21 Nonopioid intravenous anesthetics
Agonist: A drug that has a specific receptor affinity that produces a predictable response.
Antagonist: A drug that has the ability to block the effects of an agonist drug at the receptor site.
Anterograde Amnesia: The inability to recall events that occur after the onset of amnesia.
Antianalgesic: Administration of a drug that partially blocks the analgesic effects of other drugs that produce analgesia.
Antiemetic: A drug that prevents or alleviates nausea and vomiting.
Cardiostimulatory: Stimulation of the cardiovascular system.
Dissociative: Anesthesia that is characterized by analgesia and amnesia without loss of respiratory function.
Esterases: A chemical group that breaks down certain enzymes.
Extrapyramidal: Effects of the structures outside the cerebrospinal pyramidal tracts of the brain that are associated with movement of the body.
Gamma-Aminobutyric Acid (GABA): An amino acid that functions as an inhibitory neurotransmitter in the brain and spinal cord.
Hypertriglyceridemia: Type I hyperlipoproteinemia.
Neuroleptanalgesia: A state of profound tranquilization with little or no depressant effect on the cortical centers.
Parenterally: Treatment other than through the digestive system.
Resedation: Sedation that recurs after clinical signs indicate that the sedation has ceased.
Sedatives: Substances that have a calming effect.
Sympatholytic: Antiadrenergic effects.
Sympathomimetic: A pharmacologic agent that mimics the effects of stimulation of the sympathetic nervous system.
Thrombophlebitis: Inflammation of a vein accompanied by the formation of a clot.
Torsades de Pointes (TdP): Potentially fatal heart arrhythmia.
Vagotonic: Augmenting the parasympathetic activity by stimulating the vagus nerve.
Mechanism of action of the nonopioid intravenous anesthetics
The nonopioid drugs appear to interact with gamma-aminobutyric acid (GABA) in the brain. GABA is an inhibitory neurotransmitter, and activation of the GABA receptors by GABA on the postsynaptic membrane causes inhibition of the postsynaptic neuron. The barbiturates appear to bind to the GABA postsynaptic receptor, with the net result of hyperpolarization of the postsynaptic neuron and inhibition of neuronal activity and ultimately loss of consciousness. Conversely, etomidate (Amidate), which is a nonbarbiturate induction agent, probably antagonizes the muscarinic receptors in the central nervous system (CNS) and acts as an agonist to the opioid receptors.1 The resultant action of these drugs is a loss of wakefulness.
Sedatives, such as the benzodiazepines, bind to specific receptors in the limbic system. These benzodiazepine receptors use GABA as part of the neurotransmitter system. After the benzodiazepines have bound to the receptor, the action of GABA is enhanced, which leads to the hyperpolarized state and ultimately to inhibition of neuronal activity.2 The drug flumazenil is a specific benzodiazepine receptor antagonist. Consequently, after the administration of a benzodiazepine agonist, flumazenil can be administered. The pharmacologic actions on the benzodiazepine receptor are reversed, and neuronal activity resumes.
Barbiturates
Thiopental
Thiopental is a respiratory depressant.3 The chief effect is on the medullary and pontine respiratory centers. This depressant effect depends on the amount of thiopental administered, the rate at which it is injected, and the amount and type of premedication given to the patient. The response to carbon dioxide is depressed at all levels of anesthesia and is abolished at deep levels of thiopental anesthesia; therefore apnea can be an adverse outcome of high-dose thiopental.
Perianesthesia care
If the anesthesia time exceeds 1 hour or if the total dose of thiopental exceeds 1 g, patients may have a delayed awakening time because of the redistribution of thiopental. This phenomenon is particularly common in obese patients because the drug is highly fat soluble. At present, no antagonist exists for the barbiturates; therefore airway management and monitoring of cardiovascular status are important.
Methohexital
Methohexital is an ultra–short-acting barbiturate intravenous anesthetic agent. It is usually indicated for short procedures in which rapid complete recovery of the patient is needed. Like thiopental, methohexital is rarely administered, primarily because of the excellent drug actions of propofol (Diprivan). Methohexital is approximately threefold more potent as thiopental, and the recovery time from anesthesia is extremely rapid (4 to 7 minutes) because the drug is redistributed from the CNS to the muscle and fat tissues, and a significant portion of the drug is metabolized in the liver.1 Consequently, the clearance of methohexital is approximately fourfold faster than that of thiopental. Methohexital causes about the same degree of cardiovascular and respiratory depression as does thiopental. This drug can cause coughing and hiccups and, after injection, excitatory phenomena may appear, such as tremor and involuntary muscle movements.
