9 Non-surgical skin tightening
Summary and Key Features
• Non-invasive skin tightening is a popular concept with a burgeoning number of devices entering the market
• The main types of non-surgical skin tightening devices include radiofrequency, light, and ultrasound technologies
• Treatment protocols have evolved over the years to focus on reduced energy settings, making the procedures safer and more comfortable for patients
• All skin-tightening devices work by delivering heat in the form of energy to the skin or underlying structures. They create mechanical and biochemical effects that lead to both immediate contraction of collagen fibers and delayed remodeling and neocollagenesis via wound healing
• Patient selection is key for best results and overall patient satisfaction
• Patients who are concerned about risk and recovery and who are willing to accept reduced efficacy in exchange for an improved side effect and healing time profile are ideal candidates for non-ablative approaches
• Non-ablative skin-tightening devices are capable of improving both skin laxity and facial contours. The physician must analyze the patient’s three-dimensional facial structure to determine those areas that would benefit most from the procedure. Typically, this would include the upper face / brow region and the lower face / jawline region
• Skin-tightening procedures can be performed along with fillers, neurotoxins or other laser or light-based devices to address multiple issues and achieve a more global overall improvement
• Rarely, patients may experience side effects related to overly aggressive treatment such as burns, indentations, scars or changes in pigmentation. The overall incidence of such problems is extremely low with all current devices owing to updated protocol trends using lower energies and patient feedback as a guide to safe energy delivery
Introduction
In terms of skin laxity specifically, the gold standard of treatment remains rhytidectomy or surgical redraping. The goal of this chapter is to review the major types of minimally invasive, non-ablative tissue tightening techniques, including radiofrequency-, light-, and ultrasound-based devices (Table 9.1). These devices are not a replacement for surgical procedures and appropriate patient selection remains key to overall satisfaction.
| Skin-tightening technology | Device |
|---|---|
| Monopolar radiofrequency | Thermage® (Solta) |
| Pelleve® (Ellman) | |
| Bipolar radiofrequency with light energy | Galaxy®, Aurora®, Polaris®, ReFirme® (Syneron) |
| Bipolar radiofrequency with vacuum | Aluma® (Lumenis) |
| Bipolar radiofrequency delivered via a micro-needle electrode array | ePrime® (Candela-Syneron) |
| Broadband infrared light | Titan® (Cutera) |
| StarLux IR® (Palomar) | |
| SkinTyte® (Sciton) | |
| Unipolar and bipolar radiofrequency | Accent® (Alma) |
| Ultrasound technology | Ulthera® (Ulthera) |
Thermal collagen remodeling
All skin-tightening devices work by delivering heat in the form of energy to the skin or underlying structures. This creates mechanical and biochemical effects that lead to both immediate contraction of collagen fibers and delayed remodeling and neocollagenesis via a wound-healing response (Box 9.1).
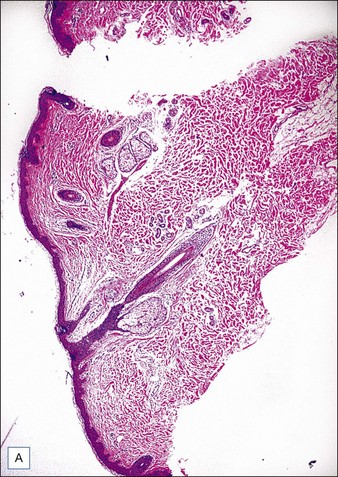
Collagen fibers are composed of a triple helix of protein chains linked with interchain bonds into a crystalline structure. When collagen fibers are heated to specific temperatures, they contract due to breakage of intramolecular hydrogen bonds. Contraction causes the crystalline triple helix structure to fold, creating thicker and shorter collagen fibers. This is thought to be the mechanism of action of immediate tissue tightening seen after skin-tightening procedures. Studies have also found selective contraction of fibrous septae in the subcutaneous fat, which is thought to be responsible for the inward (Z-dimension) tightening (Fig. 9.1).
