the later part of the first stage. Table 42-1 summarizes the uniformly good results that have been reported.
TABLE 42-1 The Results of the Use of Transcutaneous Electrical Nerve Stimulation for Pain Control in Labor
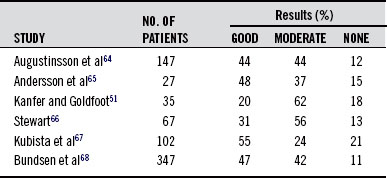
Those patients who complained of backache have especially appreciated it. An Austrian study compared the analgesic effects of TENS, pethidine, and placebos on labor pain in 30 parturient women during the first stage of labor. Patients who received pethidine and those who were given TENS experienced considerable relief of pain.69 A 1996 review of 30 studies on TENS stimulation of acupuncture points in labor substantiated the conclusions of earlier research.70
In view of the relatively good results and lack of complications, the consensus of all the preceding studies is that the TENS method is recommended as a primary pain-relieving measure, to which conventional methods can be added as needed. Robson71 commented that TENS is noninvasive and is believed to be safe for both mother and baby. It is easy to apply and can be operated throughout labor by the doctor, midwife, father, or mother. Augustinsson et al64 were most impressed by the lack of complications, because the conventional methods, including analgesic and sedative drugs, nitrous oxide inhalation, epidural anesthesia, and local blockades, all possess a varying level of potential risk.64 Another advantage is that TENS, because it does not give complete analgesia, does not eliminate pain as a diagnostic tool; it can be interrupted whenever needed for clinical evaluation. More important, perhaps, from the point of view of the woman in labor is the fact that her consciousness is not altered to the point of excluding her own active participation in and experience of the delivery.
Acupuncture
Hundreds of studies have investigated the efficacy and mechanisms of acupuncture analgesia for acute and chronic pain in surgical operations and in childbirth. In a review article of 24 studies, Lewith and Machin72 found that the typical clinical trial showed a 70% efficacy of acupuncture compared with placebo treatment. Reichmanis and Becker73 found similar results in a review of 17 studies of acupuncture analgesia in experimentally induced pain. On the basis of a thorough review of the clinical and experimental research on acupuncture pain control, Stux and Pomerantz74 concluded that acupuncture analgesia helped from 55% to 85% of patients with chronic pain, comparing favorably with the effects of potent pain medication (such as morphine, which is 70% effective), and clearly distinct from the placebo effect, which helped 30% to 35%. At the same time, somatosensory EEG–evoked potential studies provided objective evidence of the analgesic effect of acupuncture.75–77
Recent randomized and double-blinded controlled studies demonstrated clinical effectiveness of acupuncture in treating chronic lateral epicondylitis78 and chronic neck pain.79 In the neck pain study, stimulation at distant points of the neck-related meridians were more effective than sham acupuncture points and “dry needle” injections of local myofascial trigger points, reducing motion-related pain by one third after a single treatment. A single-blind randomized controlled trial showed that electroacupuncture (EAP) was superior to manual acupuncture in treating patients with tennis elbow.80 A review article on treatment of fibromyalgia pain for patients at a hospital in Brazil showed improvement with traditional acupuncture, measured on subjective scales and number of tender points.81 Preoperative EAP led to reduction in intraoperative and postoperative requirement of analgesic medications (alfentanil and morphine) in patients receiving gynecologic lower abdomen surgery.82 Surgery that requires general anesthesia in Western countries is routinely performed in Chinese hospitals with the combination of acupuncture and local anesthesia for pain control, providing a considerable decrease in risk for surgical patients.
In their own study of acupuncture analgesia for normal delivery, Hyodo and Gega13 tested 32 patients, equally divided between primaparas and multiparas. Low-frequency electrical current was introduced through needles at LI-4, ST-36, and SP-6, a standard therapeutic repertory for sedation of the reproductive organs. The results were assessed from relief noted by the patient (subjective scale) as well as from the obstetrician’s observation (objective scale); among the primiparas, 62.5% found good or excellent effect on the subjective scale, and 62.6% good or excellent on the objective scale; and among the multiparas, 93.8% subjective relief and 93.7% objective relief were seen. Overall, 90% of the patients experienced relief of pain within 20 minutes of initiation of acupuncture anesthesia. These researchers noted the considerable disparity in reports of effectiveness of acupuncture from Japan and America, explaining it as a novelty effect. It is natural that in Japan, where no analgesic methods are normally used, the scoring in favor of acupuncture would be high compared with that in America.
