Noninvasive Positive Pressure Ventilation
I Noninvasive Positive Pressure Ventilation
A Many have considered acute respiratory failure caused by the following as situations in which NPPV should be applied (Box 43-1).
1. Chronic obstructive pulmonary disease (COPD), acute exacerbation
2. Cardiogenic pulmonary edema
4. Neurologic/neuromuscular disease
5. Weaning from ventilatory support
1. Multiple randomized controlled trials of the use of NPPV in patients with COPD have indicated improved outcome.
2. Patients with a moderate to severe acute exacerbation of COPD and treated with NPPV
a. Are less likely to be intubated
b. Are less likely to develop nosocomial pneumonia
c. Have a shorter mechanical ventilation time
d. Have a shorter intensive care unit (ICU) stay
3. NPPV is a “standard of care” to manage an acute exacerbation of COPD.
4. NPPV for COPD should be the first-line therapy in all institutions caring for these patients.
1. NPPV has been useful for patients with cardiogenic pulmonary edema who are unable to effectively ventilate (Paco2, >45 cm H2O).
2. Patients with only hypoxemic acute respiratory failure should be treated with 8 to 12 cm H2O continuous positive airway pressure (CPAP).
3. Patients with a myocardial infarction or suspected myocardial infarction should not receive NPPV or CPAP; they should be intubated and invasively ventilated.
4. During NPPV 100% oxygen should initially be delivered when the indication is cardiogenic pulmonary edema.
1. Patients with severe asthma have a difficult time tolerating a tight-fitting mask.
2. These patients tend to be claustrophobic.
3. Case studies from a few centers have indicated success with NPPV for patients with asthma.
4. However, most do not recommend NPPV or CPAP for acute severe asthma.
5. Heliox does work well for many patients with acute severe asthma to reduce work of breathing (see Chapter 34).
E Neurologic/neuromuscular disease
1. NPPV works well for these patients when applied for short-term or long-term use for those with progressively deteriorating diseases.
2. No randomized controlled trials have been performed, but dozens of case series demonstrate improved gas exchange and avoidance of intubation.
3. NPPV should always be considered for patients with neurologic/neuromuscular disease before a decision to intubate is made.
F Weaning from ventilatory support
1. A series of randomized controlled trials have evaluated elective extubation to NPPV for patients who have failed to respond to weaning trials.
2. However, other randomized controlled trials have shown no benefit from elective extubation.
3. Extubation to NPPV should be considered for patients who have failed to respond to multiple attempts at weaning but all clinical signs indicate they should be weaned.
4. Patients who are extubated after passing a weaning trial but subsequently develop respiratory failure should also be considered for NPPV; however, existing data seem to indicate NPPV does not prevent reintubation.
1. Mask CPAP has been used over the years to manage acute hypoxemic respiratory failure from ALI.
2. A number of groups have used NPPV with varying success to manage hypoxemic respiratory failure.
3. However, the NPPV failure rate has been high in these patients (>60%), and mortality of those failing NPPV has also been high (>60%).
4. It is frequent that either CPAP or NPPV is maintained too long, delaying the decision to intubate.
5. As a result during intubation an increased risk of cardiac arrest exists.
6. NPPV or CPAP should be cautiously applied to patients with ALI, and if a beneficial response is not observed in a few hours, intubation should not be delayed.
1. These patients almost always develop nosocomial pneumonia if intubated and have a high mortality when intubated.
2. As a result NPPV should always be considered first-line therapy to manage ventilatory failure.
3. Randomized controlled trials indicate a decrease in intubation rate and mortality if NPPV is used.
I Patients awaiting lung transplantation
1. Many of these patients benefit from the short-term and long-term use of NPPV.
2. Intubation in transplantation candidates, similar to immunosuppressed patients, frequently results in the development of nosocomial pneumonia.
1. NPPV has been used to provide relief of hypercarbic and hypoxemic respiratory failure and to provide palliative care for these patients.
2. Because NPPV is life support patients should fully understand what it is they are receiving before it is started.
3. NPPV is useful for these patients to
4. The expected outcome of NPPV in this setting is different from that in any of the other settings in which NPPV is applied.
A Successful application of NPPV requires different skills than the successful application of invasive ventilation.
B The therapist must fully understand the indications, benefits, and limitations of NPPV.