Nonbarbiturates
Propofol
Propofol (Diprivan) is a rapid-acting nonbarbiturate induction agent. It is administered intravenously as a 1% solution and is the most popular intravenous anesthetic in use. The dose for induction is 2 to 2.5 mg/kg.4 The dose should be reduced in elderly patients and in patients with cardiac disease or hypovolemia. In addition, propofol in combination with midazolam acts synergistically. In fact, the dose of propofol can be reduced by 50% when it is administered in combination with midazolam. When propofol is used as the sole induction agent, it is usually administered over 15 seconds and produces unconsciousness within approximately 30 seconds. Emergence from this drug is more rapid than emergence from thiopental or methohexital, because propofol has a half-life of 2 to 9 minutes5; therefore the duration of anesthesia after a single induction dose is 3 to 8 minutes, depending on the dose of the propofol. A major advantage of this drug is its ability to allow the patient a rapid return to consciousness with minimal residual CNS effects. Moreover, the drug’s low incidence rate of nausea and vomiting is of particular importance to perianesthesia nursing care. In fact, propofol may possess antiemetic properties.
Propofol has a profound depressant effect on both the rate and depth of ventilation. In fact, after the induction dose is administered, apnea normally occurs. The incidence rate of apnea is greater after propofol than after thiopental and may approach 100%. Consequently, if propofol is administered in the PACU, the perianesthesia nurse should be prepared to support the patient’s ventilation and, if necessary, intubate the patient6 (see Chapter 30).
Clinically, this drug is useful for intravenous induction of anesthesia, especially for outpatient surgery.7 The drug is also an excellent choice for procedures that require a short period of unconsciousness, such as cardioversion and electroconvulsive therapy. In addition, propofol can be used for sedation during local standby procedures. This drug does not interfere with or alter the effects of succinylcholine because it has such a rapid plasma clearance. Propofol can be used during surgery in a continuous intravenous infusion, and the patients still emerge from anesthesia in a rapid fashion without any CNS depression. This drug can be used in the PACU as a continuous infusion, and the level of sedation can be adjusted by titration to effect.6 The typical infusion rates for sedation with propofol are between 25 and 100 mcg/kg/min.
Long-term or high-dose infusions can result in hypertriglyceridemia, which is usually associated with elevated levels of pancreatic enzymes and possibly with pancreatitis. After long infusions, plasma concentrations of propofol gradually increase unless the infusion rate is decreased over time. Current data seem to indicate that the recovery from propofol is less rapid after 12 hours of intravenous sedation. Propofol is contraindicated in patients who are sensitive to soybean oil, egg lecithin, or glycerol and is not recommended for PACU or intensive care unit (ICU) administration in children because of the possibility of emergence agitation.8
Perianesthesia care
Propofol is a major component used in modern clinical anesthesia practice. It offers many advantages and few disadvantages. More specifically, propofol has one major advantage over all the other intravenous induction agents: early awakening. It can be used in the PACU if indicated. The major concern for the perianesthesia care of the patient who has received this drug is the level of postoperative pain. The nursing assessment and appropriate interventions for pain are the most important aspects of care of the patient who has received this drug.6
Etomidate
Etomidate (Amidate), which is a derivative of imidazole, is a short-acting intravenous hypnotic that was synthesized in the 1960s by the laboratories of Janssen Pharmaceutica (Beerse, Belgium). It is not related chemically to the commonly used hypnotic agents. This drug is a mere hypnotic and does not possess any analgesic actions. Etomidate is safe for administration to patients because it has a high therapeutic index. Metabolism of this drug is accomplished by hydrolysis in the liver and by plasma esterases, with the final metabolite being pharmacologically inactive. The cardiovascular effects of etomidate are minimal; when the drug is injected in therapeutic doses, only a small blood pressure decrease and a slight heart rate increase may be observed. Etomidate causes a minimal reduction in the cardiac index and the peripheral resistance. This drug does not seem to produce arrhythmias, which is why etomidate is used in place of propofol as an induction agent for patients with cardiac dysfunction. Respiratory effects include a dose-related reduction in the tidal volume and respiratory frequency, which can lead to apnea.1 Laryngospasm, cough, and hiccups can occur during injection of this drug; however, the severity of these clinical phenomena can be reduced with an opiate premedication.
