2. Key Areas Determining Sensory Level
3. Key Muscles Determining Motor Level
4. Grading of Muscle Strength
5. Grading of Deep Tendon Reflexes
6. Testing of Cranial Nerves
B. Epilepsy
1. Partial (Focal Epilepsy)
Etiology
 Temporal lobe epilepsy (most common form epilepsy in adults) manifests as a complex partial seizure.
Temporal lobe epilepsy (most common form epilepsy in adults) manifests as a complex partial seizure. Frequent causes of partial seizures are tumor, stroke, CNS infections (cysticercosis, abscesses), AVMs, traumatic brain injury, cortical malformations, and idiopathic/genetic conditions.
Frequent causes of partial seizures are tumor, stroke, CNS infections (cysticercosis, abscesses), AVMs, traumatic brain injury, cortical malformations, and idiopathic/genetic conditions.Diagnosis
 EEG
EEG Ambulatory EEG and/or video EEG if diagnostic uncertainty
Ambulatory EEG and/or video EEG if diagnostic uncertaintyH&P
 Usually physical/neurologic exam is nl unless the cause is structural abnlity (stroke), wherein neuro exam is consistent with the area of CNS structural damage.
Usually physical/neurologic exam is nl unless the cause is structural abnlity (stroke), wherein neuro exam is consistent with the area of CNS structural damage. During partial seizures pts are conscious, unless there is spread of the epileptic focus causing secondary generalization and unresponsiveness. A focal seizure can evolve to a generalized tonic clonic seizure. Table 10-4 describes clinical manifestations of different types of focal seizures and areas of the brain involved.
During partial seizures pts are conscious, unless there is spread of the epileptic focus causing secondary generalization and unresponsiveness. A focal seizure can evolve to a generalized tonic clonic seizure. Table 10-4 describes clinical manifestations of different types of focal seizures and areas of the brain involved.Imaging
 Head CT to r/o space-occupying lesions. If possible, avoid in children unless an emergency.
Head CT to r/o space-occupying lesions. If possible, avoid in children unless an emergency. Brain MRI with defined epilepsy protocol should be performed if recurrent seizures.
Brain MRI with defined epilepsy protocol should be performed if recurrent seizures.Treatment
 First unprovoked seizure with nl imaging/EEG/labs generally requires no Rx; recurrent or abnl w/up requires Rx with compliance; avoidance of EtOH and sleep deprivation is essential to prevent recurrence.
First unprovoked seizure with nl imaging/EEG/labs generally requires no Rx; recurrent or abnl w/up requires Rx with compliance; avoidance of EtOH and sleep deprivation is essential to prevent recurrence. No driving is allowed until seizure freedom in accordance w/local laws/regulations (47% seizure free w/monoRx, 67% w/polyRx).
No driving is allowed until seizure freedom in accordance w/local laws/regulations (47% seizure free w/monoRx, 67% w/polyRx). Avoid valproic acid (↑ risk teratogenicity) in women of childbearing age and regardless of antiepileptic drug taken; begin folic acid (1-4 mg/day) to prevent neural tube defects.
Avoid valproic acid (↑ risk teratogenicity) in women of childbearing age and regardless of antiepileptic drug taken; begin folic acid (1-4 mg/day) to prevent neural tube defects. Carbamazepine is the traditional initial drug for partial seizures.
Carbamazepine is the traditional initial drug for partial seizures.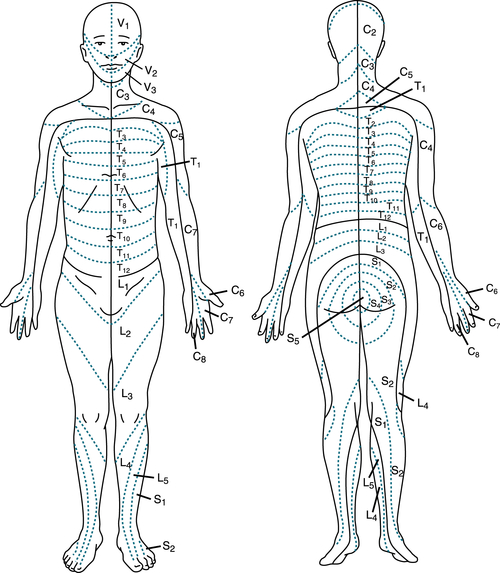
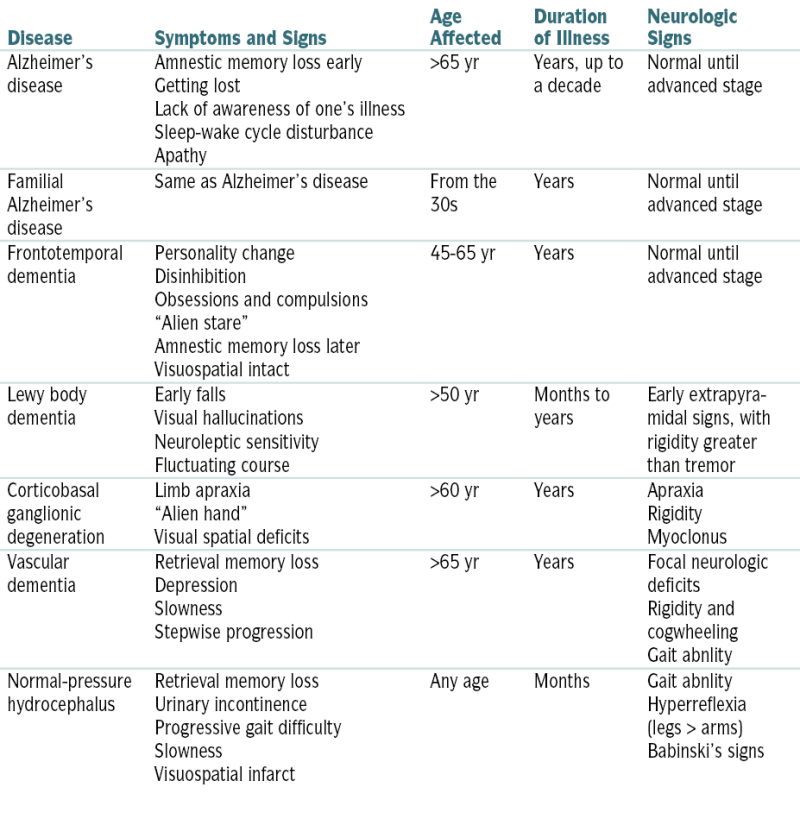
FIGURE 10-1 Spinal dermatomes. (From Green GM [ed]: The Harriet Lane Handbook: A Manual for Pediatric House Officers, 12th ed. St. Louis, Mosby–Year Book, 1991.)