C Patients must be part of the process. They must fully understand what is to be done and must be cooperative if the application is to be successful.
D The initial application period can be time consuming. Frequently 60 to 90 minutes of a therapist’s time is required during initial application.
E After appropriate patient instruction a mask is selected (see Section V, The Mask).
1. Initial application ideally is by the patient holding the mask to his or her face.
2. If the patient is incapable of holding the mask, the therapist should hold the mask.
3. Do not strap the mask to the patient’s face until he or she is completely accepting of the mask and all questions of the patient have been answered.
F Initial ventilator setting should be low (Box 43-2).
1. Positive end-expiratory pressure (PEEP): 0 to 4 cm H2O
2. Ventilatory pressure (pressure support, <5 cm H2O)
G Do not increase pressure setting until the patient is comfortable with the application of positive pressure.
H Remember the application of high pressure by mask is uncomfortable and needs to be applied gradually for maximum patient acceptance.
I Slowly adjust PEEP to improve inspiratory trigger capability (offset the effect of auto-PEEP). Normally maximum setting is 4 to 8 cm H2O.
J Increase pressure support level until an effective Vt is delivered (400 to 600 ml). In most cases 8 to 12 cm H2O pressure support is all that is necessary.
K Peak airway pressure should be kept <20 cm H2O if possible. This prevents gastric distention because the gastric opening pressure is approximately 20 to 25 cm H2O.
L Rate should be patient determined; set back up rate at 8 to 12/min, depending on patient ventilatory rate.
M Throughout this process constant encouragement and reinforcement of the purpose of NPPV should be provided.
N Only after the patient is fully accepting and comfortable with NPPV should the therapist leave the room.
O Ideally patients receiving NPPV for acute respiratory failure should be located in the emergency room, the ICU, or a special care unit where near-constant observation is possible.
A If within 2 hours of applying NPPV the following changes in patient’s status are observed, NPPV was successful.
B However, if none of the above occurs intubation should be considered because NPPV is not having a positive impact on the patient’s clinical status.
C Many patients present between these two extremes.
3. However, the patient’s clinical status appears improved.
4. The patient appears more comfortable and is not using accessory muscles to ventilate.
D In this setting NPPV has unloaded cardiopulmonary stress but has not yet altered gas exchange.
1. The patient should be allowed to continue on NPPV but should be closely observed for additional signs of benefit or failure.
2. Many patients may take a longer period before definitive blood gas data indicating success or failure are observed.
E Be careful not to prolong the unsuccessful application of NPPV to avoid marked difficulty in intubating the patients who fail to respond (i.e., cardiac arrest).
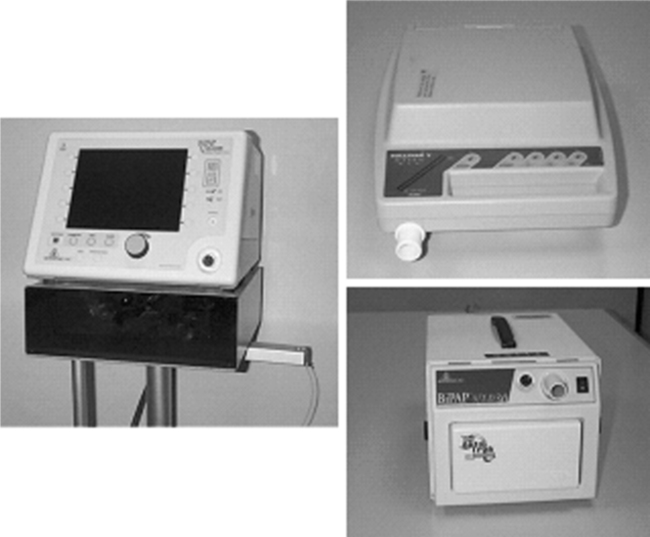
IV Type of Ventilator Used to Provide NPPV (Box 43-3)
A Any ventilator ever manufactured can be used to provide NPPV.
B However, most in the United States use either BiLevel pressure ventilators (Figure 43-1) or ICU ventilators.
C Most home care and subacute care ventilators available in the United States are not designed to provide NPPV. However, this situation is rapidly changing.
D BiLevel pressure ventilators deliver pressure-targeted breaths with at least the same efficiency as ICU ventilators.