Research has shown that etomidate inhibits steroid synthesis and that patients who receive etomidate via continuous infusion have marked adrenocortical suppression for as long as 4 days.1 Even when etomidate is administered as a single dose, adrenal function is suppressed for 5 to 8 hours. Consequently, after the administration of etomidate, a decrease is seen in cortisol, 17-alpha-hydroxyprogesterone, aldosterone, and corticosterone levels. Therefore etomidate is administered only to selected patients and is no longer administered via continuous intravenous infusion.1,5
Sedatives
Benzodiazepines
The benzodiazepines, which are sedatives, have enhanced the anesthetic outcomes of the surgical patient. They depress the limbic system without causing cortical depression. More specifically, they interact with the inhibitory neurotransmitter GABA and thus result in reduced orientation (hypnotic effect), retrograde amnesia, anxiolysis, and relaxing of the skeletal muscle.1,2 Opiates and barbiturates enhance the hypnotic action of the benzodiazepines.
Midazolam
Midazolam has become a popular drug in anesthesia practice and in the perianesthesia care of surgical patients. Midazolam can be used for premedication, cardioversion, endoscopic procedures, and induction of anesthesia and as an intraoperative adjunct for inhalation anesthesia. It also is an excellent agent for sedation during regional anesthetic techniques. The principal action of midazolam is on the benzodiazepine receptors in the CNS, particularly on the limbic system, which results in a reduction in anxiety and profound anterograde amnesia. This drug also has excellent hypnotic, anticonvulsant, and muscle-relaxant properties.
The water-soluble midazolam may offer some advantages over diazepam. It causes depression of the CNS by inducing sedation, drowsiness, and finally sleep with increasing doses. Midazolam is three to four times as potent as diazepam, has a shorter duration of action, and has a lesser incidence rate of injection pain and postinjection phlebitis and thrombosis. More specifically, this drug has a rapid onset of action, a peak in action between 10 and 30 minutes, and a duration of action between 1 and 4 hours. Midazolam administered at a dose of 0.2 mg/kg produces a decrease in blood pressure, an increase in heart rate, and a reduction in systemic vascular resistance. Midazolam should be used with caution in patients with myocardial ischemia and in those with chronic obstructive pulmonary disease.9 Postoperative patients who have a substantial amount of hypovolemia should not receive midazolam. In addition, midazolam does not affect intracranial pressure.4,10 Consequently, this drug can be used safely in neurosurgical patients in addition to patients with intracranial pathophysiology.
This drug can be administered in the PACU11; therefore the postanesthesia nurse must monitor the patient for respiratory depression after injection because midazolam causes a dose-dependent respiratory depression. Given that every patient in the PACU has received a plethora of depressant drugs during surgery, midazolam can be potentiated easily when administered in the PACU. Because of this potentiation factor, any dose of midazolam administered in the PACU should be considered effective enough to cause profound respiratory depression. Therefore, oxygen and resuscitative equipment must be immediately available, and a person skilled in maintaining a patent airway and supporting ventilation should be present. Extra care also should be observed in patients with limited pulmonary reserve and in the elderly and debilitated with reduction of the dosage of midazolam by 25% to 30%.
Midazolam can be given via continuous infusion for patients who need sustained sedation.7 However, midazolam has a pH-dependent diazepine ring; at physiologic pH, the ring can close, causing CNS penetration. In addition, its metabolites are partially active, all of which make midazolam not the drug of choice for long-term sedation. Midazolam is sometimes used in the treatment of critically ill patients who are agitated. The guidelines for use can be found in Box 21-1.
Diazepam
The principal action of diazepam is the depression of limbic system function. Important actions of diazepam are the production of anterograde amnesia for as long as 48 hours after surgery, reduction of anxiety, and provision of minimal cardiovascular depressant effects.1 Clinical doses of diazepam cause a slight degree of respiratory depression; when it is combined with an opiate, the chance of respiratory depression, including apnea, is greatly increased.
Diazepam may possess some muscle-relaxant properties. Diazepam has been reported to be antagonistic to depolarizing neuromuscular blocking agents, such as succinylcholine, and the action of the nondepolarizing neuromuscular blocking agents (e.g., vecuronium) are reported to be potentiated. Diazepam has been used clinically for psychomotor and petit mal seizures because of its anticonvulsant actions.2,12
Because many patients who undergo cardioversion are debilitated, diazepam can be used as sedation for this procedure. Increments of 2.5 to 5 mg can be given at 30-second intervals until the speech of the patient is slurred or light sleep occurs. At the time of electric discharge, the patient may have brief muscle contraction and slight arousal. When this technique is used, a significant number of the patients have complete amnesia regarding the event. Diazepam can also be used to provide anesthesia in endoscopic and dental procedures and to control behavior on emergence from ketamine.7 Finally, this drug also has strong anticonvulsant activity and can stop generalized seizure activity.
