8 Non-surgical body contouring
Summary and Key Features
• Given the epidemic rise of obesity, and the obsession with losing weight and improving our appearance, the treatment of fat and cellulite is a common cosmetic issue
• Fat and cellulite are distinct entities. Cellulite is best considered a hormonally based structural phenomenon of adipocytes and fibrous septae, whereas excess fat is an overabundance of normal adipocytes
• The treatment options for excess fat and cellulite are different and a treatment that improves one may have no discernible impact on the other
• Non-invasive body contouring is a rapidly expanding cosmetic field, with many new technologies recently developed and promising new technologies expected in the near future
• Topical agents, such as retinoids and methylxanthines, have theoretical benefits on the appearance of fat and cellulite, though objective clinical improvements are limited
• Injectable therapies, including mesotherapy and injection lipolysis, are also options for patients
• Physical massage of the affected areas may improve the appearance of fat and cellulite by modulating blood and lymphatic flow. In clinical studies, modest improvements have been observed
• Radiofrequency (RF) devices utilize alternating current to generate ionic flow and localized heat in adipocytes, moderately improving the appearance of fat and cellulite
• High-intensity focused ultrasound (HIFU) can also specifically target adipocytes, thereby improving the appearance and thickness of the fat layer. Recently, a HIFU device was cleared by the FDA for non-invasive waist circumference reduction
• Several laser devices utilizing near-infrared wavelengths, in combination with physical manipulation, have been developed to improve the appearance of fat and cellulite by stimulating dermal collagen formation. Lasers with wavelengths that are selectively absorbed by the adipocytes themselves are currently being developed and studied for potential efficacy
• Cryolipolysis is a novel therapy by which controlled cold exposure (heat extraction) is utilized to selectively damage adipocytes, cause apoptosis, and gradually improve the appearance and thickness of the fat layer over several months following the treatment
• There are few head-to-head studies comparing these different technologies. The ideal treatment option for your patient is best determined by discussing the options with the patient, their ultimate treatment goals, and reaching an informed decision together
Fat versus cellulite
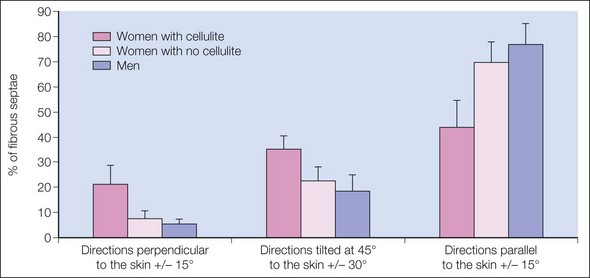
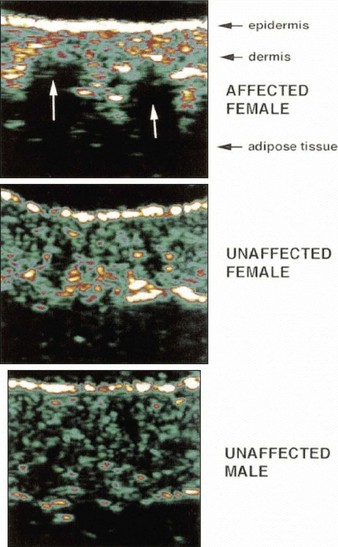
Ultrasound and magnetic resonance imaging (MRI) studies have demonstrated the significant structural alterations between male adipose tissue and female cellulite structure. In male adipose tissue, the fibrous septae of the adipose tissue are arranged in an overlapping criss-cross pattern. This theoretically provides greater strength to the overall scaffolding of the adipose tissue and prevents herniation of fat cells. Cellulite, on the other hand, has fibrous septae that are arranged parallel to each other, and perpendicular to the skin surface (Fig. 8.1). This structure is weaker, and allows for the focal herniation of adipose tissue. It is this focal herniation that is thought to cause the classic undulating, lumpy, ‘cottage cheese’ appearance of cellulite. MRI has demonstrated that women with cellulite do in fact have fibrous septae that are oriented in parallel to each other, although these septae may actually be more similar to pillar-like columns (Figs 8.2 and 8.3). In addition to this structural difference, MRI, ultrasound, and biopsies have also demonstrated that women with cellulite typically have an undulating, lumpy interface between the adipose tissue and the dermis, known as papillae adiposae (Fig. 8.4). This interface also likely contributes to the appearance of cellulite.