E Many BiLevel pressure ventilators also
1. Automatically adjust trigger sensitivity to changes in system leak
2. Automatically adjust expiratory cycling criteria to changes in system leak
3. Better ensure patient ventilator synchrony than noninvasively applied ICU ventilators
F However, most BiLevel pressure ventilators
1. Can allow rebreathing of CO2 (Figure 43-2)
a. This is now avoided on newer models of BiLevel pressure ventilators by ensuring minimal PEEP is 4 cm H2O.
b. The inclusion of a secondary expiratory valve can avoid CO2 breathing.
c. Rebreathing occurs when the flow from the ventilator is low during expiration (no or little PEEP) and the patient exhales completely into the circuit (oronasal mask).
d. Because the ventilator has low internal resistance and only a small hole for exhalation (whisper swivel), exhaled gas can move into the single circuit gas delivery tubing all the way back to the ventilator.
e. As a result on the next breath the exhaled CO2 is rebreathed.
2. Do not incorporate patient monitoring or alarms
3. Do not allow visualization of airway pressure and flow waveforms, making it difficult to identify large leaks and patient-ventilator dysynchrony
G ICU ventilators can be used during NPPV; however, the disadvantages are
2. Inability on most to adjust expiratory cycling criteria during pressure support
a. As a result in some patients, pressure assist/control instead of pressure support is needed because pressure assist/control has a set inspiratory time (see Chapter 39).
b. Simply set the inspiratory time equal to the patient actual inspiratory time.
c. Gas delivery during pressure support and pressure assist/control is the same.
d. The only difference other than the ability to set a backup rate is the mechanism that terminates inspiration.
H The ideal ventilator for NPPV is a BiLevel pressure ventilator designed for ICU use that includes
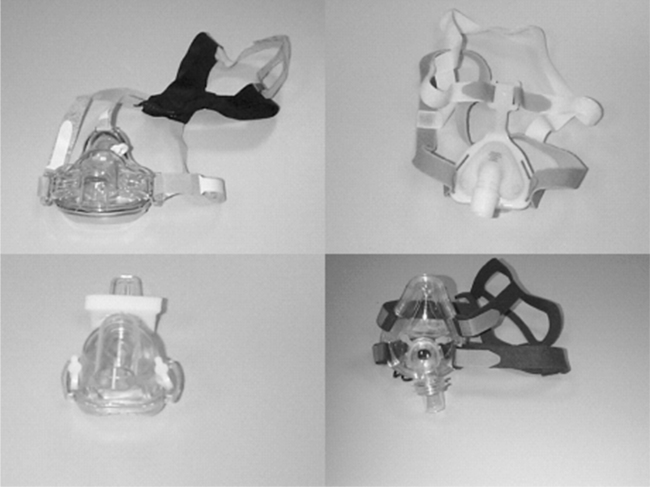
A A large number of nasal and oronasal masks are currently available from multiple manufacturers.
B Differences in opinion regarding the use of nasal or oronasal masks during acute respiratory failure exist. Table 43-1 lists the pros and cons of each mask type.
TABLE 43-1
| Nasal | Oronasal | |
| Ability to ventilate | Fair | Very good |
| Claustrophobia | Low | High |
| Ability to speak | Good | Poor |
| Ability to cough | Good | Limited |
| Air leak | Large | Small |
| Deadspace | Small | Large |
C We prefer the use of an oronasal mask for acute respiratory failure because it is easier to ensure better ventilation with the oronasal mask than a nasal mask: fewer leaks.
D Other facial interphases can be used, but the majority of patients can be effectively treated with an oronasal or nasal mask.
E However, 24 to 48 hours after initial application, when the acute failure is resolved, many patients prefer a nasal mask.
F Proper mask fit is a critical factor affecting successful application of NPPV.
G Regardless of mask type the top of the mask should rest about one fourth to one third of the way from top of the bridge of the nose.
1. If the mask rests higher on the nose there is a greater likelihood of leaks around the nose into the eyes.
2. The mask should conform to the lateral border of the nose.
H With nasal masks the bottom of the mask should rest above the upper lip.
I With oronasal masks they should either rest below the lower lip or at the chin, depending on mask design.
J If the mask is properly sized little force is necessary to maintain a good seal.