Lorazepam
Lorazepam (Ativan), a long-acting benzodiazepine, is used as a premedication in current clinical anesthesia practice and as a long-acting slow-onset benzodiazepine for sedation in the PACU and ICU. This drug has actions similar to those of diazepam, but has a slow onset of action from 20 to 40 minutes; the pharmacologic activity can last as long as 24 hours.9 Lorazepam produces profound anterograde amnesia, tranquilization, and a reduction of anxiety, and the drug provides good cardiovascular and respiratory stability. Therapeutic plasma concentrations are achieved in approximately 3 hours when the drug is given orally. The drug is well absorbed via the intramuscular route; however, the patient has a significant amount of pain during the injection of the drug. Lorazepam can also be injected intravenously, and the patient may have some burning on injection. Because of its slow onset and long duration, lorazepam is mainly used as a preanesthetic medication. If this drug has been administered in the preoperative period, the effects of lorazepam may last well into the postoperative period because of its prolonged action. If an opioid is administered in the PACU to a patient who received lorazepam before surgery, the nurse should monitor for increased opioid sedation and respiratory depression because of the potentiation of the opioid by lorazepam.
Caution should be taken with use of lorazepam in the PACU for sedation. Lorazepam does not have any active metabolites. This long-acting but slow-onset benzodiazepine is often delivered via intermittent boluses, but also can be administered as a continuous infusion. Peak effects are not observed for 30 minutes. However, the solvent for lorazepam contains polyethylene glycol 400 and propylene glycol, both of which have been implicated in the development of lactic acidosis, acute tubular necrosis, and hyperosmolar coma when lorazepam is used in prolonged high-dose infusions.12 The toxic threshold for this effect has not been defined; therefore high-dose infusions should be avoided, and monitoring for these side effects should be initiated.
Lorazepam is sometimes used in the treatment of critically ill patients who are agitated. The guidelines for use can be found in Box 21-2.
Benzodiazepine antagonists
Flumazenil
Flumazenil (Romazicon), a benzodiazepine antagonist, antagonizes or reverses the effects of benzodiazepine-induced sedation at the benzodiazepine receptors. Consequently, it reverses the CNS effects of benzodiazepines, such as the sedation produced by diazepam and midazolam. This drug also reverses the other effects produced by benzodiazepine agonists, including anxiolytic, muscle-relaxant, ataxic, and anticonvulsant actions. However, flumazenil may not be effective in the treatment for benzodiazepine-induced hypoventilation or respiratory failure. This drug is specific for the benzodiazepines and, more specifically, their receptors. Consequently, this drug does not reverse the effects of barbiturates, opiates, and ethanol. Flumazenil should be used with great caution in patients who have a history of epilepsy or chronic benzodiazepine use, because reversal with flumazenil in these patients can result in seizures. The incidence rate of postoperative nausea and vomiting is increased after flumazenil has been administered.
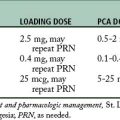
The usual reversal dose for flumazenil is 0.4 mg administered intravenously in 0.1-mg increments. Flumazenil should be administered slowly to avoid the adverse consequences of abrupt wakening. A maximum dose for this drug is 1 mg. The onset of action is usually within 5 minutes, with a duration of action between 1 and 2 hours. Flumazenil has a shorter duration of action than most of the benzodiazepines, and consequently the risk of resedation can occur after the initial reversal dose was administered. This risk is especially true when high doses of benzodiazepines were previously administered. Therefore, after the administration of flumazenil, the patient should be monitored for resedation and other residual effects of benzodiazepines in the PACU and on the receiving unit. If signs of resedation develop, flumazenil should be given at 20-minute intervals as needed to reverse the sedation. In this situation, no more than 1 mg should be given at any one time, and no more than 3 mg should be given within a 1-hour period.5 This drug should prove to be a valuable asset in the care of the patient who has received an excessive dose of a benzodiazepine, such as midazolam or diazepam. Consequently, flumazenil is useful during surgery, after surgery, and in the ICU.6
Physostigmine
Physostigmine (Antilirium) is an anticholinesterase that crosses the blood-brain barrier. Its action is inhibition of the enzyme acetylcholinesterase, which results in an increase in the availability of acetylcholine at the receptors that are affected by the benzodiazepines in the CNS. The preponderance of acetylcholine counteracts the negative effects of glycine and GABA. Consequently, this drug provides a nonspecific reversal of the CNS side effects of the benzodiazepines, scopolamine, and ketamine. The dosage is 0.5 to 1 mg, and it should be administered slowly to prevent untoward cholinergic side effects.1 Because this drug is a nonspecific agent, a number of vagally mediated cholinergic side effects can occur after its administration. These effects include nausea, vomiting, salivation, bradycardia, bronchospasm, and seizures. Because of its nonspecific properties, physostigmine is rarely used for the reversal of the untoward effects of the benzodiazepines.