Hyodo and Gega13 concluded that acupuncture analgesia is useful for delivery, especially because of its safety, although its results are more erratic and less potent than those of conventional anesthetic techniques. More recently, a randomized controlled trial investigating acupuncture treatment as a complement or an alternative to conventional analgesia for labor in a Swedish hospital found that acupuncture significantly reduced the need for epidural analgesia, and parturients receiving acupuncture achieved a better extent of relaxation than the control group.83
One of the most influential and controversial studies of acupuncture over the past decade has been the so-called “German Acupuncture Trials “(GERAC) for chronic low back pain. This double-blind, randomized controlled trial involved 340 outpatient practices and included 1162 patients. Treatment according to principles of traditional Chinese medicine was compared with “sham” acupuncture, consisting of superficial needling at nonacupuncture points, and with conventional therapy (combining drugs, physical therapy, and exercise). After 6 months, effectiveness of acupuncture, whether true (47.6%) or sham (44.2%), measured on scales grading pain and functional ability, was almost twice that of conventional therapy (27.4%). Statistical significance level wasP <0.001. The controversial issue in this study was whether the method of “sham” acupuncture applied was an adequate control, considering that insertion of acupuncture needles at nontraditional points apparently produced acupuncture effects, including the possible mechanism of stimulation of endogenous opiates.84
A considerable amount of research has focused on determining a mechanism for acupuncture analgesia. A 1995 review of studies on acupuncture effects in pain and disease pointed out that, like exercise, acupuncture produces rhythmic discharges in nerve fibers and causes the release of endogenous opioids and oxytocin. Furthermore, “experimental and clinical evidence suggests that acupuncture may affect the sympathetic system via mechanisms of the hypothalamic and brain-stem levels.”85 Animal studies continue to demonstrate that acupuncture analgesia is mediated in the central and peripheral nervous systems by opioid peptides.86–88 The cortex and hippocampus appear to participate in the modulation of chronic pain, and the analgesic action of EAP seems to operate along this pathway.89 A study carried out on dogs seemed to verify the traditional theory of points of tonification and sedation, through differential production of sympathomimetic and parasympathomimetic effects on the cardiovascular system upon stimulation of different points. Carlsson,88 a Swedish researcher, concluded that a mechanism for therapeutic acupuncture must include peripheral events that release neuropeptides, spinal mechanisms such as gate control, and supraspinal mechanisms through the descending pain inhibitory system, the sympathetic nervous system, and the hypothalamic-pituitary-adrenal axis. He cautioned that much of animal and human experimental acupuncture research shows only short-term hypoalgesia; that almost all such experimental research has been performed with EAP rather than the more gentle manual style of therapeutic acupuncture; and that pain threshold elevation in human experimental research does not necessarily predict the clinical outcome.
In a study of labor induction and inhibition by EAP, Tsuei et al89 utilized SP-6 and SP-4 points, which are located in the territory of the L4 dermatome. The spleen meridian, to which these loci belong, runs across the dermatomes of L4, L5, L2, and L1, and then upward from T12 to T5. Because the sympathetic nerve controlling the uterus through the pelvic plexus receives preganglionic fibers from T5 to L4, Tsuei et al89 concluded that it is highly possible that stimulation of the electropermeable loci within this area may alter the physiologic function of the uterus. The LI-4 points of the upper extremities, often added to the spleen meridian points in the acupunctural control of labor pain, perhaps represent the central approach to the autonomic nervous system, because these loci control pain to the head and neck. It should be noted, however, that Motoyama,90 who attempted to verify the traditional subtle anatomy of meridian pathways through tests of electrocutaneous resistance at meridian points, claimed that these effects could not be adequately explained in terms of the conventional sympathetic dermatomes but instead imply an alternative bioelectric transmission system.