K When the mask is strapped to a patient’s face, two fingers should be able to be comfortably placed between the strap and the patient’s face.
L Too tight a strapped mask causes skin breakdown on the nose.
M It is always a good idea to bring a number of differently sized masks from a variety of manufacturers to ensure that the mask that best conforms to the patient’s anatomy can be used.
A With the acute application of NPPV to hospitalized patients, active humidification should be added to the system.
B Without active humidification dried retained pharyngeal secretions can be a major problem and a cause of NPPV failure and the need to intubate.
C Do not use heat and moisture exchangers (HMEs) during NPPV.
D HMEs increase resistance to gas flow.
E HMEs require all exhaled volume to enter the device, usually not possible because of leaks.
F HMEs have up to 100 ml of deadspace, causing CO2 rebreathing.
G HMEs are large and bulky and make it difficult for the mask to be secured.
H Active humidifiers do not need high circuit temperature to be effective. Maintaining circuit temperature at 28 to 30° C is sufficient in most cases.
A As stated earlier the ideal system is one in which the FIO2 can be precisely set and monitored.
B However, if a BiLevel ventilator without the ability to titrate FIO2 is used, O2 must be added to the circuit.
C With the standard NPPV circuit with the leak port near the mask, O2 should be titrated into the mask to ensure the highest FIO2.
D If a mask is used with the leak ports in the mask, O2 should be added to the circuit right after it leaves the BiLevel ventilator. This ensures the added O2 is not all lost via the mask leak ports.
E It should also be remembered that the higher the pressure settings on the ventilator, the greater the system flow and thus the lower the FIO2at a fixed flow rate.
F As a result when O2 is added to the circuit, careful monitoring of oxygenation status is critical.
VIII Aerosolized Pharmacologic Agents
A Medications can be aerosolized during NPPV.
B However, because of the leaks and high flow, some of the drug will be lost to the environment; as a result higher doses may be necessary.
C To maximize drug delivery, the nebulizer or metered dose inhaler should be placed between the leak port and the mask.
A Contrary to invasive ventilation NPPV can easily be stopped for short periods and the patient evaluated.
B Most patients can ingest clear liquids during their short periods without NPPV.
C If patients can tolerated long periods without NPPV, solid food can be ingested.
D Weaning is accomplished by increasing the amount of time patients are without NPPV.
E Many patients decide by refusing to continue when NPPV is ready to be discontinued.

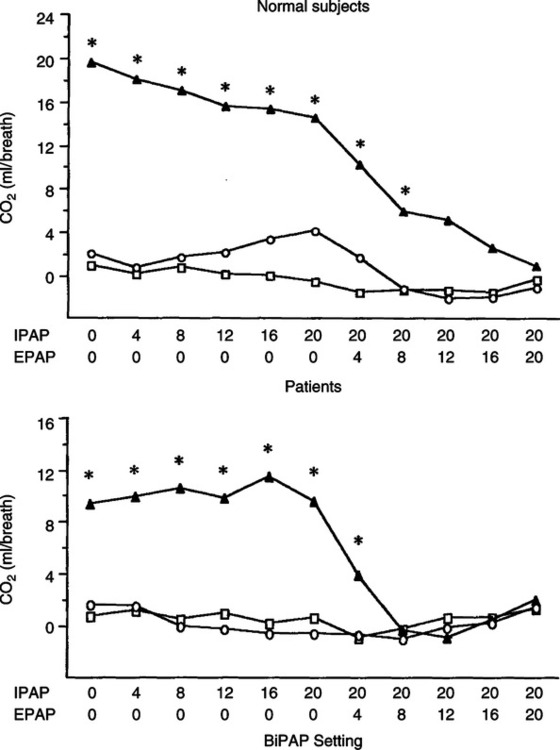
 , Whisper swivel exhalation port; O, plateau pressure valve;
, Whisper swivel exhalation port; O, plateau pressure valve;  , non-breathing valve. CO2 is rebreathed with the standard whisper swivel exhalation port unless approximately 4 cm H2O positive end-expiratory pressure is applied. *p < 0.05.
, non-breathing valve. CO2 is rebreathed with the standard whisper swivel exhalation port unless approximately 4 cm H2O positive end-expiratory pressure is applied. *p < 0.05.