CHAPTER 8 Nonarthroplasty Treatment Options for Unicompartmental Degenerative Joint Disease
Arthroscopic Débridement
Mechanical symptoms associated with meniscal or chondral lesions are the clearest indication for arthroscopic débridement. However, patient expectations need to be clearly defined, and patients should be cautioned that a significant portion of their knee pain might be attributed to the existing arthritis. Multiple authors have shown improvement in knee rating score, improved knee function, decreased anti-inflammatory use, and high patient satisfaction in osteoarthritic knees treated with arthroscopic lavage and débridement.1–4 Steadman et al.’s systematic arthroscopic approach to the degenerative knee included the expansion of joint space through the release of joint contractures, removal of loose bodies, limited chondroplasty, meniscectomy of unstable tears, thermal ablation of synovitis, and excision of osteophytes blocking full extension.4 Their published results on a consecutive series of patients with severe arthritis who underwent the procedure showed that greater than 70% of them had significant gains in knee function scores, satisfaction, and delay of arthroplasty at a minimum of 3 years postoperatively.4
The most cited predictors of failure of arthroscopic intervention include malalignment greater than 5°, age greater than 60, persistent symptoms greater than 1 year, history of prior surgery, and joint space less than 2 mm.5–9 Steadman et al. added the presence of “kissing” grade 4 lesions and severity of joint contracture as additional independent predictors of failure. The preoperative presence of a symptomatic mechanical lesion seems to be the most reproducible predictor of success from arthroscopic débridement. Multiple authors have shown persistent symptomatic benefit in patients with combined meniscal pathology and degenerative changes treated with partial meniscectomy, but better results are seen if the meniscal component is acute rather than degenerative.9–13
In contrast to the multiple reports of success with arthroscopic débridement in osteoarthritis, Moseley et al. and Kirkley et al. demonstrated equal efficacy between a focused physical therapy program and arthroscopic débridement.14,15 Moseley et al. also reported similar outcomes with a “sham-operation” highlighting the power of the placebo effect.14 Their interpretation of these results has caused many clinicians to question the utility of arthroscopy in the setting of osteoarthritis.14,15 However, some surgeons criticize these studies for lacking a specific patient cohort with arthritis but predominating mechanical symptoms. The randomized nature of these two studies does demonstrate that the blind application of arthroscopic débridement to osteoarthritis is unlikely to produce successful outcomes greater than nonsurgical treatments and highlights the importance of critically analyzing the patient’s symptomatology and applying strict patient selection criteria.
Cartilage Restoration
There are multiple, well-studied restorative options for the treatment of acute full-thickness articular cartilage defects. The most common options include microfracture, osteochondral transfer, and autologous chondrocyte transplantation. Despite the continued debate surrounding the appropriate indications and expected longevity for these procedures, one can expect good to excellent results when these restorative options are applied appropriately to the acute full-thickness lesion. On the contrary, most attempts at cartilage restoration will fail in the setting of significant degenerative disease. It is thought that the osteoarthritic environment is not conducive to these techniques and that either the cartilage at the periphery of the degenerative lesion is too thin to contain the repair or the surrounding cartilage will continue to degenerate. In a review of microfracture in the degenerative knee, there were significant gains in Lysholm scores but the improvement in function was less when compared to their “traumatic” counterpart (Fig. 8–1).16 Larger lesions, older patients, those lesions defined as “degenerative” rather than “traumatic,” and bipolar lesions all were associated with less improvement in knee function scores.16 Andres et al.’s review of osteochondral autograft transplantation demonstrated significantly greater improvements in the pain relief and function of the “isolated lesion” group compared to the “degenerative lesion” group.17 In a diverse group of patients treated with autologous chondrocyte implantation, McNickle et al. found that age was an independent predictor of postoperative Lysholm score, with less improvement in older patients.18
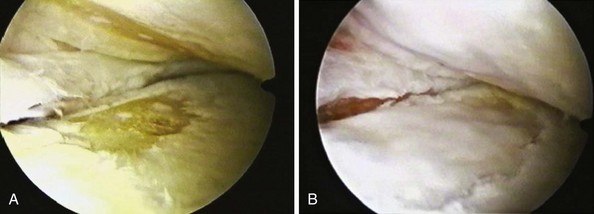
Figure 8–1 Degenerative chondral defects before microfracture (A) and after microfracture (B).
(Photos courtesy of Dr. William Sterett, Steadman-Hawkins Clinic, Vail, CO.)
