Neurophysiological investigations
The electroencephalogram
Method
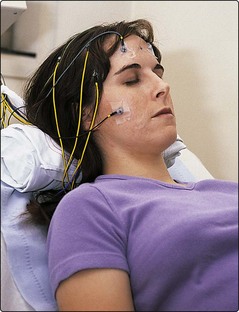
The patient rests back and 20 electrodes are attached over the scalp with glue (Fig. 1). These are connected to a multichannel recorder, which generates a paper tracing or a computer record. This is often synchronized with a video recording of the patient. A skilled technician monitors the recording throughout, to detect and eliminate artefacts. The EEG is recorded with the patient’s eyes open and closed and several methods may be used to enhance sensitivity of the technique, routinely including forced hyperventilation for 3 min and stroboscopic photic stimulation at 1–50 Hz. Another technique to increase sensitivity is to deprive the patient of sleep before the EEG, then allow the patient to fall asleep during the recording.
EEG interpretation
Paroxysmal interictal EEG changes
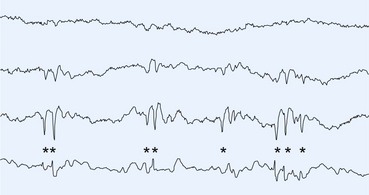
Spikes and sharp waves may be focal (affecting only part of the brain) or generalized (simultaneously affecting all parts of the brain) (Figs 2 and 3). Focal spikes suggest epilepsy due to a focal disturbance and imply a focal structural cause; neuroimaging should be considered. Generalized spikes are seen as part of the generalized epilepsies, which usually start in childhood or adolescence (pp. 74–75). The EEG shows normal background rhythms with frequent paroxysmal spike discharges. Photic stimulation triggers the discharges in about 5% of patients with primary generalized epilepsy (PGE) but rarely in other forms of epilepsy. Other generalized patterns may be seen in children with an abnormal background EEG who have a poorer prognosis and are associated with mental retardation or structural pathology such as tuberose sclerosis.
Important non-epileptic EEG patterns
| Herpes simplex encephalitis | Very regular sharp wave (e.g. 1 Hz) activity over one or both temporal regions with underlying slow activity called periodic lateralized epileptiform discharges (PLEDs) |
| Metabolic encephalopathy | Generalized slow activity. Triphasic waves typically seen in hepatic encephalopathy |
| Creutzfeldt–Jakob disease (CJD) | Widespread rhythmic triphasic waves at 0.5–2 Hz, often associated with near-simultaneous myoclonic jerks (may be absent in new variant CJD) |
Evoked potential studies
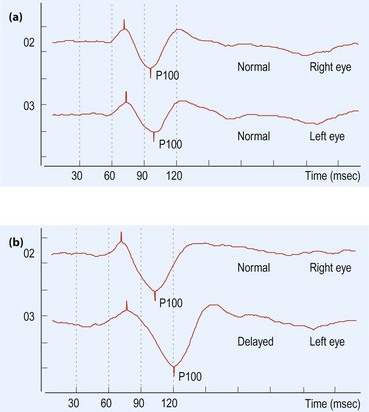
Evoked potential studies are a method of testing the integrity of sensory pathways from end-organ to cerebral cortex. They are useful in identifying subclinical sites of nervous system involvement, providing evidence of multiple lesions in CNS demyelination. The optic nerve is a particularly common site of subclinical involvement in multiple sclerosis (MS) and the visual-evoked potential (VEP) is generally the most useful test (Fig. 4). VEPs give a relatively poor indication of the site of disease along the sensory pathway and they have become less important in the diagnosis of MS since the advent of MRI scanning. Indications for evoked potentials are summarized in Table 2.
| Investigation | Possible indications |
|---|---|
| Visual-evoked potentials | Monocular visual loss, optic nerve disease, multiple sclerosis |
| Auditory-evoked potentials | Unilateral hearing loss, multiple sclerosis |
| Somatosensory-evoked potentials | Spinal cord lesions, radiculopathy, multiple sclerosis |