51 Noninvasive Positive-Pressure Ventilation
Noninvasive ventilation is defined as the provision of ventilatory assistance to the lungs without an invasive artificial airway. Noninvasive ventilators consist of a variety of devices, including negative- and positive-pressure ventilators. Until the early 1960s, negative-pressure ventilation in the form of tank ventilators was the most common type of mechanical ventilation outside the anesthesia suite.1 However, during the Copenhagen polio epidemic of 1952, it was observed that the survival rate improved when patients with respiratory paralysis were treated with invasive positive-pressure anesthesia devices. After that, invasive positive-pressure mechanical ventilation gradually became the preferred means of treating acute respiratory failure.2 Negative-pressure and other so-called body ventilators were the mainstay of ventilatory support for patients with chronic respiratory failure until the mid-1980s.1
With improving mask and ventilator technology and the many advantages over negative-pressure ventilation,1 noninvasive positive-pressure ventilation (NIPPV) displaced negative-pressure ventilation as the treatment of choice for chronic respiratory failure in patients with neuromuscular and chest wall deformities.3 Over the past 15 years, noninvasive ventilation has moved from the outpatient to the inpatient setting, where it is used to treat acute respiratory failure. A 1997 survey of medical intensive care units (ICUs) in France, Switzerland, and Spain demonstrated that noninvasive ventilation was used in 16% of cases in which mechanical ventilation was required for respiratory failure, and a follow-up survey found that this rate was up to 23% in 2001.4 More recent surveys suggest that rates continue to increase over these levels.5 This chapter discusses the rationale for the increasing use of NIPPV in critical care, as well as appropriate indications, practical applications, and monitoring.
 Rationale
Rationale
The most important advantage of noninvasive ventilation is the avoidance of complications associated with invasive mechanical ventilation. These include complications related to direct upper-airway trauma, bypass of the upper-airway defense mechanisms, increased risk of nosocomial pneumonia, and interference with upper-airway functions, including the ability to eat and communicate normally.6 By averting airway intubation, noninvasive ventilation leaves the upper airway intact, preserves airway defenses, and allows patients to eat orally, vocalize normally, and expectorate secretions. Compared with invasive mechanical ventilation, noninvasive ventilation reduces infectious complications including pneumonia, sinusitis, and sepsis.7–9 Strengthening the rationale for its use is evidence accumulated over the past decade that noninvasive ventilation lowers morbidity and mortality rates of selected patients with acute respiratory failure and may shorten hospital length of stay or avoid hospitalization altogether,10 thus reducing costs.
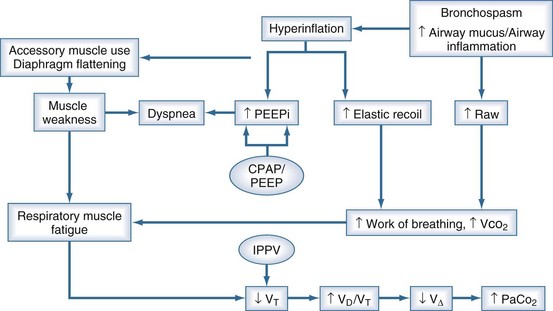
The main indication for mechanical ventilatory assistance is to treat respiratory failure, either type 1 (hypoxemic), type 2 (hypercapnic), or both. Figure 51-1 shows that airspace collapse, surfactant abnormalities, and airway narrowing and closure contribute to ventilation-perfusion abnormalities and shunt, which cause hypoxemia. By opening collapsed airspaces and narrowed airways, positive airway pressure reduces shunt and improves ventilation-perfusion relationships, ameliorating hypoxemia. In addition, positive airway pressure can reduce the work of breathing by improving lung compliance as a consequence of opening collapsed airspaces. Another potential benefit of positive airway pressure is enhanced cardiovascular function via the afterload-reducing effect of increased intrathoracic pressure. Conversely, deleterious cardiovascular effects may occur if the preload-reducing effect outweighs the afterload-reducing effect, as may be seen in patients with reduced intravascular fluid volume.