The discovery of the head McKenzie sensory zones showed the possible mediation of the invisible meridians and points of traditional Eastern medicine between internal organs and corresponding skin areas. Nakatani91 was able to detect the electropermeable line as an apparent viscerocutaneous autonomic nerve reflex when organic diseases were involved. Hyodo92 explained acupuncture stimulation as the transmission of impulses centrally from the reactive electropermeable loci via a sympathetic afferent fiber, and that the autonomic nerve in the viscera is stimulated to response by the reverse of the McKenzie theory. An exciting recent development in acupuncture research has been the finding by functional neuroimagery of neuronal correlates of acupuncture stimulation in the human brain. In a controlled study of EAP stimulation of GB-34 on the left leg, real EAP elicited significantly higher activation over the hypothalamus and primary somatosensory motor cortex than mock and minimal EAP, showing that the hypothalamic-limbic system was significantly modulated by EAP at acupoints.93
Other Methods
The scope of this chapter does not permit detailed discussion of other promising methods of pain control, but mention can be made of massage, biofeedback, and nutritional and botanical agents for treatment of pain. A literature search led to the conclusion that massage, particularly acupressure, is effective for low back pain, especially when it is combined with exercises and education, with beneficial effects lasting at least 1 year after the end of treatment.94 A vast amount of literature is available on biofeedback training for pain. An article suggesting a future direction in pain medicine described the use of “off-the shelf,” low-cost, and low-bandwidth telemedicine equipment to deliver clinical biofeedback treatment when the patient and provider are in two different locations.95 In a randomized double-blind trial of 30 patients with chronic maxillofacial pain, significant reduction in pain scores and improvement in tolerance of experimentally induced dental pain were achieved with administration of 3 g daily of the amino acid tryptophan and a high-carbohydrate, low-fat, low-protein diet in comparison with placebo.96 Among botanical agents for pain, corydalis rhizome or tuber (yanhusuo) is well known in the Chinese materia medica for its analgesic effect, containing combined alkaloids found to be 40% as effective as morphine. Acting probably through inhibition of the reticular activating system, corydaline was shown in one clinical study to decrease or relieve pain in 32 of 44 patients with dysmenorrhea.97
 Summary
Summary
This chapter has presented many of the current nonpharmacologic strategies for control of pain. Because the mechanism of pain perception has been shown to involve both physiologic and psychological components, the optimal treatment might combine psychological factors, such as preparatory information, attention focus, relaxation, and supportive communication, with the physical stimuli of TENS or acupuncture. Such a multidisciplinary approach to patients with chronic back pain was evaluated after a 4-week program that included back schooling, psychological intervention, and treatment by acupuncture, chiropractic, the Alexander technique, and a pain specialist. Significant improvement was maintained for a period of 6 months.98
Dental researchers of the Pediatric Pain Program of the University of California at Los Angeles School of Medicine searched several databases for reports of randomized, controlled clinical trials of complementary and alternative medical modalities used to treat chronic facial pain. Three acupuncture trials, eight biofeedback trials, and three relaxation trials met the researchers’ inclusion criteria, suggesting that these modalities were comparable to conventional treatment such as an intraoral appliance.99
Increasingly, the multidisciplinary pain management team, incorporating a variety of nonpharmacologic treatment modalities, is being considered “the optimal method for delivery of comprehensive treatment to patients in pain.”100 The incorporation of “alternative” forms of pain management, including acupuncture, relaxation techniques, hypnosis, biofeedback, and guided imagery, is acknowledged by the Children’s Hospital of the Medical College of Wisconsin to complement pharmacologic management of children’s pain.101 The selection, balance, and application of these treatment components should be based on consideration of an individual’s coping styles. Such a treatment program could be developed to provide a more consistently effective analgesia than the individual components can provide separately. Relieving the pain of childbirth, for example, without diminishing or distorting the full consciousness of the experience for the mother, would be consistent with the goals of the contemporary physician of natural medicine.
1. Krupp M.A., Chatton M.J. Current medical diagnosis and treatment. Los Altos, CA: Lange Medical; 1984. 1-5
2. Kitzinger S. Pain in childbirth. J Med Ethics. 1978;4:119–121.
3. Walsh D.A., Radcliffe J.C. Pain beliefs and perceived physical disability of patients with chronic low back pain. Pain. 2002;97:23–31.
