CHAPTER 17 No Vertical Scar Breast Reduction and Mastopexy
Summary
The ‘no vertical scar’ reduction/mastopexy is another tool which is useful to correct the large or sagging breast with a lot of ptosis. This technique can produce a pleasing breast shape and a nice areola without the areolar distortion or the visibility of a vertical scar.1–3
Key Points
Patient Selection
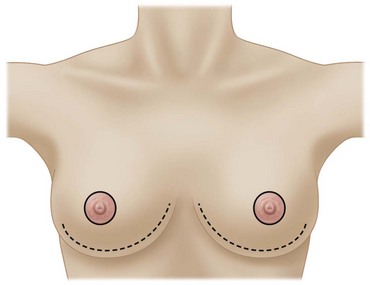
The ‘no vertical scar’ reduction/mastopexy is essentially the same reliable operation as the T scar inferior pedicle reduction except that it has one less scar: the vertical scar (see Figs 17.1–17.3). The most common cause of patient dissatisfaction after breast reduction is the scar.4 We believe that many patients can get the same nice breast shape achieved with the T scar without a vertical scar. If we can achieve good shape with one less scar than is achieved with a T scar reduction, then why not do it?
This is a good technique for a patient that has a lot of ptosis and a lot of excess skin. The ideal patient is one who has 5 or more cm of skin between the areola and the new areolar site (see Fig. 17.4).
Indications
The vertical scar reduction has the least amount of skin removal of the three techniques. We therefore prefer the medial pedicle vertical reduction/mastopexy5 for the patient who does not have very much skin to excise, and who does not have a great deal of ptosis (less than 5 cm of skin between the areola and the new areolar site). This is about 25% of the patients in our practice.
The ‘no vertical scar’ technique can be used for either reduction or mastopexy.1–3
The medial pedicle rotation advancement vertical scar operation (rotation of the medial pedicle superiorly and advancement of the lateral pillar beneath it) may give more projection than the T scar or ‘no vertical scar’ techniques. However breast shaping sutures do augment the projection obtained with the ‘no vertical scar’ and the T scar techniques.1
Operative Technique
The Plastic Surgery Video Archive has an excellent film showing preoperative markings and intraoperative technique.6
Preoperative preparation
Markings
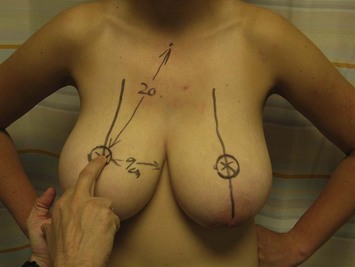
A line is drawn down the center of the breast meridian line where the areola will look best (see Fig. 17.4). If a large part of the lateral breast is to be removed, the nipple–areola axis line can be moved medially as will be appropriate to the final anticipated breast width. The axis of the breast is drawn as a continued straight line below the inframammary fold by keeping it as a straight line seen through two fingers holding up the breast mound (see Fig. 17.5).
A finger on the breast is used to palpate another finger through the breast at the level of the inframammary fold, and this becomes the new nipple site (Fig. 17.4). The areolar recipient site skin excision is marked on the skin brassiere preoperatively with the patient sitting. It is drawn as a slightly horizontal oval (3.5 cm diameter horizontally, and 3.0 cm diameter vertically) as the oval will stretch to a circle when the skin brassiere flap is pulled down over the breast to the inframammary fold at the time of final closure. The areola is marked as a 4 cm diameter circle also with the patient sitting up. The area of the areolar recipient circle is deliberately marked to be a little smaller than the areola itself in order to achieve a tension free closure in the periareolar scar. The areolar recipient site is also marked smaller than the areola itself when the author uses the T scar or the vertical scar techniques.
A tension free areolar scar means a better appearing areolar scar. This scar is the most visible scar of the reduced breast (see Fig. 17.6). The areolar scar is the scar that the woman sees every day when she is naked. It is the showcase scar of the breast and should be treated as we treat the preauricular scar of the facelift; tension free and closed with care.

Fig. 17.6 Postoperatively ‘no vertical scar’ breast reduction with typical pleasing periareolar scar. The areolar opening is designed to have a slightly smaller diameter than the areola to avoid tension. There is no distortion of the inferior periareolar scar by a vertical scar, and no vertical scar on the visible breast mound. The inframammary scar is hidden in the inframammary fold below the breast mound. This is the same patient seen in Figure 17.14.
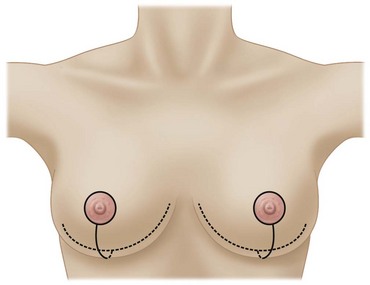
To avoid visible medial dog ears in the no vertical and T scar techniques, the medial end of the inframammary fold incision is marked to be hidden under the medial fold of the breast so that it will not be visible postoperatively (see Fig. 17.7). The lateral end of the inframammary fold incision is drawn 1 cm medial to its preoperative position because the smaller postoperative breast inframammary fold has moved medially. If the patient is overweight and has a lateral chest fat fold, the lateral scar should be kept in this fat fold crease to decrease its visibility.