Butyrophenones
Haloperidol
Haloperidol (Haldol) is a butyrophenone tranquilizer that has limited use in anesthesia practice because of its long duration of action and its high incidence rate of extrapyramidal reactions4; however, it has been found to be an excellent antiemetic. The drug is not approved for intravenous use and is usually administered intramuscularly at a dose of 2 to 5 mg. It is used in the treatment of psychoses and as an antiemetic. Haloperidol is sometimes used in the treatment of critically ill patients who are agitated. The guidelines for use can be found in Box 21-3.
Droperidol
Droperidol (Inapsine) can be used alone or in combination with fentanyl (Sublimaze) as part of a neuroleptanalgesic technique. Droperidol is rarely used during surgery for the purposes of being a component of anesthesia, but it is administered in small doses for its antiemetic effect after surgery. It produces a state of calm, disinclination to move, and disconnection from surroundings. The drug has an alpha-adrenergic blocking effect, which offers some protection against the vasoconstrictive components of shock; it leads to good peripheral perfusion; and it unmasks hypovolemia. More specifically, when a patient has compensation for a borderline hypovolemic state with activation of the alpha-vasoconstriction mechanisms, vital signs are normal. When a drug such as droperidol is administered to this patient, by virtue of droperidol’s alpha-blocking properties, the signs of hypovolemia appear; therefore the patient’s hypovolemia is “unmasked.” Droperidol also protects against epinephrine-induced arrhythmias and has an antiemetic effect. In fact, because of its excellent antiemetic properties, droperidol is sometimes administered toward the end of the surgical procedure or in the PACU to reduce the risk of vomiting and aspiration in anxious patients. The antiemetic dose of droperidol is between 1 and 2.5 mg and can be given intravenously. Because of its alpha-blocking properties, this drug can be administered in the PACU on a short-term basis to reduce the afterload.
Droperidol is similar to chlorpromazine (Thorazine) in its CNS effects; however, its mechanism of action is different. Droperidol is more selective than chlorpromazine because it provides more tranquility with less sedation and has less effect on the autonomic nervous system. Droperidol has been classified as a neuroleptic and has some adverse effects that should be assessed throughout the PACU phase. Droperidol may cause hypotension because of its alpha-adrenergic blocking effect and peripheral vasodilatation. It may cause extrapyramidal excitation, such as twitchiness, oculogyric seizures, stiff neck muscles, trembling hands, restlessness, and occasionally, psychologic disturbances (e.g., hallucinations). These excitation can be reversed with atropine or antiparkinsonian drugs such as benztropine mesylate (Cogentin) and trihexyphenidyl hydrochloride (Artane).2 Clinically, patients who have received droperidol have reported the dichotomy of appearing outwardly calm while feeling terrified inside and unable to express how they feel. As a result, the perianesthesia nurse should provide emotional support to all patients who have received droperidol.
Perianesthesia care
In the immediate postoperative period, the awakening from neuroleptanesthesia is usually rapid, extremely smooth, and uneventful. A striking feature is the extension of analgesia well into the postoperative period. It is difficult to explain the mechanism of such a prolonged pain-relieving effect with a drug such as fentanyl, in which the onset is so rapid and the duration of action is so short.
The patient should be encouraged to cough and perform the sustained maximal inspiration (SMI) maneuver in the PACU (see Chapters 12 and 28). Patients who have received even low-dose droperidol can drift back to sleep unless they are encouraged to move about the surroundings. The perianesthesia nurse will find that, because the analgesia extends into the postoperative period, the patient who has received droperidol is more willing to cough and perform the SMI maneuver. The perianesthesia nurse should use verbal stimulation with these patients because, if ordered, the patient will be able to take a deep breath; otherwise, respiration may remain slow and shallow, or the patient may even become apneic. Consequently the perianesthesia nurse must remain with the patient, provide verbal stimulation, and actively monitor for any signs of respiratory depression.