Radiofrequency devices
Radiofrequency energy is energy in the electromagnetic spectrum ranging from 300 MHz to 3 kHz. Unlike most lasers, which target specific absorption bands of chromophores, heat is generated from the natural resistance of tissue to the movement of electrons within the radiofrequency field as governed by Ohm’s law (Box 9.2). This resistance, called impedance, generates heat relative to the amount of current and time by converting electrical current to thermal energy. Consequently, energy is dispersed to three-dimensional volumes of tissue at controlled depths.
The configuration of electrodes in a radiofrequency device can be monopolar or bipolar, and both have been used for cutaneous applications. The main difference between the two is the configuration of electrodes and type of electromagnetic field that is generated. In a monopolar system, the electrical current passes through a single electrode in the handpiece to a grounding pad (Box 9.3). This type of electrode configuration is common in surgical radiofrequency devices because there is a high density of power close to the electrode’s surface with the potential for deep penetration of tissue heating. In tissue-tightening applications, surface cooling is used to protect the outer layers of the skin and heat only deeper targets. In a bipolar system, the electrical current passes between two electrodes at a fixed distance (Box 9.4). This type of electrode configuration has a more controlled current distribution; however, the depth of penetration is limited to approximately one-half the distance between the electrodes.
With radiofrequency technologies, the depth of energy penetration depends upon not only the configuration of the electrodes (i.e. either monopolar or bipolar), but also the type of tissue serving as the conduction medium (i.e. fat, blood, skin), temperature, and the frequency of the electrical current applied (Box 9.5). Tissue is made up of multiple layers, including dermis, fat, muscle, and fibrous tissue, all of which have different resistances to the movement of radiofrequency energy (Table 9.2). Structures with higher impedance are more susceptible to heating. In general, fat, bone, and dry skin tend to have low conductivities such that current tends to flow around these structures rather than through them. Wet skin has a higher electrical conductivity allowing greater penetration of current. This is why, in certain radiofrequency procedures, improved results can be seen with generous amounts of coupling fluid and increased hydration of skin. The structure of each individual’s tissue (dermal thickness, fat thickness, fibrous septae, number and size of adnexal structures) all play a role in determining impedance, heat perception, and total deposited energy despite otherwise equal parameters.
Table 9.2 Dielectric properties for human tissue at 1 MHz and room temperature
| Type of tissue | Electrical conductivity (Siemens/m) |
|---|---|
| Bone | 0.02 |
| Fat | 0.03 |
| Dry skin | 0.03 |
| Nerve | 0.13 |
| Cartilage | 0.23 |
| Wet skin | 0.22 |
| Muscle | 0.50 |
| Thyroid | 0.60 |
Monopolar radiofrequency
The first monopolar tissue-tightening device on the market was the ThermaCool® device (Solta Medical, Hayward, CA), introduced in 2001. It remains the most exhaustively studied and published apparatus. The ThermaCool® device uses a capacitive coupled electrode at a single contact point and a high-frequency current at a frequency of 6 MHz. A disposable membrane tip is used to deliver the energy into the skin, with an accompanying adhesive grounding pad serving as a low-resistance path for current flow to complete the circuit. The use of capacitive rather than conductive coupling is important because it allows the energy to be dispersed across a surface to create a zone of tissue heating. With conductive coupling, the energy is concentrated at the tip of the electrode, resulting in increased heating at the contact surface and an increased risk of epidermal injury (Fig. 9.2).

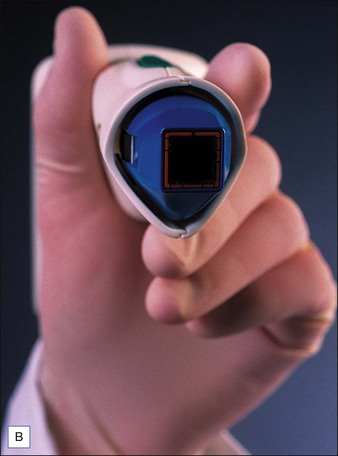
Figure 9.2 (A) Thermage ThermaCool® device; (B) capacitively coupled electrode treatment tip.
Photographs courtesy of Solta.