After the marking of the inframammary fold incision, the lower incision of the skin brassiere flap is marked on the breast mound. The center of this incision is marked at 5–6 cm below the lower border of the areola recipient site. Nice smooth curves are then drawn from this point medially to reach the medial inframammary fold incision mark (see Fig. 17.8), and then laterally to reach the lateral inframammary incision mark.
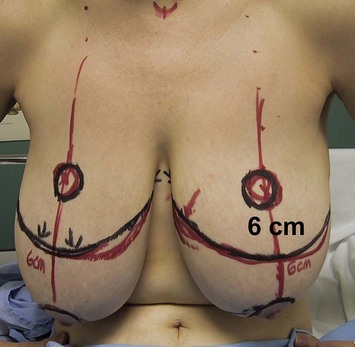
Fig. 17.8 The ideal patient has at least 5 cm of normal skin between the new areolar site and the existing areola. Notice the nice smooth curve of the black mark for the proposed inferior border of the skin brassiere flap. The red mark below it on the right medial breast would have given a boxy breast (see Figure 17.18). The medial end of the marked inframammary incision should be hidden under the medial breast mound.
Technique
Skin brassiere flap elevation
The tourniquet is released and a 1.5–2.0 cm skin brassiere flap is elevated off of the entire breast mound down to the loose areolar tissue of the chest wall (see Fig. 17.9). The lateral part of the skin flap can be made thinner (1.0 cm thick) to avoid lateral breast bulging. This lateral part of the skin brassiere flap will no longer be covering breast after surgery. Instead, it will be covering the lateral chest wall as lateral breast will either be removed in reductions or replaced from this lateral position and tacked to the chest wall medially in mastopexies.
The brassiere skin flap dissection is performed with a large #23 blade and carried over the whole breast so that the entire breast mound is skinned (see Fig. 17.10). This is particularly easy in a younger glandular breast where pressure is maintained on the back of the moving buried scalpel blade, constantly feeling it pressing against the gland so the sharp edge is cutting between the gland/subdermal fat junction. Large swooping cuts with the blade in this fashion make this part of the operation rapid.
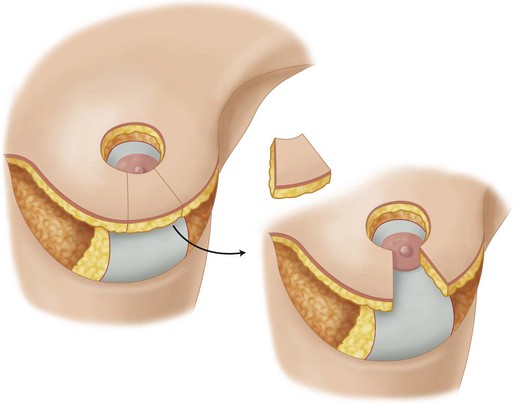
The skin brassiere flap should not be thinner than 1.5 cm in the bipedicled part below the new areolar hole in order to preserve the blood supply to that skin and fat. The areolar hole in the skin brassiere flap is made with the scalpel aimed obliquely upward (superiorly) to avoid the fat and blood supply below the areolar hole (see Fig. 17.11). There are always significant bleeders at about 10 mm in depth which provide a robust blood supply to the skin brassiere flap. We have only lost a little (<2 cm2) skin below the areolar hole on two occasions in the first year we used this technique because we thinned the bipedicled flap below the areolar hole too aggressively. This skin loss was still less than what we sometimes lost in the area of T zone necrosis in the first 15 years of the authors’ practice in which we exclusively used the T scar reduction.
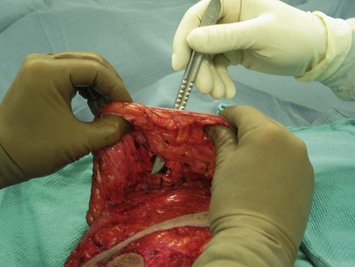
Gland excision
After the gland excision, intraoperative breast sizers (ASSI Instruments, http://www.healthforumbuyersguide.com/company.php?id=308&company=ASSI-Accurate+Surgical) are used to help further resection for final volume adjustment to ensure that the volume of the remaining breast and skin tissue is the same on both sides before the skin is closed (see Fig. 17.12). We find this technique more accurate than trying to measure breast volume with our hands.

Fig. 17.12 The entire breast pedicle and skin flap brassiere are placed in the see-through stainless steel breast sizer, which has the closest volume to the breast being measured. The same procedure is carried out on both sides to make sure that the two breasts have the same volume before the skin is closed. Breast sizers supplied by ASSI Instruments (http://www.healthforumbuyersguide.com/company.php?id=308&company=ASSI-Accurate+Surgical). Declaration of conflict of interest – D.L. is a consultant for ASSI Instruments.