Nonsteroidal antinflammatory drugs
Ketorolac
Ketorolac (Toradol) is an analgesic that is classified as a nonsteroidal antiinflammatory drug (NSAID). Its mode of action is inhibition of the prostaglandin synthetase enzyme; therefore ketorolac has analgesic, antiinflammatory, and antipyretic actions. An intramuscular dose of 30 mg of this drug is equal to approximately 12 mg of morphine or 100 mg of meperidine in degree of postoperative pain relief. This drug can be administered via either the intravenous or intramuscular route (see Table 19-1). When it is used with supplemental opioids, ketorolac is an excellent postoperative analgesia. For acute postoperative pain, an initial loading dose of 30 mg can be administered intramuscularly. Ketorolac can be administered every 6 hours thereafter at a dose of 15 mg. The duration of analgesia, but not the peak analgesic effect, is increased when the dose is increased beyond its recommended dose range of 15 to 60 mg. Ketorolac should be given at a lower dose range for patients with renal disease, for the elderly (older than 70 years) and for patients who weigh less than 50 kg. Because this drug is an NSAID and not an opioid, its lack of effect on psychomotor activities and on the respiratory system makes it an ideal analgesic for outpatient surgery.
Indomethacin
This drug has been shown to reduce postoperative pain in the PACU and in particular, patients recovering from a cholecystectomy when used as a rectal suppository.13 It is hoped that more research will be conducted in the PACU to determine the effectiveness of pain reduction using NSAIDs such as indomethacin.
Nonopioid medications
OFIRMEV (acetaminophen) is the first intravenous formulation of acetaminophen in the United States. It is indicated for the management of mild to moderate pain, management of moderate to severe pain with adjunctive opioid analgesics, and reduction of fever. It is for use with patients who are adults or children age 2 years or older. This new drug has become an important component of a multimodal approach to postoperative pain management.14
OFIRMEV is administered over a 15-minute period. The onset of analgesia occurs within 5 to 10 minutes of intravenous administration, with the peak analgesic effect within 1-hour a duration of 4 to 6 hours. It should be used with caution in patients who have hepatic impairment; however, it has not been shown to affect platelet function or increase surgical bleeding, which means it can be used during the perioperative period. Acetaminophen can potentiate the anticoagulant effects of warfarin; it does not cause the gastric irritation that has been attributed to NSAIDs.14 Intravenous acetaminophen may decrease the consumption of opioids by postoperative patients. OFIRMEV will become part of a multimodal approach to pain management that will affect patient comfort and satisfaction and lead to increased patient safety with fewer required opioid rescues.14
Other sedative medications
Dexmedetomidine
In the PACU, if dexmedetomidine is administered via intravenous infusion, the nurse should monitor the patient for significant episodes of bradycardia and hypotension. If intervention is necessary, decreasing or stopping the dexmedetomidine infusion and increasing the rate of intravenous fluid administration along with elevation of the lower extremities may be all that is needed; if the hypotension continues, vasopressor agents may be necessary (see Chapter 11). If the bradycardia continues, the PACU nurse may need to intervene by obtaining a physician order for an anticholinergic such as atropine or glycopyrrolate. A dexmedetomidine infusion is not recommended to last more than 24 hours. Because dexmedetomidine resembles the alpha-2 adrenergic agent clonidine, abrupt withdrawal of the drug can result in symptoms associated with abrupt stoppage of clonidine. Consequently, when dexmedetomidine is discontinued, symptoms that include nervousness, agitation, headaches, and a rapid rise in blood pressure should be monitored and reported to the anesthesia provider immediately.
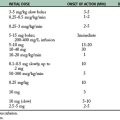
Dexmedetomidine is usually administered with a controlled infusion device. The drug should be titrated to the desired clinical effect, which is usually less than 3 on the Ramsey Sedation Scale (Table 21-1). Generally, a loading infusion of 1 mcg/kg over 10 minutes followed by a maintenance infusion of 0.2 to 0.6 mcg/kg/h, and the rate of the maintenance infusion can be adjusted to achieve the desired level of sedation.
| CLINICAL SCORE | LEVEL OF SEDATION ACHIEVED |
|---|---|
| 6 | Asleep, no response |
| 5 | Asleep, sluggish response to light glabellar tap or loud auditory stimulus |
| 4 | Asleep, but with brisk response to light glabellar tap or loud auditory stimulus |
| 3 | Patient responds to commands |
| 2 | Patient cooperative, oriented, and tranquil |
| 1 | Patient anxious, agitated, or restless |
Dissociative anesthetics
Ketamine
Traditionally, general anesthetic agents achieved control of pain with depression of the CNS. Ketamine is an anesthetic agent that has been introduced has a totally different mode of action. It selectively blocks pain conduction and perception, leaving those parts of the CNS that do not participate in pain transmission and perception free from the depressant effects of the drug. Ketamine is a dissociative drug because patients whose conditions are totally analgesic usually do not appear to be asleep or anesthetized, but rather disassociated from the surroundings. The drug is nonbarbiturate and nonopioid. It is administered parenterally and has a short duration. Early laboratory studies with ketamine suggested that most of the drug’s activity is centered in the frontal lobe of the cerebral cortex.