 Mechanisms of Action
Mechanisms of Action
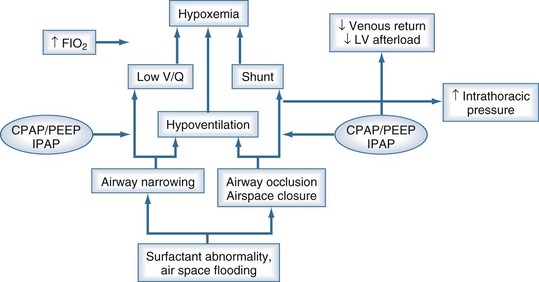
Figure 51-2 shows the pathophysiologic mechanisms that contribute to ventilatory failure. Increased airway resistance, reduced respiratory system compliance, and intrinsic positive end-expiratory pressure (PEEP) contribute to increased work of breathing, predisposing to respiratory muscle fatigue. In patients with chronic obstructive pulmonary disease (COPD), the increased radius of the diaphragmatic curvature, which increases muscle tension and thereby increases impedance to blood flow, exacerbates the situation. By counterbalancing intrinsic PEEP with extrinsic PEEP and by augmenting tidal volume with intermittent positive-pressure ventilation, NIPPV reduces the work of breathing and averts the vicious circle leading to respiratory failure. Work of breathing measurements, including transdiaphragmatic pressure, diaphragmatic pressure-time product, and diaphragmatic electromyographic amplitude, are all decreased when NIPPV is delivered to patients with exacerbations of COPD. In such patients, continuous positive airway pressure (CPAP) and pressure-support ventilation (PSV) both reduce the work of breathing, but the combination of the two (PSV + PEEP) is more effective than either alone.11
 Indications
Indications
A number of causes of acute respiratory failure are now considered appropriate for noninvasive ventilation therapy and are listed in Box 51-1. Evidence supporting these indications is rated and briefly discussed here; guidelines for patient selection are discussed later.
Box 51-1
Indications for Use of Noninvasive Ventilation in the Acute Care Setting
Airway Obstruction
Chronic Obstructive Pulmonary Disease
A number of randomized controlled trials12,13 and meta-analyses14 have consistently shown that compared with conventional therapy, NIPPV improves vital signs, gas exchange, and dyspnea scores; reduces the rates of intubation, morbidity, and mortality; and shortens hospital length of stay in patients with moderate to severe exacerbations of COPD. Thus NIPPV is considered the ventilatory mode of choice in selected patients with acute exacerbations of COPD. Some studies suggest that the addition of heliox to NIPPV further improves the work of breathing and gas exchange during COPD exacerbations,15 but a subsequent multicenter trial found no improvement in other outcomes compared with noninvasive ventilation alone.16
Asthma
Uncontrolled studies have reported improvements in gas exchange and low rates of intubation after the initiation of NIPPV in patients with severe asthma attacks. Two controlled trials have demonstrated a more rapid improvement in expiratory flow rates with NIPPV,17,18 and one showed a decreased hospitalization rate in acute asthma patients treated with noninvasive ventilation compared with a sham mask.18 Neither study was powered adequately to assess intubation or mortality rates. Nonetheless, these data support a trial of NIPPV in asthmatics responding poorly to initial bronchodilator therapy. Noninvasive ventilation can be combined with continuous nebulization and heliox, although the added value of these latter therapies has not been established in controlled trials.
Cystic Fibrosis
Uncontrolled studies indicate that noninvasive ventilation is useful to stabilize gas exchange in the treatment of acute episodes of respiratory failure in end-stage cystic fibrosis patients and can serve as a bridge to transplantation.19
Hypoxemic Respiratory Failure
Hypoxemic respiratory failure is defined as severe hypoxemia (arterial oxygen partial pressure-inspired oxygen fraction ratio <200) combined with a respiratory rate above 35 breaths per minute and a non-COPD diagnosis including acute pneumonia, acute lung injury (ALI), acute respiratory distress syndrome (ARDS), pulmonary edema, or trauma. Controlled trials of noninvasive ventilation to treat patients with acute hypoxemic respiratory failure have shown statistically significant reductions in the rate of intubation, length of hospital stay, incidence of infectious complications,8,20 and in one study, ICU mortality.20 However, because of the heterogeneity of causes, these studies fail to demonstrate that all patient subgroups with hypoxemic respiratory failure benefit equally from noninvasive ventilation. Further, when patients are stratified according to acuity of illness, patients with a simplified acute physiologic score (SAPS II) less than 35 fare considerably better with NIPPV than do those with higher scores.21 Thus the selection of patients with less severe disease is likely to enhance the success of NIPPV in treating hypoxemic respiratory failure, and studies that examine individual subgroups within the larger category are likely to be more useful clinically.