4. Haythronthwaite J.A., Lawrence J.W., Fauerbach J.A. Brief cognitive interventions for burn pain. Ann Behav Med. 2001;23:42–49.
5. Piira T., Taplin J.E., Goodenough B., et al. Cognitive-behavioural predictors of children’s tolerance of laboratory-induced pain: implications for clinical assessment and future direction. Behav Res Ther. 2002;40:571–584.
6. Kitaeff R. Cognitive strategies for control of painful stress. Unpublished manuscript, 1979.
7. Melzack R., Casey K.C. Sensory, motivational and central control of pain. In: Kenshalo D.R., ed. The skin senses: proceedings. Springfield, IL: Charles C Thomas; 1968:423–443.
8. Feurerstein M., Skjei E. Mastering Pain. New York: Bantam; 1979. 17-21
9. Melzack R., Wall P.D. Pain mechanisms: a new theory. Science. 1965;150:971–979.
10. Cheng R.S., Pomeranz B. Electroacupuncture analgesia could be mediated by at least two pain-relieving mechanisms: endorphin and non-endorphin systems. Life Sci. 1979;25:1957–1962.
11. Baldwin R. Special delivery: the complete guide to informed birth. Millbrae, CA: Les Femmes; 1979.
12. Laukaran V.H., van den Berg B.J. The relationship of maternal attitude of pregnancy outcomes and obstetric complications: a cohort study of unwanted pregnancy. Am J Obstet Gynecol. 1980;136:374–379.
13. Hyodo M., Gega O. Use of acupuncture anesthesia for normal delivery. Am J Chin Med. 1977;5:63–69.
14. Davidson P.O., McDougall C.E. The generality of pain tolerance. J Psychosom Res. 1969;13:83–89.
15. Eysenck S. Personality and pain assessment in childbirth of married and unmarried mothers. J Mental Sci. 1961;107:417–429.
16. Levine F., Tursky B., Nichols D. Tolerance for pain, extroversion and neuroticism: failure to replicate results. Percept Mot Skills. 1966;23:847–850.
17. Morgan A.H., Lezard F., Prytulak S., et al. Augmenters, reducers, and their reaction to cold-pressor pain in waking and suggested hypnotic analgesia. J Pers Soc Psychol. 1970;16:5–11.
18. Mumford J.M., Newton A.V., Ley P. Personality, pain perception and pain tolerance. Br J Psychol. 1973;64:105–107.
19. Sweeney D.R., Fine B.J. Pain reactivity and field dependence. Percept Mot Skills. 1965;21:757–758.
20. Andrew J. Coping style, stress-relevant learning and recovery from surgery. Diss Abstr. 1968;28:1182–1183.
21. Davidson P.O., Bobey M.J. Repressor-sensitizer differences on repeated exposure to pain. Percept Mot Skills. 1970;31:711–714.
22. Cohen F., Lazarus R. Active coping processes, coping dispositions, and recovery from surgery. Psychosom Med. 1973;35:375–389.
23. Chapman C.R. Lecture. University of Washington; October 1979.
24. Bowers K. The effects of UCS temporal uncertainty on heart rate and pain. Psychophysiol. 1971;8:382–389.
25. Bandler R.J., Jr., Madaras G.R., Bem D.J. Self-observation as a source of pain perception. J Pers Soc Psychol. 1968;9:205–209.
26. Geer J.H., Davison G.C., Gatchel R.I. Reduction of stress in humans through non-veridical perceived control of aversive stimulation. J Pers Soc Psychol. 1970;16:731–738.
27. Pervin L. The need to predict and control under conditions of threat. J Pers Soc Psychol. 1963;31:570–585.
28. Staub E., Tursky B., Schwartz G.E. Self-control and predictability: their effects on reactions to aversive stimulation. J Pers Soc Psychol. 1971;18:157–162.
29. Johnson J.E. Effects of accurate expectations about sensations on the sensory and distress components of pain. J Pers Soc Psychol. 1973;27:261–275.
30. Neufeld R.W., Davidson P.O. The effects of vicarious and cognitive rehearsal on pain tolerance. J Psychosom Res. 1971;15:329–335.