The clinical characteristics of ketamine consist of a state of profound analgesia combined with a state of unconsciousness. The patient usually has marked horizontal and vertical nystagmus. The eyes are usually open and shortly become centered and appear in a fixed gaze. The pupils are moderately dilated and react to light. Respiratory function is usually unimpaired, except after rapid intravenous injection, when it may become depressed for a short time. Ketamine is sympathomimetic in action and is beneficial to patients with asthma because of its bronchodilating effect. When patients receive ketamine, the pharyngeal and laryngeal reflexes remain intact. The tongue usually does not become relaxed, and the airway usually remains unobstructed. Ketamine accelerates the heart rate moderately and increases both the systolic and the diastolic pressure for several minutes, after which the pulse and blood pressure return to preinjection levels. Finally, ketamine increases cerebral blood flow and, consequently, intracranial pressure. Therefore this drug definitely is contraindicated in patients who are at risk for increased intracranial pressure.15
Perianesthesia care
The widespread use of ketamine requires an entirely different approach to perianesthesia nursing care. It should also be noted that ketamine coupled with a small dose of a benzodiazepine may be continued in a low-dose intravenous for sedation and pain relief in the PACU. Certainly, the agent has some deficiencies, but commonly overlooked is the fact that it is one of the safest anesthetics. Its safety justifies its important place in the drugs used by the anesthesiologist. Ketamine appears to be an excellent anesthetic for pediatric patients, as the sole agent for short procedures, for induction of anesthesia in patients at extremely poor risk, and for patients with burns that necessitate surgical treatment. Certain adult orthopedic and diagnostic procedures have also been found suitable for the use of ketamine anesthesia. Ketamine continues to be popular for certain types of anesthetic procedures. Because ketamine is a dissociative agent, its actions should be well understood by the PACU staff to ensure effective informed care of the patient.
Summary
The nonopioid agents are gaining popularity because they are becoming more opioid-like without the side effects. In addition, the induction agents have changed from thiopental to propofol in a short time. The same can be said for the benzodiazepines in the perioperative patient; midazolam is preferred to diazepam. In both cases, the newer drugs offer distinct advantages during surgery and, more importantly, after surgery in the PACU. Finally, the drug ketamine has continued over the years to serve as an excellent anesthetic for specific situations. In addition, the PACU stay for the patient who has received ketamine has improved significantly because of the many adjunct drugs that can be used to prevent the psychic aberrations associated with that drug in the PACU. If fact, because ketamine has demonstrated many positive effects on the relief of postanesthesia pain, it is an agent that can be used in a low-dose intravenous infusion in the PACU with minimal side effects. In an effort to reduce the length of stay of the patient and to provide appropriate post anesthesia pain relief, the nonopioid pharmacologic agents are becoming an important component of intraoperative and postanesthesia care.
1. Brunton L, et al. Goodman and Gilman’s the pharmacological basis of therapeutics, ed 12. New York: McGraw-Hill Professional; 2010.
2. Stoelting R. Pharmacology and physiology in anesthetic practice, ed 4. Philadelphia: Lippincott Williams & Wilkins; 2005.
3. Aitkenhead A, et al. Textbook of anesthesia, ed 5. Philadelphia: Churchill Livingstone; 2007.
4. Miller R, Pardo M. Basics of anesthesia, ed 6. Philadelphia: Saunders; 2011.
5. Nagelhout J, Plaus K. Nurse anesthesia, ed 4. St. Louis: Saunders; 2010.
6. Schick L, Windle PE. Perianesthesia nursing core curriculum: preprocedure, phase I and phase II PACU nursing. ed 2. Philadelphia: Saunders; 2010.
7. Blouin R, Gross J. Ventilation and conscious sedation. Semin Anesth. 1996;15(4):335–342.
8. Key K, et al. Use of propofol and emergence agitation in children: a literature review. AANA J.2010;78(6):468–473.
9. Barash P, et al. Clinical anesthesia, ed 6. Philadelphia: Lippincott Williams & Wilkins; 2009.
10. Fisher L. Anesthesia and uncommon diseases, ed 5. Philadelphia: Saunders; 2007.
11. Shorten G, et al. Postoperative pain management: an evidence-based guide to practice. Philadelphia: Saunders; 2006.
12. Borchardt M. Review of the clinical pharmacology and use of the benzodiazepines. J Perianesth Nurs. 1999;14(2):65–72.
13. Babar M, et al. Effect of preoperative rectal indomethacin on postoperative pain reduction after open cholecystectomy,. J Perianesth Nurs. 2010;25(1):7–10.