TABLE 10-1
Grading of Muscle Strength
| Grade | Description |
| 0 | Absent muscle contraction |
| 1 | Minimal contraction |
| 2 | Active movement with gravity eliminated |
| 3 | Active movement against gravity only |
| 4 | Active movement against gravity and some resistance |
| 5 | Normal muscle strength |
TABLE 10-2
Grading of Deep Tendon Reflexes
| Grade | Description |
| 0 | Absent |
| + | Hypoactive |
| ++ | Normal |
| +++ | Brisker than average |
| ++++ | Hyperactive, often indicative of disease |
TABLE 10-3
Testing of Cranial Nerves
| Cranial Nerves | Action | |
| I | Olfactory | Sense of smell |
| II | Optic | Vision (visual acuity, visual fields, color) |
| III | Oculomotor | Extraocular movement, pupillary constriction (oculomotor), elevation of upper lids, abduction of eye |
| IV | Trochlear | |
| VI | Abducens | |
| V | Trigeminal | Mastication; sensory of forehead, face, and jaw |
| VII | Facial | Facial expression; taste in anterior two thirds of tongue |
| VIII | Acoustic | Hearing and balance |
| IX | Glossopharyngeal | Sensory and motor functions of pharynx and larynx (gag reflex, position of uvula, swallowing) |
| X | Vagus | |
| XI | Accessory | Shrugging of shoulders, movement of head, motor to trapezius, sternocleidomastoid |
| XII | Hypoglossal | Motor control of tongue |
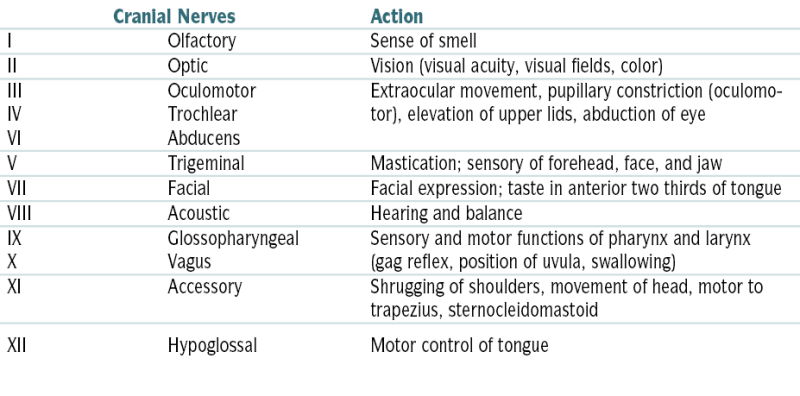
TABLE 10-4
Clinical Manifestations of Different Types of Focal Seizures and Areas of the Brain Involved
| Seizure Type | Areas of Brain Involved | Clinical Expression |
| Somatosensory | Postcentral rolandic; parietal | Contralateral intermittent or prolonged tingling, numbness, sense of movement, desire to move, heat, cold, electric shock; sensation may spread to other body segments |
| Parietal | Contralateral agnosia of a limb, phantom limb, distortion of size or position of body part | |
| Second sensory; supplementary sensory-motor | Ipsilateral or bilateral facial, truncal or limb tingling, numbness, or pain; often involving lips, tongue, fingertips, feet | |
| Motor | Precentral rolandic | Contralateral regional clonic jerking, usually rhythmic, may spread to other body segments in jacksonian motor march; often accompanied by sensory symptoms in same area |
| Supplementary sensory-motor | Bilateral tonic contraction of limbs causing postural changes; may exhibit classic fencing posture; may have speech arrest or vocalization | |
| Frontal | Contralateral head and eye version, salivation, speech arrest or vocalization; may be combined with other motor signs (as above) depending on seizure spread | |
| Auditory | Heschl’s gyrus—auditory cortex in superior temporal lobe | Bilateral or contralateral buzzing, drumming, single tones, muffled sounds |
| Olfactory | Orbitofrontal; mesial temporal cortex | Often described as unpleasant odor |
| Gustatory | Parietal; rolandic operculum; insula; temporal lobe | Often unpleasant taste, acidic, metallic, salty, sweet, smoky |
| Vertiginous | Occipitotemporal-parietal junction; frontal lobe | Sensation of body displacement in various directions |
| Visual | Occipital | Contralateral static, moving, or flashing colored or uncolored lights, shapes, or spots; contralateral or bilateral, partial or complete loss of vision |
| Temporal; occipitotemporal-parietal junction | Formed visual scenes, faces, people, objects, animals | |
| Limbic | Limbic structures: amygdala, hippocampus, cingulum, olfactory cortex, hypothalamus | Autonomic: abdominal rising sensation, nausea, borborygmi, flushing, pallor, piloerection, perspiration, heart rate changes, chest pain, shortness of breath, cephalic sensation, lightheadedness, genital sensation, orgasm Psychic: déjà vu, jamais vu, depersonalization, derealization, dreamlike state, forced memory or forced thinking, fear, elation, sadness, sexual pleasure; hallucinations or illusions of visual, auditory, or olfactory nature |
| Dyscognitive | Usually bilateral involvement of limbic structures (see above) | Previously known as “complex partial seizures,” characterized by a predominant alteration of consciousness or awareness; current definition requires involvement of at least two of five components of cognition: perception, attention, emotion, memory, and executive function |
From Goldman L, Schafer AI (eds): Goldman’s Cecil Medicine, 24th ed. Philadelphia, Saunders, 2012.