Pneumonia
One controlled trial showed that noninvasive ventilation in patients with severe community-acquired pneumonia lowers the rate of endotracheal intubation and shortens the length of ICU stay compared with conventional therapy; however, a subgroup analysis revealed that the benefits occurred only in patients with underlying COPD.22 No benefit was apparent in the non-COPD patients with severe pneumonia. A subsequent uncontrolled trial in non-COPD patients with severe pneumonia found that two-thirds of such patients treated with noninvasive ventilation eventually required intubation.23 Although the latter authors deemed a trial of noninvasive ventilation in non-COPD patients with severe pneumonia to be a reasonable approach, controlled data to support such a recommendation are currently lacking.
Immunocompromised States
The dismal prognosis of invasively ventilated immunocompromised patients makes noninvasive ventilation an appealing ventilatory mode, with its demonstrated ability to decrease the rate of nosocomial infection.7 In a study of 51 patients undergoing solid organ transplantation who developed acute hypoxemic respiratory failure within 3 weeks, noninvasive ventilation reduced the rate of intubation, frequency of invasive procedures, rate of nosocomial infection, duration of ICU stay, and ICU mortality (but not hospital mortality) compared with conventional therapy.24 In a subsequent randomized trial of neutropenic patients with pulmonary infiltrates and acute hypoxemic respiratory failure (most of whom had hematologic malignancies), noninvasive ventilation lowered the intubation rate, occurrence of nosocomial infections, and ICU and hospital mortality rates (the latter from 80% to 46%).25 More recently, noninvasive ventilation has been reported to yield similar benefits in acquired immunodeficiency syndrome (AIDS) patients with Pneumocystis carinii pneumonia versus invasive mechanical ventilation in physiologically and demographically matched patients.26 Thus, whenever possible, noninvasive ventilation should be tried first in immunocompromised patients with hypoxemic respiratory failure because of the potential to avoid the high morbidity and mortality rates associated with invasive mechanical ventilation in these patients.
Acute Respiratory Distress Syndrome
A small retrospective study reported that NIPPV averted intubation in 50% of patients during the early phase of acute lung injury or ARDS.27 However, for ARDS patients with severe oxygenation defects and multiple organ system dysfunction, invasive ventilation remains the preferred modality. A prospective cohort study28 using noninvasive ventilation as a “first-line” intervention for ARDS found that ventilator associated pneumonia and mortality were much reduced when patients succeeded rather than failed noninvasive ventilation, and a simplified acute physiology score of 34 or less and PAO2/FIO2 above 175 within the first hour predicted noninvasive ventilation success. Thus, noninvasive ventilation could be considered in ARDS patients meeting these criteria, but such patients must be monitored closely to avoid any delay in intubation if deterioration occurs.
Acute Cardiogenic Pulmonary Edema
Meta-analyses of randomized, controlled trials demonstrated that compared with oxygen therapy, CPAP (though not a true mode of ventilatory support) is highly effective at relieving respiratory distress, improving gas exchange, and averting intubation when used to treat patients with acute cardiogenic edema.29,30 Inspiratory assistance combined with expiratory pressure can reduce the work of breathing and alleviate respiratory distress more effectively than CPAP alone, and several uncontrolled trials and two controlled trials found that noninvasive ventilation and CPAP are equally effective in improving vital signs and avoiding intubation. The current recommendation is to use CPAP alone or noninvasive ventilation as initial therapy; if CPAP is used initially, inspiratory pressure support should be added if the patient has persistent hypercapnia or dyspnea.31
Postoperative Respiratory Failure
NIPPV and CPAP alone have been studied in postoperative patients who develop respiratory failure after various kinds of surgery. It reduces extravascular lung water and improves lung mechanics and gas exchange after coronary artery bypass surgery.32 Controlled trials show that CPAP averts postoperative complications compared to oxygen supplementation after high risk procedures like thoracoabdominal aortic procedures.33 Noninvasive ventilation improves oxygenation, reduces the need for re-intubation, lowers the mortality rate after lung resectional surgery,34 and enhances pulmonary function after gastroplasty.35 Thus noninvasive ventilation should be considered in selected postoperative patients at high risk of pulmonary complications or with frank respiratory failure, especially in the setting of underlying COPD or pulmonary edema.