31. Staub E., Kellett D.S. Increasing pain tolerance by information about aversive stimuli. J Pers Soc Psychol. 1972;21:198–203.
32. Seligman M., Maier S., Solomon R. Unpredictable and uncontrollable aversive events. In: Brush F., ed. Aversive Conditioning and Learning. New York: Academic Press, 1969.
33. Kanfer F.H., Seidner M.L. Self-control: factors enhancing tolerance of noxious stimulation. J Pers Soc Psychol. 1973;25:381–389.
34. Langer E, Janis I, Wolfer J. Effects of cognitive device and preparatory information on psychological stress in surgical patients. Unpublished manuscript, 1973.
35. Newton-John T.R., Spence S.H., Schotte D. Cognitive-behavioural therapy versus EMG biofeedback in the treatment of chronic low back pain. Behav Res Ther. 1995;33:691–697.
36. Vlaeyen J.W., Haazen I.W., Schuerman J.A., et al. Behavioural rehabilitation of chronic low back pain: comparison of an operant treatment, an operant-cognitive treatment and an operant-respondent treatment. Br J Clin Psychol. 1995;34:95–118.
37. Turner J.A., Jensen M.P. Efficacy of cognitive therapy for chronic low back pain. Pain. 1993;52:169–177.
38. van Dulmen A.M., Fennis J.F., Bleijenberg G. Cognitive-behavioral group therapy for irritable bowel syndrome: effects and long-term follow-up. Psychosom Med. 1996;58:508–514.
39. Dworkin S.F. Behavioral and educational modalities. Oral Surg Oral Med Pathol Oral Radiol Endod. 1997;83:128–133.
40. Gardea M.A., Gatchel R.J., Mishra K.D. Long-term efficacy of biobehavioral treatment of temporomandibular disorders. J Behav Med. 2001;24:341–359.
41. Arathuzik D. Effects of cognitive-behavioral strategies on pain in cancer patients. Cancer Nurs. 1994;17:207–214.
42. Osterhaus S.O., Passchier J., van der Helm-Hylkema H., et al. Effects of behavioral psychophysiological treatment on school children with migraine in a nonclinical setting: predictors and process variables. J Pediatr Psychol. 1993;18:697–715.
43. Basler H.D. Group treatment for pain and discomfort. Patient Educ Couns. 1993;20:167–175.
44. Sinclair V.G., Wallston K.A. Predictors of improvement in a cognitive-behavioral intervention for women with rheumatoid arthritis. Ann Behav Med. 2001;23:291–297.
45. Astin J.A., Beckner W., Soekin K., et al. Psychological interventions for rheumatoid arthritis: a meta-analysis of randomized controlled trials. Arthritis Rheum. 2002;47:291–302.
46. Williams D.A., Cary M.A., Groner K.H., et al. Improving physical functional status in patients with fibromyalgia: a brief cognitive behavioral intervention. J Rheumatol. 2002;29:1280–1286.
47. Lee B.H., Scharff L., Sethna N.F., et al. Physical therapy and cognitive-behavioral treatment for complex regional pain syndromes. J Pediatr. 2002;141:135–140.
48. Stevens R.J., Heide F. Analgesic characteristics of prepared childbirth techniques: attention focusing and systematic relaxation. J Psychosom Res. 1977;21:429–438.
49. Dahlquist L.M., Busby S.M., Slifer K.J., et al. Distraction for children of different ages who undergo repeated needle sticks. J Pediatr Oncol Nurs. 2002;19:22–34.
50. Haythronthwaite J.A., Lawrence J.W., Fauerbach J.A. Brief cognitive interventions for burn pain. Ann Behav Med. 2001;23:42–49.
51. Kanfer F.H., Goldfoot D.A. Self-control and tolerance of noxious stimulation. Psychol Rep. 1966;18:79–85.
52. Evans M.B., Paul G.L. Effects of hypnotically suggested analgesia on physiological and subjective responses to cold stress. J Consult Clin Psychol. 1970;35:362–371.
53. Anand B.K., Chhina E.S., Singh B. Some aspects of electroencephalographic studies in yogis. EEG Clin Neurophysiol. 1961;13:452–456.