| C2 | Occipital protuberance | T6 | Sixth intercostal space, xiphisternum |
| C3 | Supraclavicular fossa | T7-9 | Intercostal spaces |
| C4 | Top of the acromioclavicular joint | T10 | Umbilicus |
| C5 | Lateral side of the antecubital fossa | T11 | Intercostal space |
| C6 | Thumb | T12 | Inguinal ligament |
| C7 | Middle finger | L1 | Upper anterior thigh |
| C8 | Little finger | L2 | Midanterior thigh |
| T1 | Medial side of the antecubital fossa | L3 | Medial femoral condyle |
| T2 | Apex of the axilla | L4 | Medial malleolus |
| T3 | Third intercostal space | L5 | Dorsum of the foot at the third metatarsophalangeal joint |
| T4 | Fourth intercostal space, nipple line | S1 | Lateral heel |
| T5 | Fifth intercostal space | S2 | Popliteal fossa in the midline |
| S3 | Ischial tuberosity | ||
| S4-5 | Perianal area |
| C1-4 | Diaphragm |
| C5 | Elbow flexors (biceps) |
| C6 | Wrist extensors |
| C7 | Elbow extensors (triceps) |
| C8 | Finger flexors, distal phalanx |
| T1 | Hand intrinsics (interossei) |
| T2-L1 | Use sensory level and Beevor’s sign |
| L2 | Hip flexors (iliopsoas) |
| L3 | Knee extensors (quadriceps) |
| L4 | Ankle dorsiflexors (tibialis anterior) |
| L5 | Long toe extensors (extensor hallucis longus) |
| S1 | Ankle plantar flexors (gastrocnemius) |
| S2-5 | Use sensory level and sphincter ani |
 Lamotrigine and levetiracetam are effective and well tolerated.
Lamotrigine and levetiracetam are effective and well tolerated. Antiepileptics (lacosamide, oxcarbazepine, ezogabine) may be used by epilepsy specialists.
Antiepileptics (lacosamide, oxcarbazepine, ezogabine) may be used by epilepsy specialists. Surgery (temporal lobectomy in mesial temporal sclerosis) may be indicated in refractory cases.
Surgery (temporal lobectomy in mesial temporal sclerosis) may be indicated in refractory cases.2. Idiopathic General Epilepsy
Diagnosis
 EEG
EEG Ambulatory EEG and/or video EEG if diagnostic uncertainty
Ambulatory EEG and/or video EEG if diagnostic uncertaintyTABLE 10-5
Generalized Seizures: Classification and Clinical Expression
| Seizure Type | Subtype | Clinical Expression |
| Absence | Typical | Abrupt cessation of activities, with motionless, blank stare and loss of awareness lasting ≈10 sec; the attack ends suddenly, and pt resumes normal activities immediately |
| Atypical | Longer duration than typical absence, often accompanied by myoclonic, tonic, atonic, and autonomic features as well as automatisms | |
| With myoclonias | Absence with myoclonic components of variable intensity | |
| Myoclonic | Myoclonic | Sudden, brief (<100 msec), shocklike, involuntary, single or multiple contractions of muscle groups of various locations |
| Myoclonic-atonic | A sequence consisting of a myoclonic followed by an atonic phase | |
| Myoclonic-tonic | A sequence consisting of a myoclonic followed by a tonic phase | |
| Tonic | Sustained increase in muscle contraction lasting a few seconds to minutes | |
| Clonic | Prolonged, regularly repetitive contractions involving the same muscle groups at a rate of 2-3 cycles/sec | |
| Atonic | Sudden loss or diminution of muscle tone lasting 1-2 sec, involving head, trunk, jaw, or limb musculature | |
| Tonic-clonic | A sequence consisting of a tonic followed by a clonic phase |
From Goldman L, Schafer AI (eds): Goldman’s Cecil Medicine, 24th ed. Philadelphia, Saunders, 2012.
Labs
 Routine blood w/up (CBC, CMP, glucose, electrolytes), urine tox screen
Routine blood w/up (CBC, CMP, glucose, electrolytes), urine tox screen LP recommended if suspicion of meningitis
LP recommended if suspicion of meningitisImaging
 Head CT scan r/o space-occupying lesions; avoid in children unless a neurologic emergency
Head CT scan r/o space-occupying lesions; avoid in children unless a neurologic emergency MRI of the brain epilepsy protocol performed in all pts with recurrent seizures
MRI of the brain epilepsy protocol performed in all pts with recurrent seizuresTreatment
 First unprovoked seizure with nl imaging/EEG/laboratory w/up requires no Rx; recurrent seizures or pts w/abnl w/up require Rx based on type/etiology.
First unprovoked seizure with nl imaging/EEG/laboratory w/up requires no Rx; recurrent seizures or pts w/abnl w/up require Rx based on type/etiology. Chronic Rx is indicated for more than two unprovoked seizures or in pts with one seizure with abnl w/up.