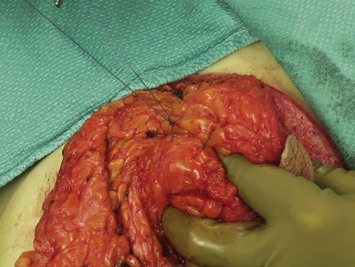
Breast shaping sutures
Breast shaping sutures can be used with any kind of breast reduction, including the T scar and the no vertical scar reductions. We use breast shaping sutures for both no vertical scar mastopexy and reduction cases. We use 3-0 Monocryl (Ethicon, Piscataway, NJ, USA) sutures to suture the breast gland to itself to increase projection and get a pleasing shape (Figs 17.13 and 17.14). We then suture the breast to the chest wall superomedially to get it out from under the dependent lateral empty skin brassiere flap pocket until that space heals closed.
We use our fingers to shape the breast to achieve both projection and lateral concavity. Breast shaping sutures should not be tied too tightly to strangle the breast, nerves and blood vessels inside of the suture loop (Fig. 17.13). We therefore tie solid knots over large loose loops of breast tissue designed to just bring the breast tissue together in a kissing fashion.
Pitfalls and How to Correct
Armpit breast deformity (lateral bulge)
The lateral bulge deformity (see Fig. 17.15) can be avoided by thinning out the skin brassiere flap and the chest wall laterally, by aggressively excising lateral breast tissue, and by suturing the breast mound superomedially until the lateral skin brassiere flap heals to the lateral chest wall. It can be corrected by secondary lateral tissue removal either directly through the inframammary incision or by liposuction under local anesthesia.
Medial and lateral dog ears/visible incisions
These can be avoided by drawing the incisions as in Figure 17.9 so they end up hidden in the inframammary crease when the patient is sitting or standing after wound healing occurs. Visible scars cannot be removed, only revised. Dog ears can be defatted or excised under local anesthesia (see Figs 17.15 and 17.17 for lateral and medial dog ears).
Boxy shape
This can be avoided by drawing the inframammary incisions as smooth curves (see Fig. 17.16). This can be corrected with skin and/or fat excision under local anesthesia as a secondary procedure.
Inframammary fold wound dehiscence
This can be avoided by careful closure of the inframammary incision with care to make sure epidermal/dermal contact occurs on both sides of the wound throughout its entire length. If it occurs (see Fig. 17.18), the wounds are usually clean and can be resutured secondarily under local anesthesia taking large 1 cm bites of 3-0 Nylon that will not rip through the skin.
Possible skin loss of the bipedicled part of the skin brassiere flap below the areola
This can be avoided by: (1) aiming the scalpel blade obliquely upward (superiorly) when making the areolar recipient site cut in the skin brassiere flap in order to preserve the blood supply to the skin and fat below the areolar hole (see Fig. 17.11); and (2) by keeping the skin brassiere flap thicker than 1.5 cm below the areolar recipient hole. If skin loss does occur, allow secondary healing as you would with T zone necrosis in the T scar reduction.
1 Chun YS, Lalonde DH, May JWJr. Internal pedicle shaping to improve aesthetic results in reduction mammaplasty. Plast Reconstr Surg. 2007;119:1183.
2 Lalonde DH, Lalonde J, French R. The no vertical scar breast reduction: a minor variation that allows you to remove vertical scar portion of the inferior pedicle wise pattern T scar. Aesth Plast Surg. 2003;27(5):335.
3 Lalonde DH, French RJ, Lalonde J. The no vertical scar breast reduction: how to delete the vertical scar of the standard T-scar breast reduction and produce an excellent breast shape. Perspect Plast Surg. 2001;15(2):103.
4 Celebiler O, Sönmez A, Erdim M, et al. Patients’ and surgeons’ perspectives on the scar components after inferior pedicle breast reduction surgery. Plast Reconstr Surg. 2005;116:459.
5 Hall-Findlay EJ. Vertical breast reduction with a medially based pedicle. Operative strategies. Aesth Surg J. 2002;22(2):185-195.
6 Video of marking and surgery. http://www.mediafire.com/download.php?3jyzummt2nw.
Hosnuter M, Tosun Z, Kargi E, et al. No-vertical-scar technique versus inverted T-scar technique in reduction mammoplasty: a two-center comparative study. Aesth Plast Surg. 2005;29:496.
Movassaghi K, Liao E, Morris D, Orgill D, Pribaz J. Eliminating the vertical scar in breast reduction. The Boston modification of the Robertson technique. Aesth Plast Surg. 2006;26:687.
Nagy MW, McCraw JB, Lalonde DH, et al. The no vertical scar mammaplasty: a durable approach to a complex problem. Plast Reconstr Surg. 2005;116(3 Suppl):216. 75