14. Groudine S, Fossum S. Use of intravenous acetaminophen in the treatment of postoperative pain. J Perianesth Nurs. 2011;26(2):74–80.
15. Rakic A, Golembiewski J. Low-dose ketamine infusion for postoperative pain management. J Perianesth Nurs. 2009;24(4):254–257.
American Association of Critical-Care Nurses. Core curriculum for progressive care nursing. Philadelphia: Saunders; 2010.
Aitkenhead A, et al. Textbook of anesthesia, ed 5. Philadelphia: Churchill Livingstone; 2007.
Alspach J. Core curriculum for critical care nursing, ed 6. Philadelphia: Saunders; 2005.
Atlee J. Complications in anesthesia, ed 2. Philadelphia: Saunders; 2007.
Barash P, et al. Clinical anesthesia, ed 6. Philadelphia: Lippincott Williams & Wilkins; 2009.
Barrett K, et al. Ganong’s review of medical physiology, ed 23. New York: McGraw-Hill Medical; 2009.
Bready L, et al. Decision making in anesthesiology, ed 4. St. Louis: Mosby; 2007.
Brunton L, et al. Goodman and Gilman’s the pharmacological basis of therapeutics, ed 12. New York: McGraw-Hill Professional; 2010.
Conlay L, et al. Case files anesthesiology. New York: McGraw-Hill Medical; 2011.
Davis P, et al. Smith’s anesthesia for infants and children. St. Louis: Mosby; 2011.
Drake R, et al. Gray’s anatomy for students, ed 2. Philadelphia: Churchill Livingstone; 2009.
Deutschman C, Netigan P. Evidence-based practice of critical care. Philadelphia: Saunders; 2010.
Fisher L. Anesthesia and uncommon diseases, ed 5. Philadelphia: Saunders; 2007.
Gallager C, Issenberg B. Simulation in anesthesia. Philadelphia: Saunders; 2007.
Hall J. Guyton and Hall textbook of medical physiology, ed 12. Philadelphia: Saunders; 2011.
Hines R, Marschall K. Handbook for Stoelting’s anesthesia and co-existing disease, ed 3. Philadelphia: Saunders; 2009.
Hines R, Marschall K. Stoelting’s anesthesia and co-existing disease, ed 6. Philadelphia: Saunders; 2012.
Kaplan J, et al. Cardiac anesthesia. New York: Churchill Livingstone; 2011.
Kier L, Dowd C. The chemistry of drugs for nurse anesthetists. Chicago: AANA Publishing; 2004.
Kulli J, Koch C. Does anesthesia cause loss of consciousness. Trends Neurosci. 1991;14(1):6–10.
Longnecker D, et al. Anesthesiology. New York: McGraw-Hill Medical; 2007.
Miller R, et al. Miller’s anesthesia, ed 7. Philadelphia: Churchill Livingstone; 2009.
Miller R, Pardo M. Basics of anesthesia, ed 6. Philadelphia: Saunders; 2011.
Mason R. Murray and Nadel’s textbook of respiratory medicine, ed 5. Philadelphia: Saunders; 2011.
Nagelhout J, Plaus K. Nurse anesthesia, ed 4. St. Louis: Saunders; 2010.
Pasero C, McCaffery M. Pain assessment and pharsmacologic management. St. Louis: Mosby; 2011.
Pasero C, McCaffery M. Orthopaedic postoperative pain management. J Perianesth Nurs. 2007;22(3):160–174.
Prielipp R, Young C. Current drugs for sedation of critically ill patients. Semin Anesthesia Perioperative Med Pain. 2001;20(2):85–94.
Reves J, et al. Midazolam: pharmacology and uses. Anesthesiology.1985;62:310–324.
Sandberg W, et al. The MGH textbook of anesthetic equipment. New York: Churchill Livingstone; 2011.
Schreiber J, et al. Prevention of succinylcholine-induced fasciculation and myalgia. Anesthesiology. 2005;103:877–884.
Sieber F. Geriatric anesthesia. New York: McGraw-Hill Medical; 2006.
Stoelting R. Pharmacology and physiology in anesthetic practice, ed 4. Philadelphia: Lippincott Williams & Wilkins; 2005.
Townsend CM, et al. Sabiston textbook of surgery: the biological basis of modern surgical practice. ed 19. Philadelphia: Saunders; 2012.
Vincent J, et al. Textbook of critical care, ed 6. Philadelphia: Saunders; 2011.
White P. Perioperative drug manual, ed 2. Philadelphia: Saunders; 2005.