In the early clinical experience, one of the main drawbacks to the ThermaCool® procedure was a high degree of discomfort during the procedure, requiring heavy sedation or frank anesthesia. The protocol at that time was to perform 1–2 passes at higher energies. The treatments were quite painful, results tended to be inconsistent from patient to patient, and some adverse events such as fat necrosis and atrophic scarring were noted. Over the years, treatment protocols have evolved to a paradigm utilizing lower energies, multiple passes, and patient feedback on heat sensation as the end point of therapy. This has all but eliminated the risk of unacceptable side effects and has greatly reduced the pain involved such that most procedures can be performed without any anesthesia. Monopolar radiofrequency energy is now commonly used to accomplish skin tightening of the face, eyelids (Case study 1), abdomen (Fig. 9.3), and extremities.
The clinical results of non-ablative radiofrequency skin tightening were first reported by Fitzpatrick and colleagues for the periorbital area in 2003. At least some degree of clinical improvement was reported in 80% of subjects (Figs 9.4–9.6) In 2006, Dover and colleagues compared the original single-pass, high-energy technique with the updated low-energy, multiple-pass technique using immediate tissue tightening as a real-time end point. With the original treatment algorithm, 26% of patients saw immediate tightening, 54% observed skin tightening at 6 months, and 45% found the procedure overly painful. With the updated protocol, 87% had immediate tissue tightening, 92% had some degree of tightening at 6 months, only 5% found the procedure overly painful, and 94% stated the procedure matched their expectations (Figs 9.7, 9.8). The low-energy, multiple-pass protocol has also been reported to be significantly safer, lowering the incidence of adverse events to less than 0.05%.


Figure 9.8 Facial skin tightening following Thermage® treatment: (A) baseline, and (B) 4 months post-treatment.
Photographs courtesy of Solta Medical Aesthetic Center.
Combined electrical and optical energy
The technology has been used in hair removal, wrinkle reduction, skin tightening, and the treatment of both pigment and vascular disorders (Case study 2). The premise is that less radiofrequency energy is ultimately needed for proper collagen denaturation and remodeling. The major disadvantage to these devices is that bipolar radiofrequency energy does not penetrate very deep into the skin. There is also some criticism that bipolar radiofrequency is unable to produce a uniform, volumetric heating response comparable to monopolar radiofrequency. Furthermore, because the bipolar radiofrequency devices are often combined with other light-based technologies, it is difficult to assess exactly how large a role bipolar radiofrequency plays in the clinical outcomes of such treatments.
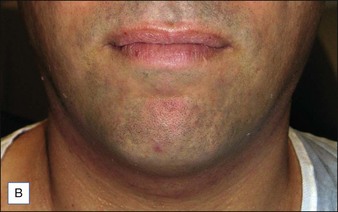
A 54-year-old male presents to your office and states that he has been recently divorced and wants to improve his appearance so that he feels more comfortable re-entering the dating scene. He states he is against injectable treatments such as botulinum toxin or fillers because he does not want to put what he calls ‘foreign substances’ in his body and he does not want to have to come into the office for repeated maintenance. On examination, he has fair skin with scattered lentigines on the cheeks and forehead and fine telangiectasias over the cheeks and nose creating a blush-type erythema. He has early changes consistent with skin laxity predominantly in the mid-face region, brow, and jawline. Combined electrical and optical energy may be the best option for patients who wish to treat their skin laxity in combination with other signs of photodamage such as lentigines or telangiectasias. A 2002 study by Bitter evaluating a series of 3–5 combined intense pulsed light and radiofrequency energy treatments on photoaged skin revealed a 70% improvement in erythema and telangiectasia, a 78% improvement in lentigines, and a 60% improvement in skin texture as determined by subject satisfaction levels. Because these devices can also be used for hair removal, caution should be used in treating the lower face and neck in a male patient so as not to thin or remove the beard. This patient is fair skinned; however, prudence should also be used when treating darker skin types or tanned skin with devices utilizing an optical component absorbed by pigment. As a general guideline, optical fluences should be lowered by a minimum of 20% when treating darkly pigmented lesions or dense pigment irregularity, even in light-skinned patients, to avoid side effects such as burns, crusting or pigmentary alteration.