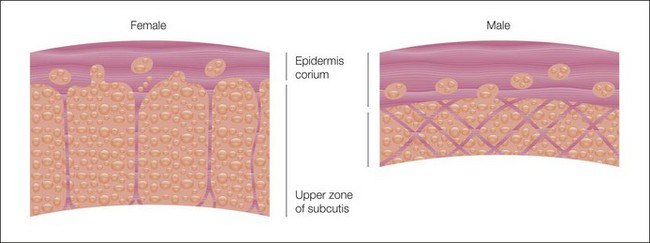
Figure 8.1 Orientation of subcutaneous fibers extending from dermis to fascia in males and females.
Reprinted by permission of Blackwell from Nurnberger F, Muller G 1978 So-called cellulite: An invented disease. Journal of Dermatologic Surgery and Oncology 4:221.
Evaluation of fatty tissue and cellulite
Cellulite can similarly be assessed with various measurements and definitions. Typically, direct observation with side lighting is the simplest and most effective assessment. Based upon these observations, a relatively simple scoring system for the appearance of cellulite has been described (Table 8.1).
| Grade I | No or minimal skin irregularity upon standing, pinch test, or muscle contraction |
| Grade II | No or minimal skin irregularity upon standing. Dimpling becomes apparent by pinching or muscle contraction |
| Grade III | Classic skin dimpling at rest with palpable, small subcutaneous nodularities |
| Grade IV | More severe puckering and nodularity |
Therapeutic options
Topical creams
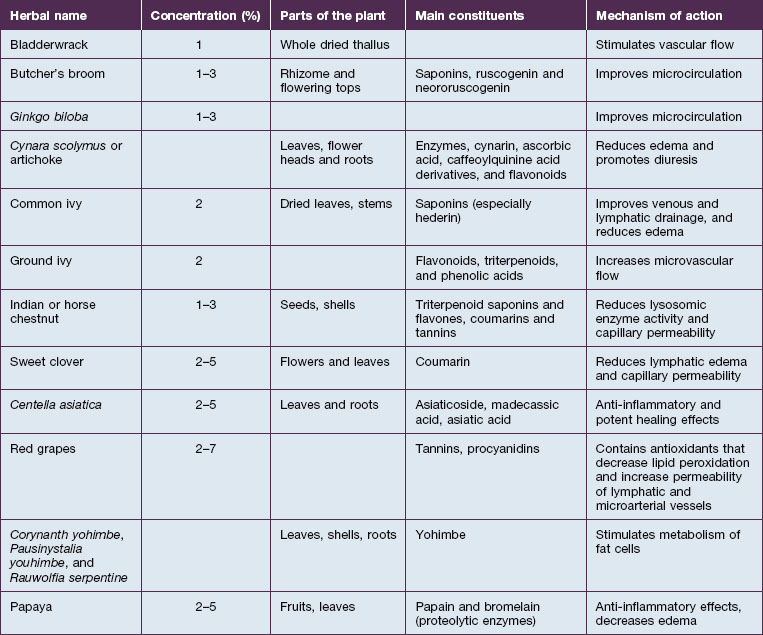
Numerous herbal therapies have also been reported to be effective in treating fat and cellulite (Table 8.2). Many of these herbal supplements have not undergone rigorous testing to determine their efficacy, and their clinical utility remains to be fully elucidated.
Radiofrequency devices
The VelaSmooth® and VelaShape® (Syneron Medical Ltd, Irvine, CA) devices combine physical manipulation (massage and suction), with bipolar RF energy and infrared light (700–2000 nm) to treat excess fat and cellulite. It has been proposed that these devices improve fat and cellulite by heating the subcutaneous tissue and fat, thereby causing increased localized blood flow and lipolysis. In a randomized clinical study by Nootheti et al, comparing the VelaSmooth® device with another laser device for cellulite (TriActive®, Cynosure Inc., Westford, MA), patients were treated twice weekly for 6 weeks. Following the treatments, patients were observed to have an improvement in the upper and lower thigh circumference, as well as in the appearance of cellulite (Figs 8.5 and 8.6). Seventy-five percent of patients were observed to have an improvement, when comparing pre- and post-treatment photographs, but the results were modest. There were no statistically significant differences in the efficacies of the two devices. Bruising can occur following treatment with the VelaSmooth® device, and was more common with this device than the Triactive® device (Fig. 8.7).