Trauma and Burns
Trauma patients develop respiratory failure for a multitude of reasons, but some have chest wall injuries such as flail chest or mild acute lung injury that might respond favorably to NIPPV. In a retrospective survey of 46 trauma patients with respiratory insufficiency that had been treated with NIPPV, Beltrame and coworkers found rapid improvements in gas exchange and a 72% success rate; however, patients with burns responded poorly.36 More recently, a randomized trial of NIPPV versus high-flow oxygen in thoracic trauma patients with PAO2/FIO2 less than 200 was stopped early after enrollment of 50 patients because of significant reductions in intubation rate (12% versus 40%) and hospital length of stay (14 versus 21 days) in the NIPPV group.37 These promising results justify a cautious trial of NIPPV in carefully selected and monitored thoracic trauma patients, but data are too limited to draw firm conclusions.
Restrictive Lung Disease
The use of noninvasive ventilation in patients with underlying restrictive disease and acute deterioration of respiratory status has not been studied extensively because they constitute only a small portion of patients admitted to acute care hospitals. Patients with restriction related to an underlying neuromuscular disease and superimposed acute respiratory failure may benefit from a trial of NIPPV. Small case series have reported that using NIPPV in patients with myasthenic crises may avoid intubation.38 In contrast, patients with end-stage pulmonary fibrosis in respiratory extremis have been reported to do poorly with mechanical ventilation.39
Do-Not-Intubate Patients
Although controversial, noninvasive ventilation may be a useful tool in patients with acute respiratory failure who do not wish to be intubated. There are several reports of good outcomes (>50% survival to discharge) with noninvasive ventilation in this subset of patients, especially those with COPD and congestive heart failure.40 Noninvasive ventilation may also be used as a palliative technique to reduce dyspnea, preserve patient autonomy, and provide time for finalization of affairs for some terminal patients.41 However, there is concern that this may merely prolong the dying process, and patients and their families must be informed that noninvasive ventilation is being used as a form of life support in this setting and should be given the option to refuse it.
Facilitation of Weaning and Extubation
Patients who require invasive mechanical ventilation initially and fail to wean promptly are potential candidates for noninvasive ventilation to facilitate extubation, thus reducing the complications related to prolonged intubation. Several randomized controlled trials have demonstrated that noninvasive ventilation significantly shortens the duration of invasive mechanical ventilation, reduces the length of ICU stay, and improves survival compared with patients weaned in the routine fashion.42–44 Another potential application of noninvasive ventilation in the weaning process is to avoid reintubation in patients with extubation failure, a complication of invasive mechanical ventilation associated with a high mortality rate. Earlier studies looking at the role of NIPPV in this situation showed promise, but one randomized trial found that NIPPV may delay needed intubation in this setting, resulting in an increased ICU mortality rate.45 More recent studies have demonstrated that patients at high risk for extubation failure,46 especially those with hypercapnia,47 have reduced need for intubation and mortality if treated with noninvasive ventilation as opposed to oxygen supplementation alone. Thus, although the use of noninvasive ventilation to facilitate weaning and extubation appears to benefit hypercapnic patients with COPD or congestive heart failure, its overzealous application could lead to increased extubation failure rates and other adverse consequences.
Bronchoscopy
Both CPAP and NIPPV have been studied as ways of supporting oxygenation and ventilation during bronchoscopy. Using a specially designed open CPAP system during bronchoscopy in patients with marginal oxygenation, Maitre et al. observed maintenance of adequate gas exchange and avoidance of respiratory failure.48 In a controlled trial, Antonelli et al. demonstrated equivalent oxygenation and complication rates in patients undergoing bronchoscopy and supported with either noninvasive or invasive mechanical ventilation.47 Thus NIPPV is an effective way of providing ventilatory support in patients undergoing bronchoscopy.49
 Practical Application
Practical Application
Patient Selection
Noninvasive ventilation should be viewed as a “crutch” that assists patients through a period of acute respiratory failure while reversible factors are being treated, helping them avoid invasive mechanical ventilation and its attendant complications. To optimize the chance of success, noninvasive ventilation should be used early, when patients first develop signs of incipient respiratory failure. In addition, predictors of success are useful in identifying patients most likely to benefit (Box 51-2). The selection process might be viewed as taking advantage of a “window of opportunity”: the window opens when the patient first needs ventilatory assistance and closes when the patient becomes too unstable.