In 2005, Doshi & Alster conducted one of the first studies using combined diode and radiofrequency technology with a series of three treatments in 20 female subjects (RF: 50–85 J/cm2, optical energy: 32–40 J/cm2). Energy was increased with each session based on the patient’s pain tolerance and a clinical response of immediate erythema and edema. Modest improvement was seen in all patients at 3 months; however, improvement was found to be slightly reduced at 6 months. In 2005, Sadick and colleagues conducted a two-center study using combination intense pulsed light and radiofrequency (RF: up to 20 J/cm2, optical energy: 30–45 J/cm2) over five treatments for facial rhytides and skin laxity. Modest improvements were reported. Side effects were minimal, but some instances of scarring and crusting occurred. In 2007, Yu and colleagues used combination radiofrequency and infrared energy to study skin tightening in a series of three treatments on 19 female Asian patients (RF: 70–120 J/cm2, optical energy: 10 J/cm2). Objective assessment showed mild to moderate improvement in 26–47% of areas treated (Figs 9.9, 9.10).


Figure 9.9 Periorbital rejuvenation: (A) before, and (B) after three treatments with the Galaxy® device.
Hybrid monopolar and bipolar radiofrequency
The first system to combine monopolar and bipolar radiofrequency in one device was the Accent® (Alma Lasers, Buffalo Grove, IL). The theory behind using both types of radiofrequency is to deliver different depths of current to the skin. The bipolar electrode handpiece allows for more superficial, localized (non-volumetric) heating based on tissue resistance to the radiofrequency conductive current. The monopolar electrode handpiece targets deeper, volumetric heating via the rotational movement of water molecules in the alternating current of the electromagnetic field. The monopolar handpiece delivers a higher amount of energy since it theoretically is heating a greater tissue volume than the bipolar handpiece. Typically the monopolar handpiece is used to treat the forehead, cheeks, jawline, and neck (Fig. 9.11). The bipolar handpiece is used to treat the glabella, lateral periorbital area (Fig. 9.12), upper lip and chin, and leg (Fig. 9.13). Despite the use of monopolar radiofrequency, this particular system uses a closed system where no grounding plate is required (Case study 3).

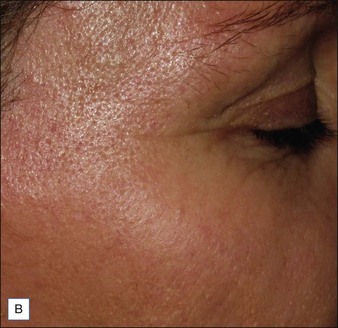
Figure 9.12 Periorbital rejuvenation: (A) before, and (B) 3 months after four treatments with the Accent® treatment.
Photographs courtesy of Dr Alexiades-Armenakas.
Infrared light devices
In 2006, Ruiz-Esparza performed one to three treatments on 25 patients utilizing broadband infrared light from 1100 to 1800 nm. Most patients showed improvement ranging from minimal to excellent with immediate skin tightening visible in 22 of the 25 patients. Three patients showed no improvement. The best results were achieved when using a combination of lower fluences and a high number of pulses. Patients treated at 30 J/cm2 expressed no pain during the procedure and had a high degree of satisfaction immediately post-procedure. The same year, Zelickson and colleagues looked at ultrastructural changes in cadaver and human skin post-treatment. Collagen fibril alteration was found to be highest with greater fluences and depths of 1–2 mm. Marginal results were observed at shallower depths and lower fluences, which were possibly due to the effect of contact cooling. Comparison of the two studies emphasizes that clinical skin tightening does not always correlate with immediate positive histological findings. This is explained by the fact that full clinical effect may take weeks or months to be demonstrated owing to a secondary wound healing response.
Complications were limited to minor erythema, but a few blisters were observed in areas that were overtreated. In 2007, Goldberg and colleagues noted positive results in 11 of 12 patients receiving two treatments with the same device (30–36 J/cm2). The best results were observed in patients who had loose draping skin, with less significant results in sagging skin that was firmly associated with the subcutaneous tissue. No improvement was noted in the jowl region.