Chronic Rx is indicated for more than two unprovoked seizures or in pts with one seizure with abnl w/up. Levetiracetam (initial dose 250-500 mg bid, max 1500 mg bid) is an effective and well-tolerated antiepileptic drug for generalized tonic clonic seizures.
Levetiracetam (initial dose 250-500 mg bid, max 1500 mg bid) is an effective and well-tolerated antiepileptic drug for generalized tonic clonic seizures. Valproic acid (initial dose 10-15 mg/kg/day div bid, max dose 60 mg/kg/day) is better tolerated than topiramate and more efficacious than lamotrigine in pts w/generalized and unclassified epilepsy types; avoid valproic acid (↑ risk teratogenicity) in women of childbearing age and regardless of antiepileptic drug taken; begin folic acid (1-4 mg/day) to prevent neural tube defects.
Valproic acid (initial dose 10-15 mg/kg/day div bid, max dose 60 mg/kg/day) is better tolerated than topiramate and more efficacious than lamotrigine in pts w/generalized and unclassified epilepsy types; avoid valproic acid (↑ risk teratogenicity) in women of childbearing age and regardless of antiepileptic drug taken; begin folic acid (1-4 mg/day) to prevent neural tube defects. No driving is allowed until seizure freedom in accordance with local laws and regulations.
No driving is allowed until seizure freedom in accordance with local laws and regulations.3. Status Epilepticus
Diagnosis
 Convulsive status epilepticus: Pts are unresponsive w/obvious tonic, clonic, or tonic-clonic extremity movements.
Convulsive status epilepticus: Pts are unresponsive w/obvious tonic, clonic, or tonic-clonic extremity movements. Nonconvulsive status epilepticus varies from complete unresponsiveness w/little or no observable motor activity to confusion and/or repetitive behaviors/automatisms; confirm dx by video EEG monitoring or paradoxical improvement in ms after low-dose benzodiazepine.
Nonconvulsive status epilepticus varies from complete unresponsiveness w/little or no observable motor activity to confusion and/or repetitive behaviors/automatisms; confirm dx by video EEG monitoring or paradoxical improvement in ms after low-dose benzodiazepine.Management
C. Stroke
1. Transient Ischemic Attack (TIA)
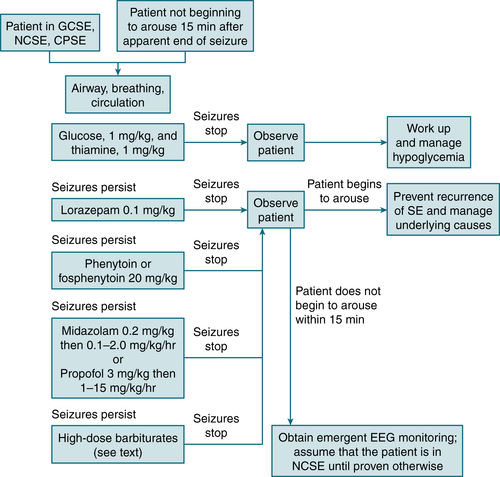
FIGURE 10-2 Management algorithm for status epilepticus. CPSE, complex partial status epilepticus; GSCE, generalized convulsive status epilepticus, NCSE, nonconvulsive status epilepticus; SE, status epilepticus. (From Vincent JL, Abraham E, Moore FA, et al [eds]: Textbook of Critical Care, 6th ed. Philadelphia, Saunders, 2011.)
Etiology
 Cardioembolic
Cardioembolic Large-vessel atherothrombotic disease
Large-vessel atherothrombotic disease Lacunar disease
Lacunar disease Hypoperfusion w/fixed arterial stenosis
Hypoperfusion w/fixed arterial stenosis Hypercoagulable states
Hypercoagulable statesDiagnosis
H&P
Imaging
 Head CT, brain MRI, MRA
Head CT, brain MRI, MRA Carotid Doppler, echo, ECG
Carotid Doppler, echo, ECG Telemetry for hospitalized pts
Telemetry for hospitalized ptsLabs
 CBC w/Plt, PT, PTT
CBC w/Plt, PT, PTT Glucose, lipid profile, ESR
Glucose, lipid profile, ESR CXR; other tests dictated by suspected etiology
CXR; other tests dictated by suspected etiologyTreatment
 Depends on etiology. Table 10-6 describes the characteristics of thrombosis vs embolism. The ABCD2 score can help stratify pts who are at highest risk of subsequent stroke after TIA (Table 10-7). Consider hospital admission for pts with ABCD2 score >3 or those with transient monocular blindness.
Depends on etiology. Table 10-6 describes the characteristics of thrombosis vs embolism. The ABCD2 score can help stratify pts who are at highest risk of subsequent stroke after TIA (Table 10-7). Consider hospital admission for pts with ABCD2 score >3 or those with transient monocular blindness. Acute anticoagulation is indicated for new-onset AF and atherothrombotic carotid disease causing recurrent transient neurologic sx, especially before carotid endarterectomy (CEA) or carotid stenting. It is also considered for basilar artery thrombosis, given concern for progression to brainstem stroke w/high morbidity and mortality.
Acute anticoagulation is indicated for new-onset AF and atherothrombotic carotid disease causing recurrent transient neurologic sx, especially before carotid endarterectomy (CEA) or carotid stenting. It is also considered for basilar artery thrombosis, given concern for progression to brainstem stroke w/high morbidity and mortality. Antiplatelet therapy should be used to reduce the risk of recurrent TIAs or subsequent stroke. Three antiplatelet agents are commonly used in stroke prevention: aspirin, aspirin/dipyridamole, and clopidogrel. All are reasonable choices, but practitioners should consider their individual pt’s comorbidities when selecting an antiplatelet agent.
