Neuroradiology
Ordinary X-rays show only the bony structures, giving no direct information about the nervous system itself for which X-ray computerized tomography (CT) or magnetic resonance imaging (MRI) are required. MRI is the best technique for imaging most central nervous system (CNS) pathology of both the brain and spinal cord.
Contrast media may be used to enhance diagnosis of CT and MRI scans, particularly highlighting defects in the blood–brain barrier (BBB). While different agents are used in each (iodine-based preparation for CT, gadolinium for MRI), the principle is the same. They are injected into a vein, usually in the arm, and become concentrated in vascular structures or where the BBB is disrupted, making these areas appear brighter. For example, a tumour is vascular with an impaired BBB and will therefore enhance, while the centre of the tumour is necrotic with no circulation and will not enhance, giving a characteristic pattern of ‘ring enhancement’ with contrast on the scan (Fig. 1).
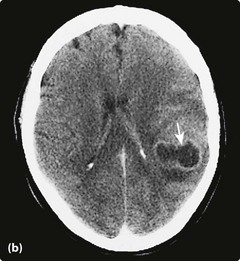
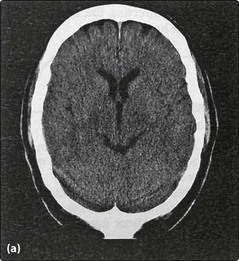
Computerized axial tomography
CT scan is the most commonly available form of neuroimaging in the UK (Fig. 2a). The patient lies with the head in a ring which contains both X-ray emission and detection apparatus. Images are formed in slices, as the head is moved through the ring. The dose of X-rays is relatively large and CT is contraindicated in pregnancy except in emergencies. CT scan remains the method of choice, however, for the demonstration of acute intracranial haemorrhage and intracranial calcification. CT is relatively insensitive at detecting pathology of the spinal cord but can detect most herniated lumbar intervertebral discs and is useful in delineating bony abnormalities. Modern CT can be used to examine arterial and venous structures and provides a non-invasive high-quality alternative to conventional angiography.
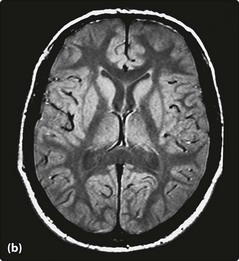
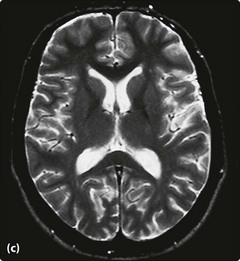
Magnetic resonance imaging
There are two commonly performed types of scan:
 T2 – water is bright and pathological tissue is often highlighted, but with some loss of anatomical resolution (Fig. 2c).
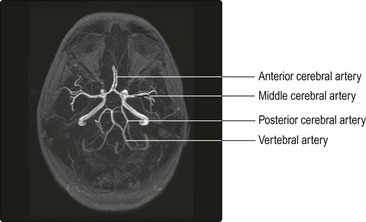
T2 – water is bright and pathological tissue is often highlighted, but with some loss of anatomical resolution (Fig. 2c).MRI parameters may be set to detect blood flow and MRI may be used as another non-invasive form of angiography (MRA; Fig. 3) of both arterial and venous circulations. MRI can be tailored so that tissues alter appearance according to scan parameters (e.g. suppressing signal from fat), and it is the combination of appearances on different types of scans that leads to the diagnosis.
Special MRI sequences may be used for particular purposes. Diffusion-weighted imaging (DWI) is very useful in identifying distinguishing acute infarction from other pathologies (Fig. 2, p. 69) and gradient-echo imaging highlights haemosiderin deposition from previous haemorrhage.
Angiography
This is still the ‘gold standard’ test for imaging blood vessels intracranially and in the neck (Fig. 4). Advances in MRA or CT angiography may replace this technique for diagnostic purposes in the future. A cannula is inserted into the femoral artery under local anaesthetic, manoeuvred into the aortic arch and into the carotid or vertebral arteries. Contrast is injected and X-rays are taken. Delayed X-rays allow visualization of the venous system. The examination is relatively safe, major complications such as stroke occurring in <0.5%. Transient neurological deficits due to vasospasm are seen occasionally. Bruising may occur at the site of arterial puncture and bleeding is occasionally severe. Most units monitor pulse and blood pressure very closely for several hours after angiography.
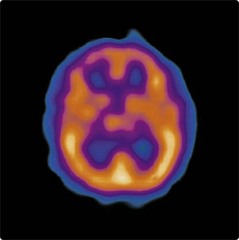
Functional neuroimaging
A variety of techniques are becoming available to explore regional cerebral function. These are generally research techniques. The most widely available is single photon emission computed tomography (SPECT) (Fig. 5). This utilizes radioactive isotopes whose distribution mirrors cerebral perfusion. Regional uptake of these isotopes is determined by CT detection of radioactive decay emissions. This has very limited temporal and spatial resolution.