Other laser wavelengths that have been used for tissue tightening include the 1064 nm and 1320 nm wavelengths. The chromophores for the 1064 nm wavelength, in decreasing order, are melanin, hemoglobin and water, and the primary chromophore for the 1320 nm wavelength is water. A 2005 study by Taylor & Prokopenko compared a single treatment using a monopolar radiofrequency system (73.5 J/cm2) with a single treatment using the 1064 nm neodymium : yttrium-aluminum-garnet (Nd : YAG) laser (50 J/cm2). The 1064 nm laser side was deemed to have better overall results in terms of improvement in wrinkles and skin laxity, although only modest improvements was noted in both modalities. Another study in 2007 by Key compared a single facial treatment with a monopolar radiofrequency system (40 J/cm2) to the 1064 nm Nd : YAG laser (73–79 J/cm2). The 1064 nm laser resulted in greater improvement on the lower face, while improvement on the upper face was equivalent with both modalities. In 2001, Trelles and colleagues treated 10 patients with a series of eight treatments using a 1320 nm laser system (30–35 J/cm2). Clinical improvement was subtle, with only two patients reporting satisfaction with the procedure. The authors suggested combining laser treatment with parallel epidermal treatment may yield better results and achieve higher patient satisfaction.
Ultrasound devices
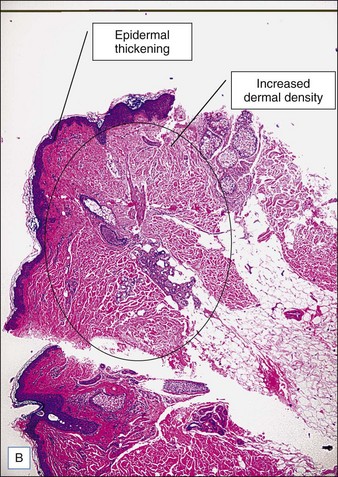
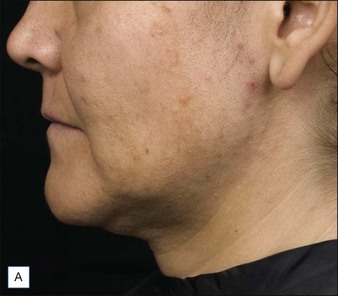
Current protocols aim for a geometric focal depth of therapy in the mid to deep dermis. One of the first clinical trials by Alam and colleagues in 2010 assessed the safety and efficacy of intense focused ultrasound on skin tightening. Significant improvement was seen in brow elevation in more than 83% of treated patients with an average increase in brow elevation of 1.7–1.9 mm (Fig. 9.14). Results developed over a 90-day period following treatment and were still noticeable at 10-month follow-up. The authors found lower face tightening more difficult to assess due to a lack of fixed anatomical landmarks. In 2011, Suh and colleagues treated 22 Asian patients with facial skin laxity with intense focused ultrasound; 77% of patients reported much improvement in the nasolabial folds, and 73% reported much improvement in the jaw line. Histological evaluation of skin samples showed greater dermal collagen with thickening of the dermis and straightening of elastic fibers in the reticular dermis after treatment (Figs 9.15 and 9.16).
Tips for maximizing patient satisfaction
Patient selection is of utmost importance in ultimate satisfaction with non-surgical skin-tightening technologies. Patients must be counseled that maximum results are slow and occur over a period of 3–6 months. In terms of expectations, these technologies should not be thought of as an equivalent technology to surgical lifting, but as an alternative option for a certain subset of patients. Despite a number of clinical studies reporting significant improvement in the appearance of lax skin, most patients show only mild improvement. It appears that patients who are younger with a lesser degree of skin laxity may yield the most promising clinical outcomes; skin laxity without a significant muscular attachment also appears to yield better results (Case study 4). Very elderly patients with severe sagging and wrinkles are, in general, suboptimal candidates for the degree of improvement expected with non-invasive tightening devices (Case study 5).