Antiplatelet therapy should be used to reduce the risk of recurrent TIAs or subsequent stroke. Three antiplatelet agents are commonly used in stroke prevention: aspirin, aspirin/dipyridamole, and clopidogrel. All are reasonable choices, but practitioners should consider their individual pt’s comorbidities when selecting an antiplatelet agent. Chronic therapy should be aimed at modifying the four major risk factors: BP control, control of dyslipidemia, control of blood sugar, and smoking cessation.
Chronic therapy should be aimed at modifying the four major risk factors: BP control, control of dyslipidemia, control of blood sugar, and smoking cessation.TABLE 10-6
Characteristics of Thrombosis and Embolism
| Thrombosis | Embolism | |
| Onset of sx | Progression of sx during hours to days | Very rapid (seconds) |
| Hx of previous TIA | Common | Uncommon |
| Time of presentation | Often during night hours while pt is sleeping Classically, pt awakens w/a slight neurologic deficit that gradually progresses in a stepwise fashion |
Pt is usually awake and involved in some type of activity |
| Predisposing factors | Atherosclerosis, HTN, diabetes, arteritis, vasculitis, hypotension, trauma to head and neck | AF, mitral stenosis and regurgitation, endocarditis, mitral valve prolapse |
TABLE 10-7
ABCD2 Risk of Stroke After a TIA
| Score (points) | |
| Age ≥60 yr | 1 |
| BP: ≥140 mm Hg systolic or 90 mm Hg diastolic | 1 |
| Clinical features Unilateral weakness Speech disturbance without weakness |
2 1 |
| Duration of TIA ≥60 min 10-59 min |
2 1 |
| Presence of diabetes mellitus | 1 |
| Two-day risk of stroke is 4.1% with a score 4-5 and 8.1% with a score 6-7. | |
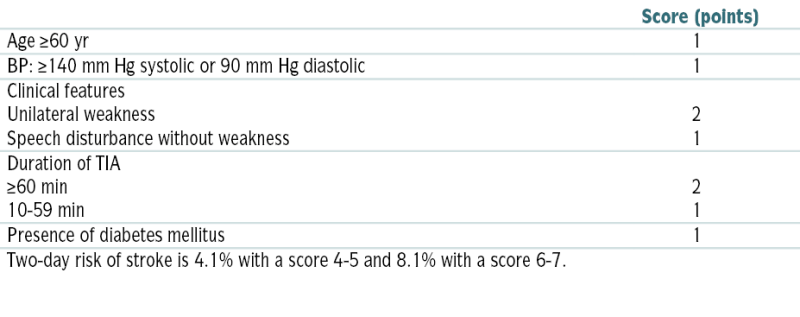
Modified from Ballinger A: Kumar & Clark’s Essentials of Clinical Medicine, 6th ed. Edinburgh, Saunders, 2012.
2. Ischemic Stroke
Diagnosis
H&P
Imaging
 Immediate CT of the head without contrast or MRI of the brain with stroke protocol to rule out hemorrhage and, if possible, to assess the extent of stroke. CT of brain: area of ↓ density; initial CT scan may be nl because the infarct may not be evident for 2 to 3 days afterward.
Immediate CT of the head without contrast or MRI of the brain with stroke protocol to rule out hemorrhage and, if possible, to assess the extent of stroke. CT of brain: area of ↓ density; initial CT scan may be nl because the infarct may not be evident for 2 to 3 days afterward.
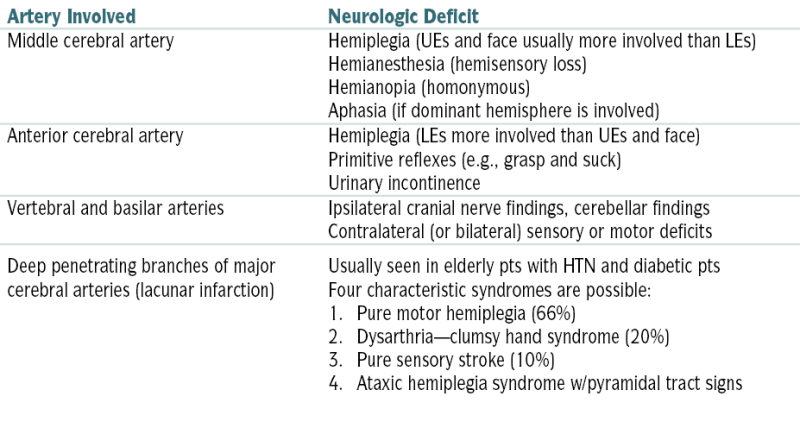
TABLE 10-8
Selected Stroke Syndromes
| Artery Involved | Neurologic Deficit |
| Middle cerebral artery | Hemiplegia (UEs and face usually more involved than LEs) Hemianesthesia (hemisensory loss) Hemianopia (homonymous) Aphasia (if dominant hemisphere is involved) |
| Anterior cerebral artery | Hemiplegia (LEs more involved than UEs and face) Primitive reflexes (e.g., grasp and suck) Urinary incontinence |
| Vertebral and basilar arteries | Ipsilateral cranial nerve findings, cerebellar findings Contralateral (or bilateral) sensory or motor deficits |
| Deep penetrating branches of major cerebral arteries (lacunar infarction) | Usually seen in elderly pts with HTN and diabetic pts Four characteristic syndromes are possible: 1. Pure motor hemiplegia (66%)
2. Dysarthria—clumsy hand syndrome (20%)
3. Pure sensory stroke (10%)
4. Ataxic hemiplegia syndrome w/pyramidal tract signs
|
Treatment
 IV TPA is the only medical therapy approved by the U.S. FDA for the treatment of acute ischemic stroke.