Ventilator Selection
PSV is a flow-triggered and flow-cycled mode, and patient effort determines tidal volume and duration of inspiration. Pressure-support modes have the potential to match breathing pattern quite closely, and they have been rated by patients as more comfortable for NIPPV than volume-limited ventilation.50 However, leaks during noninvasive ventilation can interfere with the detection of reduced inspiratory flow at the termination of inspiration, causing expiratory asynchrony. Noninvasive pressure-limited modes of ventilation are usually administered using either standard critical care ventilators or portable bilevel ventilators.
Traditional bilevel devices designed for home use have limited pressure-generating capability (≤30 cm H2O) and lack oxygen blenders or sophisticated alarm or battery backup systems, precluding their use in patients who require high oxygen concentrations or inflation pressures. Newer versions designed for the acute setting are equipped with sophisticated alarm and monitoring capabilities, graphic displays, and oxygen blenders. These devices are capable of enhancing synchrony by offering ways to limit inspiratory duration and an adjustable “rise time”—the time to reach the targeted inspiratory pressure. Many critical care ventilators now include an “NIV” mode that enhances leak compensation capabilities and silences “nuisance” alarms, but many of these have difficulty maintaining performance in the face of variable air leaks.51 If desired, volume-limited ventilation can be delivered using critical care ventilators, but a higher tidal volume than that commonly used for invasive mechanical ventilation is recommended to compensate for air leakage.
Initial ventilator pressure settings are usually low to facilitate patient acceptance, but they can be set higher if necessary to alleviate respiratory distress. Typical starting pressures are an inspiratory positive airway pressure of 10 to 12 cm H2O and a PEEP (or expiratory positive airway pressure) of 4 to 5 cm H2O. L’Her et al.52 demonstrated that increases in inspiratory pressure are helpful to alleviate dyspnea, whereas increases in expiratory pressure are better to improve oxygenation. For volume ventilation, initial tidal volumes range from 6 to 7 mL/kg. The ventilator is set in a spontaneously triggered mode, with or without a backup rate. Pressures commonly used to deliver CPAP in patients with acute respiratory distress range from 5 to 12.5 cm H2O. CPAP can be applied using compressed air with a regulator system, blower-based CPAP devices, bilevel devices, or critical care ventilators.
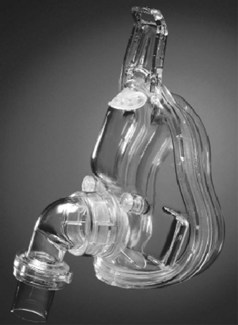
Interfaces
Full facemasks cover both the nose and the mouth (Figure 51-3) and are preferable to nasal masks in the acute setting. The efficacy of both nasal and oronasal masks in lowering PaCO2 and avoiding intubation is similar in the acute setting, but a randomized controlled trial53 observed better patient tolerance with full facemasks because of reduced air leakage through the mouth. More recently, a “total” facemask has become available; it seals around the perimeter of the face and resembles a hockey goalie’s mask. Made of optical-grade plastic, it is easy to apply and causes no more claustrophobia than standard facemasks. Mouthpieces are seldom used to administer noninvasive ventilation in the acute setting but are occasionally used during initiation, when the patient holds the mouthpiece in place to adapt to the sensation of positive-pressure ventilation.
Monitoring
Once noninvasive ventilation is initiated, patients should be closely monitored in a critical care or step-down unit until they are sufficiently stable to be moved to a regular medical floor. The aim of monitoring is to determine whether the main goals are being achieved, including relief of symptoms, reduced work of breathing, improved or stable gas exchange, good patient-ventilator synchrony, and patient comfort (Box 51-3). A drop in the respiratory rate with improved oxygen saturation or improving pH with a lower PaCO2 within the first 1 to 2 hours portends a successful outcome.54 Abdominal paradox, if present initially, subsides, and the heart rate usually falls. The absence of these propitious signs indicates a poor response to noninvasive ventilation and the need to make further adjustments. Leaks should be sought and corrected, patient-ventilator synchrony should be optimized, and pressures may have to be adjusted upward to relieve respiratory distress and achieve a reduction in PaCO2. If these adjustments fail to improve the response within a few hours, noninvasive ventilation should be considered a failure, and the patient should be promptly intubated if it is still clinically indicated. Excessive delay in intubation may precipitate a respiratory crisis and add to morbidity and mortality.
