Neurology and psychiatry
A primary psychiatric diagnosis is present in 13–27% of new neurology outpatients and evidence of psychiatric morbidity in up to 48%.
Introduction
 Psychiatric illness may present with neurological symptoms. Examples are depression presenting as pseudodementia (p. 55) and non-organic neurological illness (p. 116).
Psychiatric illness may present with neurological symptoms. Examples are depression presenting as pseudodementia (p. 55) and non-organic neurological illness (p. 116).Psychiatric complications of neurological disease
Obsessive-compulsive disorder
This is also seen in movement, especially Parkinson’s disease and Huntington’s disease.
Complications of epilepsy
Neurological diseases presenting with psychiatric manifestations
The diagnosis of a primary psychiatric illness requires that the symptoms occur in normal consciousness. The presence of altered consciousness or periods of drowsiness suggest a neurological cause (pp. 50, 52). There may, however, be no obvious clouding of consciousness in the early stages and other factors may be helpful in making the diagnosis (Table 1).
Table 1 Comparison of organic brain syndromes and psychiatric disease
| Symptom | Organic disease | Psychiatric disease |
|---|---|---|
| Clouding of consciousness | Common | Rare |
| Seizures | Common | Rare |
| Memory | Impaired | Often preserved |
| Visual hallucinations | Commonly without auditory hallucinations | Rare without auditory hallucinations |
| Tactile hallucinations | Commonly without auditory hallucinations | Rare without auditory hallucinations |
| Focal neurological signs | Sometimes | Rare |
| Disturbed sleep | Reversal of sleep cycle | Insomnia |
| Paranoia | Common | Common |
| Feelings of control | Rare | Sometimes |
| Headache | Sometimes | Sometimes |
Auditory hallucinations are common in psychiatric disease and may be accompanied by hallucinations in other modalities, but in organic disease these commonly occur without auditory hallucinations. Visual hallucinations most commonly occur in acute confusional states, where they are often complex (pink elephants in delirium tremens). They may also occur with lesions at any level of the visual system from the eyes to the association cortex, when they may be flashes of light or complex images and may be restricted to an abnormal visual field. Brief, stereotyped images may represent partial seizures but are also seen by normal individuals when falling off to sleep (hypnagogic hallucinations) and, rarely, in brain stem lesions (peduncular hallucinosis). Cortical Lewy body disease causes dementia with visual hallucinations in up to 85% of cases and Parkinson’s disease causes nightmares and similar hallucinations when treated with high doses of levodopa. Olfactory, gustatory and somatosensory (crawling ants on the skin) hallucinations also occur in acute organic brain syndromes and in epilepsy (p. 74).
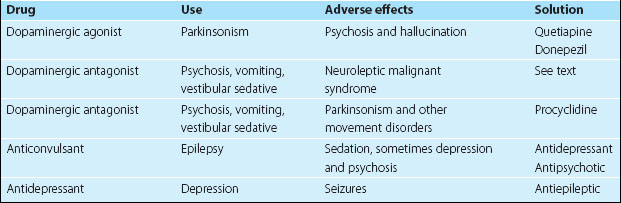
Neurological and psychotropic medication
Drugs used in the treatment of psychiatric illness often have neurological side effects and vice versa. Withdrawal of the culprit may not be possible; Table 2 lists some alternative strategies.
Neuropsychiatric complications of drugs of abuse
Drug dependence is a psychiatric disorder, with organic components, physical dependence and tolerance, psychological components and psychological dependence. Most drugs are associated with both neurological and psychiatric complications (Table 3).
| Drug | Neurological complications | Psychiatric complications |
|---|---|---|
| Alcohol | Intoxication, stupor and coma, Wernicke’s encephalopathy, Korsakoff syndrome, seizures, delirium tremens, myopathy, neuropathy, cerebellar syndrome | Acute and chronic auditory hallucinosis, personality disintegration, morbid jealousy |
| Amfetamine | Organic hallucinosis, NMS-type syndrome, cerebral vasculitis | Chronic psychosis |
| MDMA (ecstasy) | Organic hallucinosis, NMS-type syndrome, destruction of serotonergic fibres | Not yet established |
| Cocaine | Organic hallucinosis, stroke (common), subarachnoid and cerebral haemorrhage | Depression, mania, phobic disorders, anxiety disorders |
| Lysergic acid (LSD) | Organic hallucinosis | Chronic psychosis, hallucinatory flashbacks |
NMS, neuroleptic malignant syndrome