IV TPA is the only medical therapy approved by the U.S. FDA for the treatment of acute ischemic stroke. The time window for administration is ≤3 hr of symptom onset.
The time window for administration is ≤3 hr of symptom onset. The protocol is weight based, with 90 mg being the maximum allowable dose.
The protocol is weight based, with 90 mg being the maximum allowable dose. The risk of brain hemorrhage with IV TPA is ≈5% in pts w/stroke.
The risk of brain hemorrhage with IV TPA is ≈5% in pts w/stroke. Multimodal therapy (i.e., thrombectomy and intra-arterial TPA) is sometimes performed.
Multimodal therapy (i.e., thrombectomy and intra-arterial TPA) is sometimes performed. Endovascular treatment may be performed for select cases in which IV TPA has failed to recanalize an occluded artery.
Endovascular treatment may be performed for select cases in which IV TPA has failed to recanalize an occluded artery. Endovascular intervention may be an option for pts w/systemic contraindications to IV TPA.
Endovascular intervention may be an option for pts w/systemic contraindications to IV TPA. Endovascular intervention is useful only for large, accessible thrombi. Therefore, if a pt w/stroke is a candidate for IV TPA, then he or she should probably receive IV TPA.
Endovascular intervention is useful only for large, accessible thrombi. Therefore, if a pt w/stroke is a candidate for IV TPA, then he or she should probably receive IV TPA. Antiplatelet therapy: Beginning oral or feeding tube administration of aspirin (325 mg/day) ≤48 hours of stroke onset is advised. This will decrease the likelihood of a repeat ischemic stroke. Another oral antiplatelet regimen approved for secondary stroke prophylaxis (e.g., clopidogrel, aspirin plus extended-release dipyridamole) will also suffice and may be superior in the long term.
Antiplatelet therapy: Beginning oral or feeding tube administration of aspirin (325 mg/day) ≤48 hours of stroke onset is advised. This will decrease the likelihood of a repeat ischemic stroke. Another oral antiplatelet regimen approved for secondary stroke prophylaxis (e.g., clopidogrel, aspirin plus extended-release dipyridamole) will also suffice and may be superior in the long term. ↑ BP is common during acute stroke, and it often subsides without specific Rx. In general, HTN is not treated acutely unless it is extremely high (e.g., >220 mm Hg SBP); unless there is evidence of organ damage caused by the HTN; or unless thrombolysis is being considered, in which case BP needs to ↓ (if it can be safely accomplished) to ∼185/110 mm Hg. It is risky to ↓ BP severely the presence of acute ischemic stroke. A 15% to 25% decrease over the first 24 hours is recommended.
↑ BP is common during acute stroke, and it often subsides without specific Rx. In general, HTN is not treated acutely unless it is extremely high (e.g., >220 mm Hg SBP); unless there is evidence of organ damage caused by the HTN; or unless thrombolysis is being considered, in which case BP needs to ↓ (if it can be safely accomplished) to ∼185/110 mm Hg. It is risky to ↓ BP severely the presence of acute ischemic stroke. A 15% to 25% decrease over the first 24 hours is recommended.3. Acute Hemorrhagic Stroke
a. Intracranial hemorrhage
Etiology
 HTN (50%-60%)
HTN (50%-60%) Cerebral amyloid angiopathy (10%)
Cerebral amyloid angiopathy (10%) Hemorrhagic infarcts (10%)
Hemorrhagic infarcts (10%) Use of anticoagulants and fibrinolytic agents (10%)
Use of anticoagulants and fibrinolytic agents (10%) Brain tumors (5%)
Brain tumors (5%) Vascular malformations (5%)
Vascular malformations (5%)Diagnosis
H&P
 Signs of ↑ ICP (e.g., bradycardia, ↓ RR, third nerve palsy)
Signs of ↑ ICP (e.g., bradycardia, ↓ RR, third nerve palsy)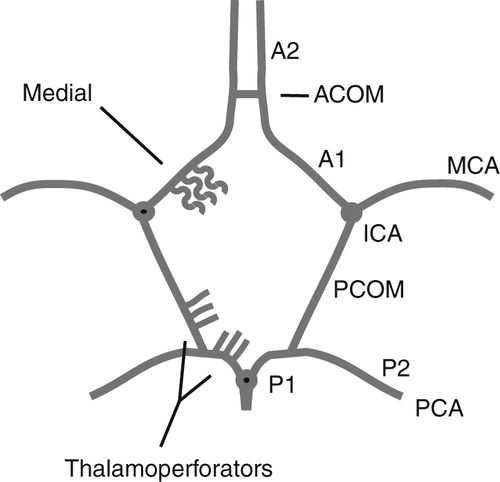
FIGURE 10-3 Circle of Willis. ACOM, anterior communicating artery; MCA, middle cerebral artery; PCA, posterior cerebral artery; PCOM, posterior communicating artery. (From Weissleder R, Wittenberg J, Harisinghani M, Chen JW [eds]: Primer of Diagnostic Imaging, 5th ed. St. Louis, Mosby, 2011.)
Imaging
 Immediate: CT scanning of the head without contrast is highly sensitive for hemorrhage (area of hemorrhagic infarct appears as a zone of ↑ density).
Immediate: CT scanning of the head without contrast is highly sensitive for hemorrhage (area of hemorrhagic infarct appears as a zone of ↑ density). MRI of the brain with a gradient echo sequence is also highly sensitive for hemorrhage, including intracerebral microhemorrhages that may not be visible with CT scanning.