Key Points
Antonelli M, Conti G, Esquinas A, et al. A multiple-center survey on the use in clinical practice of noninvasive ventilation as a first-line intervention for acute respiratory distress syndrome. Crit Care Med. 2007;35:18-25.
Demoule A, Girou E, Richard JC, Taillé S, Brochard L. Increased use of noninvasive ventilation in French intensive care units. Intensive Care Med. 2006;32:1747-1755.
Farha S, Ghamra ZW, Hoisington ER, Butler RS, Stoller JK. Use of noninvasive positive-pressure ventilation on the regular hospital ward: experience and correlates of success. Respir Care. 2006;51:1237-1243.
Ferrer M, Sellares J, Valencia M, et al. Non-invasive ventilation after extubation in hypercapnic patients with chronic respiratory disorders: randomised controlled trial. Lancet. 2009;374:1082-1088.
Maheshwari V, Paioli D, Rothaar R, Hill NS. Utilization of noninvasive ventilation in acute care hospitals: a regional survey. Chest. 2006;129:1226-1233.
Winck JC, Azevedo LF, Costa-Pereira A, Antonelli M, Wyatt JC. Efficacy and safety of non-invasive ventilation in the treatment of acute cardiogenic pulmonary edema—a systematic review and meta-analysis. Crit Care. 2006;10:R69.
1 Hill NS. Clinical applications of body ventilators. Chest. 1986;90:897-905.
2 Lassen HA. A preliminary report on the 1952 epidemic of poliomyelitis in Copenhagen. Lancet. 1953;1:37.
3 Hill NS, Carlisle C, Kramer NR. Effect of a nonrebreathing valve on long-term nasal ventilation using a bilevel device. Chest. 2002;122:84-91.
4 Demoule A, Girou E, Richard JC, Taille S, Brochard L. Increased use of noninvasive ventilation in French intensive care units. Intensive Care Med. Nov 2006;32(11):1747-1755.
5 Ozsancak AAP, Khodabandeh A, Maheshwari V, Hill NS. Increasing utilization of non-invasive positive pressure ventilation in acute care hospitals in Massachusetts and Rhode Island. Am J Respir Crit Care Med. 2008;177:A283. May 2008
6 Griesdale DE, Bosma TL, Kurth T, Isac G, Chittock DR. Complications of endotracheal intubation in the critically ill. Intensive Care Med. Oct 2008;34(10):1835-1842.
7 Nourdine K, Combes P, Carton MJ, et al. Does noninvasive ventilation reduce the ICU nosocomial infection risk? A prospective clinical survey. Intensive Care Med. 1999;25:567-573.
8 Antonelli M, Conti G, Rocco M, et al. A comparison of noninvasive positive-pressure ventilation and conventional mechanical ventilation in patients with acute respiratory failure. N Engl J Med. 1998;339:429-435.
9 Girou E, Schorten F, Delclaux C, et al. Association of noninvasive ventilation with nosocomial infections and survival in critically ill patients. JAMA. 2000;284:2361-2367.
10 Tomii K, Seo R, Tachikawa R, et al. Impact of noninvasive ventilation (NIV) trial for various types of acute respiratory failure in the emergency department; decreased mortality and use of the ICU. Respir Med. Jan 2009;103(1):67-73.
11 Appendini L, Palessio A, Zanaboni S, et al. Physiologic effects of positive end-expiratory pressure and mask pressure support during exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1994;149:1069-1076.
12 Brochard L, Mancebo J, Wysocki M, et al. Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med. 1995;333:817-822.
13 Plant PK, Owen JL, Elliott MW. Early use of non-invasive ventilation for acute exacerbations of chronic obstructive pulmonary disease on general respiratory wards: a multicentre randomised controlled trial. Lancet. 2000 Jun 3;355(9219):1931-1935.
14 Lightowler JV, Wedzicha JA, Elliott MW, Ram FS. Noninvasive positive pressure ventilation to treat respiratory failure resulting from exacerbations of chronic obstructive pulmonary disease: Cochrane systematic review and meta-analysis. BMJ. 2003;326:185-189.
15 Jaber S, Fodil R, Carlucci A, et al. Noninvasive ventilation with helium-oxygen in acute exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000.