Figure 8.5 A 47-year-old woman (A) before, and (B) after six treatments with the VelaShape® device.
Photos courtesy of Neil S. Sadick, MD. Reprinted with permission from Sadick NS 2010 VelaSmooth and VelaShape. In Goldman MP, Hexsel D (eds) Cellulite: pathophysiology and treatment, 2nd edn. Informa Healthcare, New York, NY, p 108-114.

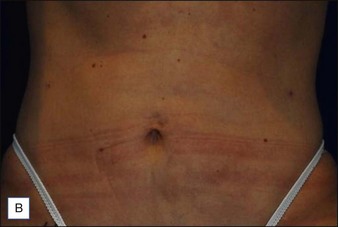
Figure 8.6 A 37-year-old woman (A) before, and (B) after seven treatments with the VelaShape® device.
Photographs courtesy of Neil S. Sadick, MD. Reprinted with permission from Sadick NS 2010 VelaSmooth and VelaShape. In Goldman MP, Hexsel D (eds) Cellulite: Pathophysiology and Treatment, 2nd edn. Informa Healthcare, New York, NY, p 108-114.


Figure 8.7 Purpura after treatment with (A) Triactive® and (B) Velasmooth®.
Reproduced with permission from: Nootheti PK, Magpantay A, Yosowitz G, Calderon S, Goldman MP 2006 A single center, randomized, comparative, prospective clinical study to determine the efficacy of the Velasmooth system versus the Triactive system for the treatment of cellulite. Lasers in Surgery and Medicine 38:908-912.
Lasers and light sources
The TriActive® device (Cynosure Inc., Bedford, MA) combines deep tissue massage and suction (similar to Endermologie®), with contact cooling and a low-intensity diode laser (808 nm). The device purports to increase lymphatic drainage, improve blood flow, and simultaneously tighten skin in the treated areas, which is thought to improve the appearance of cellulite. Patients typically are treated with the device twice weekly, with a progressive improvement following the treatments. In clinical studies, patients were noted to achieve improvement in the appearance of cellulite, as well as objective improvement in hip and thigh circumferences. Subjective improvement included reduction in the appearance of skin dimpling, improvement in the overall contour of the limb, and improvement in overall skin texture (Fig. 8.8). The treatments were well tolerated, although many patients (~20%) developed mild bruising.


Figure 8.8 Cellulite treatment with Triactive®: subject (A) before, and (B) following 10 treatments.
Reproduced with permission from: Boyce S, Pabby A, Chuchaltkaren P, Brazzini B, Goldman MP 2005 Clinical evaluation of a device for the treatment of cellulite: Triactive. American Journal of Cosmetic Surgery 22:233-237.
Cryolipolysis
This patient’s BMI is 23.4, which is within the normal range. She does have localized pockets of excess adipose tissue below the umbilicus, without substantial skin redundancy. This patient could be a good candidate for localized, tumescent liposuction, if she desired. However, she states she does not want an invasive procedure. After discussing options, she elects to have the area treated with CoolSculpting®. The proposed treatment area is marked (a separate, but representative patient is shown in Fig. 8.9A). Due to the size, two applications in the same treatment session will be necessary to treat the complete area, each marked with an X (Fig. 8.9B). A pinch test is performed to insure that the area can be effectively elevated in the device (Fig. 8.9C). The patient undergoes treatment with no adverse effects.
It is important to remind the patient that the full effect of the treatment will not be visible for 2–3 months. In the post-procedure photo, taken 16 weeks after the patient’s single cryolipolysis treatment session, a noticeable reduction in the volume and appearance of the abdominal fat ‘muffin top’ is clearly observable (Fig. 8.9D, E).
Avram MM. Cellulite: a review of its physiology and treatment. Journal of Cosmetic and Laser Therapy. 2004;6:181–185.
Collis N, Elliot LA, Sharpe C, et al. Cellulite treatment: a myth or reality: a prospective randomized, controlled trial of two therapies, endermologie and aminophylline cream. Plastic and Reconstructive Surgery. 1999;104(4):1110–1114.