A 78-year-old woman presents for a consult regarding general photoaging. She has avoided sun exposure her whole life and is a devoted wearer of sunscreen. She tells you she has been going to an esthetician for the past 15 years who gives her light glycolic peels every few months. She has also used a prescription tretinoin cream given to her by her general dermatologist for the past 25 years. She is otherwise healthy and would like to improve her appearance, but she would like to get your advice on what she needs. She has never had surgery before and tells you she would like to avoid having a facelift if possible. On examination she has remarkably preserved skin quality with very few deep lines and no major pigmentary issues owing to her diligent sun protection and long-term use of topical rejuvenation therapies. She does have some loss of definition along the jawline, with mild to moderate jowling, deepening of the nasolabial folds, descent of the eyebrow, and volume-related changes in the mid-face region. She also has prominent platysmal banding visible in the neck region. This patient would be an ideal candidate for almost any of the non-invasive skin-tightening approaches in combination with other therapies such as neurotoxins and fillers to augment her results. Although studies have shown that younger patients tend to have better results than older patients after tissue tightening procedures, this patient has extremely good skin quality and can be expected to have at least some degree of improvement. Because the skin-tightening procedure will not address her underlying changes in facial volume and musculature, performing adjunctive therapies such as botulinum toxin to the superior-lateral orbicularis oculi and platysma muscles would help her lift the brow, decrease banding on the neck, and achieve a more defined jawline. Filler to her mid-face region, nasolabial folds, pre-jowl region, and jawline would also be of use to restore underlying structure, increase the lifting effect, and give a more youthful shape to the face. A 2006 study by Shumaker and colleagues showed monopolar radiofrequency skin tightening to be safe when performed over multiple soft tissue fillers and indicated it may even have some synergistic effects in terms of long-term collagen growth. The patient has proven she is not averse to maintenance therapies and she will achieve a better overall result with global rejuvenation.
Patients should be told that non-ablative skin tightening is not a substitute for a facelift and that results may be modest (Box 9.6). A small number of patients perceive no improvement at all. Patients should also be counseled that non-ablative skin tightening alone is not effective for the textural aspects of photoaging including wrinkles and pigmentary alterations. Long-term studies to examine the longevity of skin tightening have not been performed, but it appears patients can expect at least a period of a year or more before touch-up treatments are required. More research also needs to be done comparing the devices themselves to determine precise advantages of one over another.
Alam M, White L, Martin N, et al. Ultrasound tightening of facial and neck skin: A rater-blinded prospective cohort study. Journal of the American Academy of Dermatology. 2010;62:262–269.
Alexiades-Armenakas M, Rosenberg D, Renton B, et al. Blinded, randomized, quantitative grading comparison of minimally invasive, fractional radiofrequency and surgical face-lift to treat skin laxity. Archives of Dermatology. 2010;146:396–405.
Atiyeh BS, Dibo SA. Nonsurgical nonablative treatment of aging skin: radiofrequency technologies between aggressive marketing and evidence-based efficacy. Aesthetic Plastic Surgery. 2009;33:283–294.
Biesman BS, Pope K. Monopolar radiofrequency treatment of the eyelids: a safety evaluation. Dermatologic Surgery. 2007;33:794–801.
Bitter P, Jr., Mulholland RS. Report of a new technique for enhanced non-invasive skin rejuvenation using a dual mode pulsed light and radiofrequency energy source: selective radiothermolysis. Journal of Cosmetic Dermatology. 2002;1:142–145.
Doshi SN, Alster TS. Combined diode laser and RF energy for rhytides and skin laxity: investigation of a novel device. Journal of Cosmetic and Laser Therapy. 2005;7:11–15.
Dover JS, Zelickson B, and the 14-Physician multispecialty consensus panel. Results of a survey of 5,700 patient monopolar radiofrequency facial skin tightening treatments: assessment of a low-energy multiple-pass technique leading to a clinical end point algorithm. Dermatologic Surgery. 2007;33:900–907.
Fitzpatrick R, Geronemus R, Goldberg D, et al. Multicenter study of noninvasive radiofrequency for periorbital tissue tightening. Lasers in Surgery and Medicine. 2003;33:232–242.