Despite the mounting evidence against cartilage restorative attempts in significant degenerative disease, some advocate these techniques as an adjunct to other joint-preservative procedures such as high tibial osteotomy and meniscal allograft. Gomoll et al. reported on successful outcomes at 2 years postoperatively using the “Triad of Cartilage Restoration”: meniscal allograft transplantation, cartilage repair, and osteotomy.19 Marrow stimulation techniques have been shown to improve early outcomes of osteotomy, and second-look arthroscopy has demonstrated maintenance of the reparative tissue.20–22 However, Matsunaga et al. questioned the utility of adjunctive marrow stimulation with osteotomy when they showed no significant difference in 5-year clinical outcome between the marrow stimulation and nonreparative groups.22 Successful treatment of unicompartmental disease with current restorative techniques remains a challenge. The development of biologic scaffolds, platelet-rich gels, stem cell augmentation, and articular allografts are promising potential solutions for unicompartmental arthrosis, but their current use remains controversial and investigational.
High Tibial Osteotomy
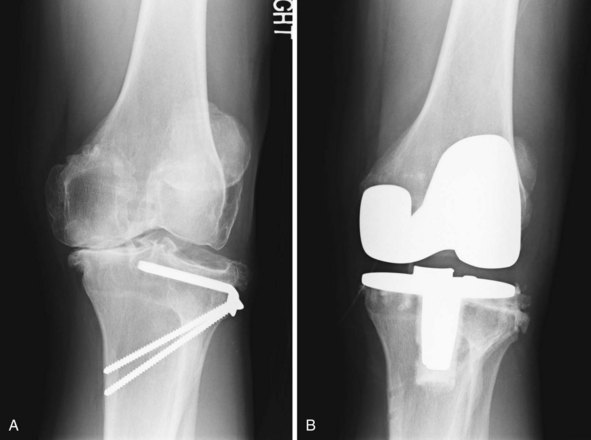
High tibial osteotomy is indicated in patients with significant medial osteoarthritis and concomitant varus deformity. The improvement in medial unicompartmental arthroplasty design and clinical outcomes has significantly decreased the popularity of high tibial osteotomy. In addition, the conversion of a high tibial osteotomy to a total knee arthroplasty is complicated by multiple factors, including the presence of hardware, changes in the patellofemoral anatomy, scarring, and previous incisions (Fig. 8–2). Therefore, the indications for high tibial osteotomy have narrowed to younger, active patients with isolated medial arthrosis for whom arthroplasty is contraindicated. High tibial osteotomy is also indicated in patients who need medial compartment off-loading secondary to concomitant medial compartment cartilage restoration or meniscal allograft.
Multiple long-term studies of the clinical results of high tibial osteotomy demonstrate reproducible improvement in Lysholm knee scores, decrease in pain scores, and high patient satisfaction.20,21,23–31 Survivorship and percentage of good to excellent results at 5 years tend to be between 80% and 90%; however, there is a steady deterioration of the survivorship to between 50% and 60% at 10 years.20,23–27 This consistent decline in efficacy suggests that high tibial osteotomy postpones the need for total knee arthroplasty rather than actually preventing it.
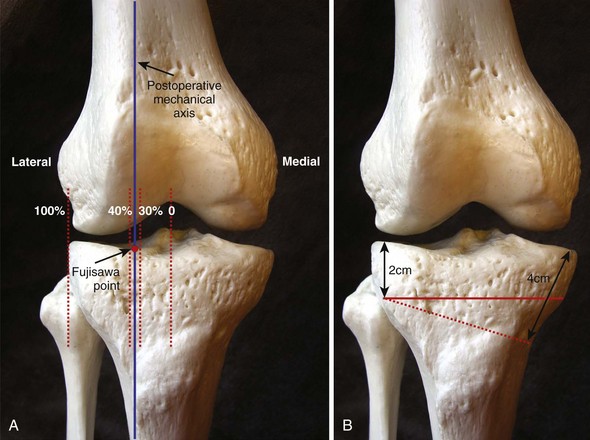
Multiple different tibial osteotomy techniques have been described, including lateral closing wedge, medial opening wedge, and dome osteotomies. In addition, the fixation types have also varied between casting, external fixation, and plate fixation. Regardless of the technique, the ultimate goal of the procedure is to shift the mechanical axis from the diseased medial compartment to the preserved lateral compartment. It is commonly accepted to shift the mechanical axis into slight valgus so that the anatomic valgus angle is approximately 8–10°.23,28 Fujisawa et al. found that postoperative success correlated with a postoperative mechanical axis that crossed the lateral compartment at a point 30–40% of the distance between the center and lateral edge of the plateau (see Fig. 8–2A).28 The accuracy of the correction is of paramount importance because excessive overcorrection and undercorrection have been shown to be intimately associated with suboptimal satisfaction and durability of the procedure.29–31 Other factors that have been shown to contribute to the deterioration of high tibial osteotomy include age older than 60, ligamentous instability, obesity, concomitant lateral compartment disease, poor preoperative range of motion, and greater than 12° of preoperative angular deformity.26,31
Conversion of high tibial osteotomy to total knee arthroplasty is technically more demanding than a primary total knee arthroplasty. An oblique medial opening wedge osteotomy at the level of the tibial tubercle has been shown to have less of an effect on patellar height and tibial slope than a traditional horizontal osteotomy and should conceivably allow for easier conversion to total knee arthroplasty (see Fig. 8–1B).32 However, it is important to aim the oblique osteotomy toward the lateral metaphyseal flare approximately 2–3 cm below the lateral joint line because failure is associated with osteotomies that are too distal on the lateral cortex (Fig. 8–3).32 The use of external fixation with or without distraction osteogenesis can eliminate the hardware concerns, but pin tract infections are a significant problem especially when a future implant is likely. Biocompatible hardware options with PEEK (polyether ether ketone) or trabecular metals could obviate hardware concerns during conversion; however, there are no such implants currently available.