16 Jolliet P, Tassaux D, Roeseler J, et al. Helium-oxygen versus air-oxygen noninvasive pressure support in decompensated chronic obstructive disease: A prospective, multicenter study. Crit Care Med. 2003;31:878-884.
17 Soroksky A, Stav D, Shpirer I. A pilot prospective, randomized, placebo-controlled trial of bilevel positive airway pressure in acute asthmatic attack. Chest. 2003;123:1018-1025.
18 Soma T, Hino M, Kida K, Kudoh S. A prospective and randomized study for improvement of acute asthma by non-invasive positive pressure ventilation (NPPV). Intern Med. 2008;47(6):493-501.
19 Madden BP, Kariyawasam H, Siddiqi AJ, et al. Noninvasive ventilation in cystic fibrosis patients with acute or chronic respiratory failure. Eur Respir J. 2002;19:310-313.
20 Ferrer M, Esquinas A, Leon M, Gonzalez G, Alarcon A, Torres A. Noninvasive ventilation in severe hypoxemic respiratory failure: a randomized clinical trial. Am J Respir Crit Care Med. Dec 15 2003;168(12):1438-1444.
21 Antonelli M, Conti G, Moro ML, et al. Predictors of failure of noninvasive positive pressure ventilation in patients with acute hypoxemic respiratory failure: a multi-center study. Intensive Care Med. 2001;27:1718-1728.
22 Confalonieri M, Potena A, Carbone G, et al. Acute respiratory failure in patients with severe community-acquired pneumonia. Am J Respir Crit Care Med. 1999;160:1585-1591.
23 Jolliet P, Abajo B, Pasquina P. Noninvasive ventilation in severe community acquired pneumonia. Intensive Care Med. 2001;27:812-821.
24 Antonelli M, Conti G, Bufi M, et al. Noninvasive ventilation for treatment of acute respiratory failure in patients undergoing solid organ transplantation: a randomized trial. JAMA. 2000;283:235-241.
25 Hilbert G, Gruson D, Vargas F, et al. Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever, and acute respiratory failure. N Engl J Med. 2001;344:481-487.
26 Confaloreni M, Calderni E, Terraciano S, et al. Noninvasive ventilation for treating acute respiratory failure in AIDS patients with PCP pneumonia. Intensive Care Med. 2002;28:1233-1238.
27 Rocker GM, Mackenzie MG, Williams B, Logan PM. Noninvasive positive pressure ventilation: successful outcome in patients with acute lung injury/ARDS. Chest. 1999;115:173-177.
28 Antonelli M, Conti G, Esquinas A, et al. A multiple-center survey on the use in clinical practice of noninvasive ventilation as a first-line intervention for acute respiratory distress syndrome. Crit Care Med. Jan 2007;35(1):18-25.
29 Masip J, Roque M, Sanchez B, Fernandez R, Subirana M, Exposito JA. Noninvasive ventilation in acute cardiogenic pulmonary edema: systematic review and meta-analysis. JAMA. Dec 28 2005;294(24):3124-3130.
30 Winck JC, Azevedo LF, Costa-Pereira A, Antonelli M, Wyatt JC. Efficacy and safety of non-invasive ventilation in the treatment of acute cardiogenic pulmonary edema–a systematic review and meta-analysis. Crit Care. 2006;10(2):R69.31.
31 Nava S, Hill N. Non-invasive ventilation in acute respiratory failure. Lancet. 2009 Jul 18;374(9685):250-259.
32 Ferreyra GP, Baussano I, Squadrone V, et al. Continuous positive airway pressure for treatment of respiratory complications after abdominal surgery: a systematic review and meta-analysis. Ann Surg. Apr 2008;247(4):617-626.
33 Kindgen-Milles D, Muller E, Buhl R, et al. Nasal-continuous positive airway pressure reduces pulmonary morbidity and length of hospital stay following thoracoabdominal aortic surgery. Chest. Aug 2005;128(2):821-828.
34 Auriant I, Jallot A, Herve P. Noninvasive ventilation reduces mortality in acute respiratory failure following lung resection. Am J Respir Crit Care Med. 2001;164:1231-1235.
35 Joris JL, Sottiaux TM, Chiche JD, et al. Effect of bilevel positive airway pressure (BiPAP) nasal ventilation on the postoperative pulmonary restrictive syndrome in obese patients undergoing gastroplasty. Chest. 1997;111:665-670.