54. Pelletier K., Peper E. The chutzpah factor in altered states of consciousness. J Humanis Psych. 1977;17:63–73.
55. Benson H. The Relaxation Response. New York: Avon; 1976.
56. Chaves J.F. Recent advances in the application of hypnosis to pain management. Am J Clin Hypn. 1994;37:117–129.
57. Kroger W.S. Clinical and experimental hypnosis in medicine, dentistry, and psychology. Philadelphia: Lippincott; 1963. 197-198
58. De Pascalis V., Magurano M.R., Bellusci A., et al. Somatosensory event-related potential and autonomic activity to varying pain reduction cognitive strategies in hypnosis. Clin Neurophysiol. 2001;112:1475–1485.
59. Yuan C.S., Attele A.S., Dey L., et al. Transcutaneous electrical acupoint stimulation potentiates analgesic effect of morphine. J Clin Pharmacol. 2002;42:899–903.
60. Naeser M.A., Hahn K.A., Lieberman B.E., et al. Carpal tunnel syndrome pain treated with low-level laser and microamperes transcutaneous electric nerve stimulation: a controlled study. Arch Phys Med Rehabil. 2002;83:978–988.
61. Chesterton L.S., Barlas P., Foster N.E., et al. Sensory stimulation (TENS): effect of parameter manipulation on mechanical pain thresholds in healthy human subjects. Pain. 2002;99:253–262.
62. Bonica J.J. Fundamental considerations. Vol I, Principles and practice of obstetric analgesia and anesthesia. Philadelphia: FA Davis, 1967.
63. Bonica J.J. The nature of pain in parturition. Clin Obstet Gynecol. 1975;2:499–516.
64. Augustinsson L.E., Bohlin P., Bundsen P., et al. Pain relief during delivery by transcutaneous electrical nerve stimulation. Pain. 1977;4:59–65.
65. Andersson S.A., Block E., Holmgren E. Lagfrekvent transkutan electrisk stimulering for smartlindring vid forlassning. Larktidningen. 1976, Jun 23;73(26-27):2421–2423.
66. Stewart P. Transcutaneous nerve stimulation as a method of analgesia in labour. Anaesthesia. 1979;34:361–364.
67. Kubista E., Kucera H., Riss P. The effect of transcutaneous nerve stimulation on labor pain. Geburtshilfe Frauenheilkd. 1978;38:1079–1084.
68. Bundsen P., Carlsson C.A., Forssman L., et al. Pain relief during delivery by transcutaneous electrical nerve stimulation. Prakt Anaesth. 1978;13:20–28.
69. Neumark J., Pauser G., Scherzer W. Pain relief in childbirth; an analysis of the analgesic effects of transcutaneous nerve stimulation (TNS), pethidine and placebos. Prakt Anaesth. 1978;13:13–20.
70. Kemp T. The use of transcutaneous electrical nerve stimulation on acupuncture points in labour. Midwives. 1996;109:318–320.
71. Robson J.E. Transcutaneous nerve stimulation for pain relief in labour. Anaesthesia. 1979;34:357–360.
72. Lewith G.T., Machin D. On the evaluation of the clinical effects of acupuncture. Pain. 1983;16:111–127.
73. Reichmanis M., Becker R.O. Relief of experimentally-induced pain by stimulation at acupuncture loci: a review. Comp Med East West. 1977;5:281–288.
74. Stux G., Pomeranz B. Basics of Acupuncture. New York: Springer-Verlag; 1988.
75. Chapman C.R., Colpitts Y.M., Benedetti C., et al. Evoked potential assessment of acupunctural analgesia: attempted reversal with naloxone. Pain. 1980;9:183–197.
76. Kumar A., Tandon O.P., Bhattarcharya A., et al. Somatosensory evoked potential changes following electro-acupuncture therapy in chronic pain patients. Anaesthesia. 1995;50:411–414.
77. Xu X., Shibasaki H., Shindo K. Effects of acupuncture on somatosensory evoked potentials: a review. J Clin Neurophysiol. 1993;10:370–377.
78. Fink M., Wolkenstein E., Luennemann M., et al. Chronic epicondylitis: effects of real and sham acupuncture treatment: a randomized controlled patient- and examiner-blinded long-term trial. Forsch Komplementarmed Klass Naturheilkd. 2002;9:210–215.