Distal Femoral Osteotomy
Varus-producing distal femoral osteotomy is indicated in patients with lateral compartment disease and concomitant valgus malalignment. Similar to high tibial osteotomy, distal femoral osteotomy is indicated in younger patients for whom a unicompartmental arthroplasty is contraindicated due to young age or high activity level. Medial closing wedge or lateral opening wedge are the most common surgical techniques, and larger deformities are best treated with the lateral opening wedge osteotomy. Like the high tibial osteotomy, the results are excellent in the first 5 years, but the survivorship has a predictable decline after 10 years.33,34 Subsequent conversion to total knee arthroplasty is a challenge, and the results are inferior to that of primary knee arthroplasty.35 Outside of the hardware complications and difficulty with intramedullary guidance, the most common problems encountered are instability necessitating a constrained prosthesis and the tendency to place the femoral component into varus angulation.34 Therefore, extramedullary guidance, computer-assisted technology, or axial image-based systems may be of considerable utility when converting a distal femoral osteotomy to total knee arthroplasty.
1 Livesley PJ, Doherty M, Needoff M, Moulton A. Arthroscopic lavage of osteoarthritic knees. J Bone Joint Surg [Br]. 1991;73:922-926.
2 Edelson R, Burks RT, Bloebaum RD. Short-term effects of knee washout for osteoarthritis. Am J Sports Med. 1995;23:345-349.
3 Merchan EC, Galindo E. Arthroscope-guided surgery versus nonoperative treatment for limited degenerative osteoarthritis of the femorotibial joint in patients over 50 years of age: a prospective comparative study. Arthroscopy. 1993;9:663-667.
4 Steadman JR, Ramappa AJ, Maxwell RB, Briggs KK. An arthroscopic treatment regimen for osteoarthritis of the knee. Arthroscopy. 2007;23:948-955.
5 Salisbury RB, Nottage WM, Gardner V. The effect of alignment on results in arthroscopic debridement of the degenerative knee. Clin Orthop Relat Res. 1985;198:268-272.
6 Harwin SF. Arthroscopic debridement for osteoarthritis of the knee: predictors of patient satisfaction. Arthroscopy. 1999;15:142-146.
7 Wouters E, Bassett FH3rd, Hardaker WTJr, Garrett WEJr. An algorithm for arthroscopy in the over-50 age group. Am J Sports Med. 1992;20:141-145.
8 Ogilvie-Harris DJ, Fitsialos DP. Arthroscopic management of the degenerative knee. Arthroscopy. 1991;7:151-157.
9 Aichroth PM, Patel DV, Moyes ST. A prospective review of arthroscopic debridement for degenerative joint disease of the knee. Int Orthop. 1991;15:351-355.
10 Rand JA. Arthroscopic management of degenerative meniscus tears in patients with degenerative arthritis. Arthroscopy. 1985;1:253-258.
11 McBride GG, Constine RM, Hofmann AA, Carson RW. Arthroscopic partial medial meniscectomy in the older patient. J Bone Joint Surg [Am]. 1984;66:547-551.
12 Barrett GR, Treacy SH, Ruff CG. The effect of partial lateral meniscectomy in patients > or = 60 years. Orthopedics. 1998;21:251-257.
13 Jackson RW, Rouse DW. The results of partial arthroscopic meniscectomy in patients over 40 years of age. J Bone Joint Surg [Br]. 1982;64:481-485.