Dover J, Burns J, Coleman S, et al. A prospective clinical study of noninvasive cryolypolysis for subcutaneous fat layer reduction – Interim report of available subject data. Presented at the Annual Meeting of the American Society for Laser Medicine and Surgery, April 2009, National Harbor, MD 2009.
Goldberg DJ, Fazeli A, Berlin AL. Clinical, laboratory and MRI analysis of cellulite treatment with a unipolar radiofrequency device. Dermatologic Surgery. 2008;34(2):204–209.
Güleç AT. Treatment of cellulite with LPG endermologie. International Journal of Dermatology. 2009;48:265–270.
Hamilton EC, Greenway FL, Bray GA. Regional fat loss from the thigh in women using 2% aminophylline. Obesity Research. 1993;1:95S.
Hexsel DM, Mazzuco R. Subcision: a treatment for cellulite. International Journal of Dermatology. 2000;39:539–544.
Jewell ML, Baxter RA, Cox SE, et al. Randomized sham-controlled trial to evaluate the safety and effectiveness of a high-intensity focused ultrasound device for noninvasive body sculpting. Plastic and Reconstructive Surgery. 2011;128(1):253–262.
Klein KB, Zelickson B, Riopelle JG, et al. Non-invasive cryolipolysis for subcutaneous fat reduction does not affect serum lipid levels or liver function tests. Lasers in Surgery and Medicine. 2009;41(10):785–790.
Kligman AM, Pagnoni A, Stoudemayer T. Topical retinol improves cellulite. Journal of Dermatologic Treatment. 1999;10:119–125.
Kulick MI. Evaluation of a noninvasive, dual-wavelength laser-suction and massage device for the regional treatment of cellulite. Plastic and Reconstructive Surgery. 2010;125(6):1788–1796.
Lach R. Reduction of subcutaneous fat and improvement in cellulite appearance by dual-wavelength, low-level laser energy combined with vacuum and massage. Journal of Cosmetic and Laser Therapy. 2008;10(4):202–209.
Manstein D, Laubach H, Watanabe K, et al. Selective cryolysis: a novel method of non-invasive fat removal. Lasers in Surgery and Medicine. 2008;40(9):595–604.
Mirrashed F, Sharp JC, Krause V, et al. Pilot study of dermal and subcutaneous fat structures by MRI in individuals who differ in gender, BMI, and cellulite grading. Skin Research and Technology. 2004;10:161–168.
Nootheti PK, Magpantay A, Yosowitz G, et al. A single center, randomized, comparative, prospective clinical study to determine the efficacy of the Velasmooth system versus the Triactive system for the treatment of cellulite. Lasers in Surgery and Medicine. 2006;38(10):908–912.
Nurnberger F, Muller G. So-called cellulite: an invented disease. Journal of Dermatologic Surgery and Oncology. 1978;4:221–229.
Pierard-Franchiemont C, Pierand GE, Henry F, et al. A randomized, placebo controlled trial of topical retinal in the treatment of cellulite. American Journal of Clinical Dermatology. 2000;1(6):369–374.
Querleux B, Cornillon C, Jolivet O. Anatomy and physiology of subcutaneous adipose tissue by in vivo magnetic resonance imaging and spectroscopy: relationships with sex and presence of cellulite. Skin Research and Technology. 2002;8:118–124.
Rosales-Berber IA, Diliz-Perez E. Controlled cooling of subcutaneous fat for body reshaping. Presented at the 15th World Congress of the International Confederation for Plastic, Reconstructive and Aesthetic Surgery, New Delhi, India, 2009.
Rossi ABR, Vergnanini AL. Cellulite: a review. Journal of the European Academy of Dermatology and Venereology. 2000;14:251–262.
Rotunda AM, Avram MM, Avram AS. Cellulite: Is there a role for injectables? Journal of Cosmetic and Laser Therapy. 2005;7:147–154.
Teitelbaum SA, Burns JL, Kubota J, et al. Noninvasive body contouring by focused ultrasound: safety and efficacy of the Contour I device in a multicenter, controlled, clinical study. Plastic and Reconstructive Surgery. 2007;120(3):779–789.