MRI of the brain with a gradient echo sequence is also highly sensitive for hemorrhage, including intracerebral microhemorrhages that may not be visible with CT scanning.Treatment
 Surgery should be performed promptly for cases of cerebellar hemorrhage of >3 cm when the pt is deteriorating clinically or showing brainstem edema or hydrocephalus.
Surgery should be performed promptly for cases of cerebellar hemorrhage of >3 cm when the pt is deteriorating clinically or showing brainstem edema or hydrocephalus. Surgery for lobar or deep brain clots may be considered for select cases, although the level of evidence for efficacy is not high.
Surgery for lobar or deep brain clots may be considered for select cases, although the level of evidence for efficacy is not high. Pneumatic compression devices should be applied to help prevent DVT.
Pneumatic compression devices should be applied to help prevent DVT. Early mobilization for rehabilitation is desirable.
Early mobilization for rehabilitation is desirable.TABLE 10-9
Localizing Signs in Pts w/Intracerebral Hemorrhage
| Location of Intracerebral Hemorrhage | Common Neurologic Signs | Examples |
| Putamen | Both eyes deviating conjugately to the side of the lesion (away from hemiparesis) Pupils normal in size and reacting normally Contralateral hemiplegia present Hemisensory defect noted |
Left putaminal hemorrhage |
| Thalamus | Both eyes deviating downward and looking at the nose Impairment of vertical eye movements present Pupils small (≈2 mm) and nonreactive Contralateral hemisensory loss present |
Thalamic hemorrhage |
| Pons | Both eyes in midposition No doll’s-eye movements Pupils pinpoint but reactive (use magnifying glass) Coma common Flaccid quadriplegia noted |
Pontine hemorrhage |
| Cerebellum | Ipsilateral paresis of conjugate gaze (inability to look toward side of lesion) Pupils normal in size and reacting normally Inability to stand or to walk Vertigo and dysarthria present |
Cerebellar hemorrhage |
 HTN: BP should be quickly lowered by 15% and then gradually and safely brought to the individual pt’s target range. In theory, this may diminish expansion of the hematoma. Recommended guidelines for Rx of HTN in pts w/spontaneous hemorrhage are described in Box 10-6.
HTN: BP should be quickly lowered by 15% and then gradually and safely brought to the individual pt’s target range. In theory, this may diminish expansion of the hematoma. Recommended guidelines for Rx of HTN in pts w/spontaneous hemorrhage are described in Box 10-6. Hyperglycemia: A high blood glucose level predicts a worse outcome. Markedly elevated glucose levels should be lowered to <300 mg/dL.
Hyperglycemia: A high blood glucose level predicts a worse outcome. Markedly elevated glucose levels should be lowered to <300 mg/dL. Seizures: If seizures occur, they should be treated aggressively, including with IV medications, if needed.
Seizures: If seizures occur, they should be treated aggressively, including with IV medications, if needed. ↑ ICP: This condition should be treated with a graded approach, which may include the elevation of the head of the bed, analgesia/sedation, hyperventilation, and osmotic therapy.
↑ ICP: This condition should be treated with a graded approach, which may include the elevation of the head of the bed, analgesia/sedation, hyperventilation, and osmotic therapy. Antipyretics should be administered for cases that involve fever; in addition, the cause of the fever should be sought.
Antipyretics should be administered for cases that involve fever; in addition, the cause of the fever should be sought. Protamine sulfate is used to treat cases of heparin-induced intracerebral hemorrhage.
Protamine sulfate is used to treat cases of heparin-induced intracerebral hemorrhage. Vitamin K is given for warfarin-associated intracerebral hemorrhage. In addition, recombinant factor VIIa and fresh frozen plasma are sometimes used.
Vitamin K is given for warfarin-associated intracerebral hemorrhage. In addition, recombinant factor VIIa and fresh frozen plasma are sometimes used. Recommendations for thrombolytic-associated intracerebral hemorrhage treatment include the consideration of the infusion of Plts and cryoprecipitate.
Recommendations for thrombolytic-associated intracerebral hemorrhage treatment include the consideration of the infusion of Plts and cryoprecipitate.b. Subarachnoid Hemorrhage (SAH)
Diagnosis
H&P
 Abrupt onset of severe occipital or generalized headache that radiates into the posterior neck region and is worsened by neck and head movements; often described as “the worst headache” of the pt’s life
Abrupt onset of severe occipital or generalized headache that radiates into the posterior neck region and is worsened by neck and head movements; often described as “the worst headache” of the pt’s life Restlessness, vomiting, diminished level of consciousness, syncope
Restlessness, vomiting, diminished level of consciousness, syncope Focal neurologic signs usually are absent.
Focal neurologic signs usually are absent. Level of consciousness varies from nl to deeply comatose.
Level of consciousness varies from nl to deeply comatose. Fever and nuchal rigidity are present or usually develop within 24 hr.
Fever and nuchal rigidity are present or usually develop within 24 hr. Fundi may show papilledema or retinal hemorrhage.
Fundi may show papilledema or retinal hemorrhage. Cranial nerve abnlities may be noted (e.g., pupillary dilation secondary to oculomotor nerve dysfunction).
Cranial nerve abnlities may be noted (e.g., pupillary dilation secondary to oculomotor nerve dysfunction). HTN may be present and can lead to an incorrect dx of primary hypertensive emergency.
HTN may be present and can lead to an incorrect dx of primary hypertensive emergency. Tachycardia and irregular heartbeat may be present (≤91% of pts w/SAH have cardiac arrhythmias).
Tachycardia and irregular heartbeat may be present (≤91% of pts w/SAH have cardiac arrhythmias).Imaging and Labs
 CT of brain is (+) in >95% of cases, especially during the acute phase (i.e., 24-48 hr) after the onset of bleeding.