36 Beltrame F, Lucangelo U, Gregory D, Gregoretti C. Noninvasive positive pressure ventilation in trauma patients with acute respiratory failure. Monaldi Arch Chest Dis. 1999;54:109-114.
37 Hernandez G, Fernandez R, Lopez-Reina P, et al. Noninvasive ventilation reduces intubation in chest trauma-related hypoxemia: a randomized clinical trial. Chest. Jan 2010;137(1):74-80.
38 Rabenstein A, Widjicks EF. BiPAP in acute respiratory failure due to myasthenic crisis may prevent intubation. Neurology. 2002;59:1647-1649.
39 Fumeaux T, Rothmeier C, Jolliet P. Outcome of mechanical ventilation for acute respiratory failure in patients with pulmonary fibrosis. Intensive Care Med. 2001;27:1868-1874.
40 Levy M, Tanios MA, Nelson D, et al. Outcomes of patients with do-not-intubate orders treated with noninvasive ventilation. Crit Care Med. Oct 2004;32(10):2002-2007.
41 Curtis JR, Cook DJ, Sinuff T, et al. Noninvasive positive pressure ventilation in critical and palliative care settings: understanding the goals of therapy. Crit Care Med. Mar 2007;35(3):932-939.
42 Nava S, Ambrosino N, Clini E, et al. Noninvasive mechanical ventilation in the weaning of patients with respiratory failure due to chronic obstructive pulmonary disease: a randomized, controlled trial. Ann Intern Med. 1998;128:721-728.
43 Girault C, Daudenthum I, Chevron V, et al. Noninvasive ventilation as a systematic extubation and weaning technique in acute or chronic respiratory failure: a prospective, randomized controlled study. Am J Respir Crit Care Med. 1999;160:86-92.
44 Ferrer M, Esquinas A, Arancibia F, et al. Noninvasive ventilation during persistent weaning failure: A randomized controlled trial. Am J Respir Crit Care Med. 2003;168:70-76.
45 Esteban A, Frutos-Vivar F, Ferguson ND, et al. Noninvasive positive-pressure ventilation for respiratory failure after extubation. N Engl J Med. Jun 10 2004;350(24):2452-2460.
46 Ferrer M, Valencia M, Nicolas JM, Bernadich O, Badia JR, Torres A. Early noninvasive ventilation averts extubation failure in patients at risk: a randomized trial. Am J Respir Crit Care Med. Jan 15 2006;173(2):164-170.
47 Ferrer M, Sellares J, Valencia M, et al. Non-invasive ventilation after extubation in hypercapnic patients with chronic respiratory disorders: randomised controlled trial. Lancet. Sep 26 2009;374(9695):1082-1088.
48 Maitre B, Jaber S, Maggiore SM, et al. Continuous positive airway pressure during fiberoptic bronchoscopy in hypoxemic patients: a randomized double-blind study using a new device. Am J Respir Crit Care Med. 2000;162:1063-1067.
49 Antonelli M, Conti G, Rocco M, et al. Noninvasive positive-pressure ventilation vs conventional oxygen supplementation in hypoxemic patients undergoing diagnostic bronchoscopy. Chest. 2002;121:1149-1154.
50 Vitacca M, Rubini F, Foglio K. Noninvasive modalities of positive pressure ventilation improve the outcome of acute exacerbation of COLD patients. Intensive Care Med. 1993;19:450-455.
51 Ferreira JC, Chipman DW, Hill NS, Kacmarek RM. Bilevel vs ICU ventilators providing noninvasive ventilation: effect of system leaks: a COPD lung model comparison. Chest. 2009 Aug;136(2):448-456.
52 L’Her E, Deye N, Lellouche F, Taille S, Demoule A, Fraticelli A, et al. Physiologic effects of noninvasive ventilation during acute lung injury. Am J Respir Crit Care Med. 2005 Nov 1;172(9):1112-1118.
53 Kwok H, McCormack J, Cece R, et al. Controlled trial of oronasal versus mask ventilation in the treatment of acute respiratory failure. Crit Care Med. 2003;123:949-952.
54 Soo Hoo GW, Santiago S, Williams J. Nasal mechanical ventilation for hypercapnic respiratory failure in chronic obstructive pulmonary disease: determinants of success and failure. Crit Care Med. 1994;27:417-434.