Friedman DJ, Gilead LT. The use of hybrid radiofrequency device for the treatment of rhytides and lax skin. Dermatologic Surgery. 2007;33:543–551.
Gold MH. Update on tissue tightening. Journal of Clinical and Aesthetic. Dermatology. 2010;3:36–41.
Gold MH, Goldman MP, Rao J, et al. Treatment of wrinkles and elastosis using vacuum-assisted bipolar radiofrequency heating of the dermis. Dermatologic Surgery. 2007;33:300–309.
Goldberg DJ, Hussain M, Fazeli A, et al. Treatment of skin laxity of the lower face and neck in older individuals with a broad-spectrum infrared light device. Journal of Cosmetic and Laser Therapy. 2007;9:35–40.
Hantash BM, Renton B, Berkowitz RL, et al. Pilot clinical study of a novel minimally invasive bipolar microneedle radiofrequency device. Lasers in Surgery and Medicine. 2009;41:87–95.
Hsu TS, Kaminer MS. The use of nonablative radiofrequency technology to tighten the lower face and neck. Seminars in Cutaneous Medicine and Surgery. 2003;22:115–123.
Key DJ. Single-treatment skin tightening by RF and long-pulsed, 1064-nm Nd : YAG laser compared. Lasers in Surgery and Medicine. 2007;2:169–175.
Laubach HJ, Makin IR, Barthe PG, et al. Intense focused ultrasound: evaluation of a new treatment modality for precise microcoagulation within the skin. Dermatologic Surgery. 2008;34:727–734.
Mayoral FA. Skin tightening with a combined unipolar and bipolar radiofrequency device. Journal of Drugs in Dermatology. 2007;6:212–215.
Narins RS, Tope WD, Pope K, et al. Overtreatment effects associated with a radiofrequency tissue-tightening device: rare, preventable, and correctable with subcision and autologous fat transfer. Dermatologic Surgery. 2006;32:115–124.
Ruiz-Esparza J. Painless, nonablative, immediate skin contraction induced by low-fluence irradiation with new infrared device: a report of 25 patients. Dermatologic Surgery. 2006;32:60–610.
Sadick NS, Alexiades-Armenakas M, Bitter P, Jr., et al. Enhanced full-face skin rejuvenation using synchronous intense pulsed optical and conducted bipolar RF energy (ELOS): Introducing selective radiophotothermolysis. Journal of the European Academy of Dermatology and Venereology. 2005;4:181–186.
Sadick NS, Shaoul J. Hair removal using a combination of conducted radiofrequency and optical energies – an 18-month follow-up. Journal of Cosmetic and Laser Therapy. 2004;6:21–26.
Shumaker PR, England LJ, Dover JS, et al. Effect of monopolar radiofrequency treatment over soft-tissue fillers in an animal model: Part 2. Lasers in Surgery and Medicine. 2006;38:211–217.
Suh DH, Shin MK, Lee SJ, et al. Intense focused ultrasound tightening in Asian skin: clinical and pathologic results. Dermatologic Surgery. 2011;37(11):1595–1602.
Taub AF, Battle EF, Jr., Nikolaidis G. Multicenter clinical perspectives on a broadband infrared light device for skin tightening. Journal of Drugs in Dermatology. 2006;5(8):771–778.
Taylor MB, Prokopenko I. Split-face comparison of RF versus long-pulse Nd:YAG treatment of facial laxity. Journal of Cosmetic and Laser Therapy. 2006;8:17–22.
Trelles MA, Allones I, Luna R. Facial rejuvenation with a nonablative 1320-nm Nd:YAG laser: a preliminary clinical and histologic evaluation. Dermatologic Surgery. 2001;27:111–116.
Yu CS, Yeung CK, Shek SY, et al. Combined infrared light and bipolar RF for skin tightening in Asians. Lasers in Surgery and Medicine. 2007;39:471–475.
Zelickson B, Ross V, Kist D, et al. Ultrastructural effects of an infrared handpiece on forehead and abdominal skin. Dermatologic Surgery. 2006;32:897–901.