14 Moseley JB, O’Malley K, Petersen NJ, et al. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002;347:81-88.
15 Kirkley A, Birmingham TB, Litchfield RB, et al. A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2008;359:1097-1107. [published erratum appears in N Engl J Med 2009;361:2004]
16 Miller BS, Steadman JR, Briggs KK, et al. Patient satisfaction and outcome after microfracture of the degenerative knee. J Knee Surg. 2004;17:13-17.
17 Andres BM, Mears SC, Somel DS, et al. Treatment of osteoarthritic cartilage lesions with osteochondral autograft transplantation. Orthopedics. 2003;26:1121-1126.
18 McNickle AG, L’Heureux DR, Yanke AB, Cole BJ. Outcomes of autologous chondrocyte implantation in a diverse patient population. Am J Sports Med. 2009;37:1344-1350.
19 Gomoll AH, Kang RW, Chen AL, Cole BJ. Triad of cartilage restoration for unicompartmental arthritis treatment in young patients: meniscus allograft transplantation, cartilage repair and osteotomy. J Knee Surg. 2009;22:137-141.
20 Sterett WI, Steadman JR, Huang MJ, et al. Chondral resurfacing and high tibial osteotomy in the varus knee: survivorship analysis. Am J Sports Med. 2010;38:1420-1424.
21 Miller BS, Joseph TA, Barry EM, et al. Patient satisfaction after medial opening high tibial osteotomy and microfracture. J Knee Surg. 2007;20:129-133.
22 Matsunaga D, Akizuki S, Takizawa T, et al. Repair of articular cartilage and clinical outcome after osteotomy with microfracture or abrasion arthroplasty for medial gonarthrosis. Knee. 2007;14:465-471.
23 Hernigou P, Medevielle D, Debeyre J, Goutallier D. Proximal tibial osteotomy for osteoarthritis with varus deformity: a ten to thirteen-year follow-up study. J Bone Joint Surg [Am]. 1987;69:332-354.
24 Insall JN, Joseph DM, Msika C. High tibial osteotomy for varus gonarthrosis: a long-term follow-up study. J Bone Joint Surg [Am]. 1984;66:1040-1048.
25 Sprenger TR, Doerzbacher JF. Tibial osteotomy for the treatment of varus gonarthrosis: survival and failure analysis to twenty-two years. J Bone Joint Surg [Am]. 2003;85:469-474. [published erratum appears in J Bone Joint Surg [Am] 2003;85:912]
26 Berman AT, Bosacco SJ, Kirshner S, Avolio AJr. Factors influencing long-term results in high tibial osteotomy. Clin Orthop Relat Res. 1991;272:192-198.
27 Rinonapoli E, Mancini GB, Corvaglia A, Musiello S. Tibial osteotomy for varus gonarthrosis: a 10- to 21-year follow-up study. Clin Orthop Relat Res. 1998;353:185-193.
28 Fujisawa Y, Masuhara K, Shiomi S. The effect of high tibial osteotomy on osteoarthritis of the knee: an arthroscopic study of 54 knee joints. Orthop Clin North Am. 1979;10:585-608.
29 Matthews LS, Goldstein SA, Malvitz TA, et al. Proximal tibial osteotomy: factors that influence the duration of satisfactory function. Clin Orthop Relat Res. 1988;229:193-200.
30 Coventry MB, Ilstrup DM, Wallrichs SL. Proximal tibial osteotomy: a critical long-term study of eighty-seven cases. J Bone Joint Surg [Am]. 1993;75:196-201.
31 Pfahler M, Lutz C, Anetzberger H, et al. Long-term results of high tibial osteotomy for medial osteoarthritis of the knee. Acta Chir Belg. 2003;103:603-606.
32 Matar WY, Boscariol R, Dervin GF. Open wedge high tibial osteotomy: a roentgenographic comparison of a horizontal and an oblique osteotomy on patellar height and sagittal tibial slope. Am J Sports Med. 2009;37:735-742.
33 Kosashvili Y, Safir O, Gross A, et al. Distal femoral varus osteotomy for lateral osteoarthritis of the knee: a minimum ten-year follow-up. Int Orthop. 2010;34:249-254.
34 Aglietti P, Menchetti PP. Distal femoral varus osteotomy in the valgus osteoarthritic knee. Am J Knee Surg. 2000;13:89-95.
35 Nelson CL, Saleh KJ, Kassim RA, et al. Total knee arthroplasty after varus osteotomy of the distal part of the femur. J Bone Joint Surg [Am]. 2003;85:1062-1065.