79. Irnich D., Behrens N., Gleditsch J.M., et al. Immediate effects of dry needling and acupuncture at distant points in chronic neck pain: results of a randomized, double-blind, sham-controlled crossover trial. Pain. 2002;99:83–89.
80. Tsui P., Leung M.C. Comparison of the effectiveness between manual acupuncture and electro-acupuncture on patients with tennis elbow. Acupunct Electrother Res. 2002;27:107–117.
81. Targino R.A., Imamura M., Kaziyama H.H., et al. Pain treatment with acupuncture for patients with fibromyalgia. Curr Pain Headache Rep. 2002;6:379–383.
82. Sim C.K., Xu P.C., Pua H.L., et al. Effects of electroacupuncture on intraoperative and postoperative analgesic requirement. Acupunct Med. 2002;20:56–65.
83. Ramnero A., Hanson U., Kihlgren M. Acupuncture treatment during labour: a randomized, controlled trial. Br J Obstet Gynecol. 2002;109:637–644.
84. Haake M., Muller H.-H., Schade-Brittinger C., et al. German Acupuncture Trials (GERAC) for Chronic Low Back Pain. Arch Intern Med. 2007;167:1892–1898.
85. Wu G.C., Zhu J., Cao X. Involvement of opioid peptides of the preoptic area during electroacupuncture analgesia. Acupunct Electrother Res. 1995;20:1–6.
86. Zhu L., Li C., Ji C., et al. The role of OLS in peripheral acupuncture analgesia in arthritic rats. Zhen Ci Yan Jiu [Acupunct Res]. 1993;18:214–218.
87. Zhou L., Jiang J.W., Wu G.C., et al. Changes of endogenous opioid peptides content in RPGL during acupuncture analgesia. Sheng Li Xue Bao. 1993;45:36–43.
88. Carlsson C. Acupuncture mechanisms for clinically relevant long-term effects: reconsideration and a hypothesis. Acupunct Med. 2002;20:82–99.
89. Tsuei J.J., Lai Y., Sharma S.D. The influence of acupuncture stimulation during pregnancy. Obstet Gynecol. 50, 1977. 479
90. Motoyama H. How to measure and diagnose the functions of meridians and corresponding internal organs. Tokyo: Institute for Religious Psychology; 1976.
91. Nakatani Y. A guide for application of Ryodoraku autonomous nerve regulatory therapy. Tokyo: Japanese Society of Ryodoraku Autonomic Nervous System; 1972.
92. Hyodo M. New management of pain. Tokyo: Chiyugai Igakushiya; 1970.
93. Wu M.T., Sheen J.M., Chuang K.H., et al. Neuronal specificity of acupuncture response: a fMRI study with electroacupuncture. Neuroimage. 2002;16:1028–1037.
94. Furlan A.D., Brosseau L., Imamura M., et al. Massage for low back pain: a systematic review within the framework of the Cochrane Collaboration Back Review Group. Spine. 2002;27:1896–1910.
95. Earles J., Folen R.A., James L.C. Biofeedback using telemedicine: clinical applications and case illustrations. Behav Med. 2001;27:77–82.
96. Seltzer S., Dewart D., Pollack R.L., et al. The effect of dietary tryptophan on chronic maxillofacial pain and experimental pain tolerance. J Psychiatr Res. 1982-83;17:181–186.
97. Bensky D., Gamble A. Chinese herbal medicine materia medica. Seattle: Eastland Press; 1986. 389
98. Elkayam O., Ben Itzhak S., et al. Multidisciplinary approach to chronic back pain: prognostic elements of the outcome. Clin Exp Rheumatol. 1996;14:281–288.
99. Myers C.D., White B.A., Heft M.W. A review of complementary and alternative medicine use for treating chronic facial pain. J Am Dental Assoc. 2002;133:1189–1196.
100. Golden B.A. A multidisciplinary approach to nonpharmacologic pain management. J Am Osteopath Assoc. 2002;102:S1–S5.
101. Rusy L.M., Weisman S.J. Complementary therapies for acute pediatric pain management. Pediatr Clin North Am. 2000;47:589–599.