CT of brain is (+) in >95% of cases, especially during the acute phase (i.e., 24-48 hr) after the onset of bleeding. A CT angiogram or a cerebral angiogram is imperative for determining the origin of the SAH. Angiography may also be extremely useful because it may offer a therapeutic benefit via the coiling of the aneurysm.
A CT angiogram or a cerebral angiogram is imperative for determining the origin of the SAH. Angiography may also be extremely useful because it may offer a therapeutic benefit via the coiling of the aneurysm. Basic labs should include CBC, chemistry panel, PT, PTT, Plt count, troponin.
Basic labs should include CBC, chemistry panel, PT, PTT, Plt count, troponin. LP is a very important part of the w/up, especially because 3% of pts with normal CT scans show evidence of hemorrhage on LP. An RBC count of >100,000/m3 strongly suggests SAH. If RBC counts ↓ between the first and fourth tubes, then the tap is most likely traumatic. The presence of xanthochromia or bilirubin in the CSF is a sign of SAH.
LP is a very important part of the w/up, especially because 3% of pts with normal CT scans show evidence of hemorrhage on LP. An RBC count of >100,000/m3 strongly suggests SAH. If RBC counts ↓ between the first and fourth tubes, then the tap is most likely traumatic. The presence of xanthochromia or bilirubin in the CSF is a sign of SAH.Treatment
 Management of SAH varies w/the pt’s clinical status (Table 10-10), as well as the location (see Fig. 10-3) and surgical accessibility of the aneurysm.
Management of SAH varies w/the pt’s clinical status (Table 10-10), as well as the location (see Fig. 10-3) and surgical accessibility of the aneurysm.TABLE 10-10
Glasgow Coma Scale∗
| Eyes | Motor | Verbal |
| 1. None | 1. None | 1. None |
| 2. To pain | 2. Abnl extension | 2. Incomprehensible (groaning) |
| 3. To speech | 3. Abnl flexion | 3. Inappropriate |
| 4. Spontaneous | 4. Flexion (withdrawal) | 4. Disoriented, confused |
| 5. Localizing | 5. Oriented | |
| 6. Obeying commands |
∗ The best score for each response should be documented and communicated in the format described above. Assessment of the best motor score is based on the best response of the arms. For use in individual pts, separate description of the three components of the GCS is strongly recommended. For purposes of classification, the total GCS can be calculated by adding the best score obtained in each category. The GCS should be annotated to indicate confounding factors: T signifies an intubated pt; S, sedation; P, neuromuscular blockade.
From Vincent JL, Abraham E, Moore FA, et al (eds): Textbook of Critical Care, 6th ed. Philadelphia, Saunders, 2011.
 Pts with a depressed level of consciousness may need to be intubated and mechanically ventilated in an ICU setting.
Pts with a depressed level of consciousness may need to be intubated and mechanically ventilated in an ICU setting. A lumbar drain or ventriculostomy is required should the pt develop hydrocephalus and ↑ ICP.
A lumbar drain or ventriculostomy is required should the pt develop hydrocephalus and ↑ ICP. Initial management strategies are geared toward stabilizing the pt and preventing recurrent hemorrhage and hydrocephalus.
Initial management strategies are geared toward stabilizing the pt and preventing recurrent hemorrhage and hydrocephalus. Tight BP control is paramount. This can be done with the use of drips (e.g., nitroprusside) or PRN medications. An SBP 120 to 150 mm Hg is recommended.
Tight BP control is paramount. This can be done with the use of drips (e.g., nitroprusside) or PRN medications. An SBP 120 to 150 mm Hg is recommended. After an aneurysm has been identified, measures to secure it should be undertaken; this can be done by either clipping or coiling the aneurysm. Clipping consists of placing a clip around the neck of the aneurysm and is performed via intra-arterial angiography; it consists of deploying platinum coils inside the aneurysm to cause thrombosis of the aneurysmal sac.
After an aneurysm has been identified, measures to secure it should be undertaken; this can be done by either clipping or coiling the aneurysm. Clipping consists of placing a clip around the neck of the aneurysm and is performed via intra-arterial angiography; it consists of deploying platinum coils inside the aneurysm to cause thrombosis of the aneurysmal sac. Pain control is performed with the use of short-acting and less-sedating medications (e.g., codeine, low-dose morphine).
Pain control is performed with the use of short-acting and less-sedating medications (e.g., codeine, low-dose morphine). Seizures occur in ≤3% of pts during the acute phase; however, the use of prophylactic antiepileptics is still controversial.
Seizures occur in ≤3% of pts during the acute phase; however, the use of prophylactic antiepileptics is still controversial. Vasospasm, which typically begins around day 3 after the hemorrhage and reaches a peak on day 6 to 8, is the leading cause of death and disability after aneurysm rupture. Nimodipine has been shown to improve outcomes if it is administered between days 4 and 21 after the hemorrhage, even if it does not significantly reduce the amount of vasospasm detected on angiography. After vasospasm develops, “triple H” therapy—to achieve Hypertension, Hypervolemia, and Hemodilution—is used in an attempt to provide adequate cerebral perfusion.
Vasospasm, which typically begins around day 3 after the hemorrhage and reaches a peak on day 6 to 8, is the leading cause of death and disability after aneurysm rupture. Nimodipine has been shown to improve outcomes if it is administered between days 4 and 21 after the hemorrhage, even if it does not significantly reduce the amount of vasospasm detected on angiography. After vasospasm develops, “triple H” therapy—to achieve Hypertension, Hypervolemia, and Hemodilution—is used in an attempt to provide adequate cerebral perfusion.4. Sinus Venous Thrombosis
Etiology
 Staphylococcus aureus (50%-60%), Streptococcus (second leading cause), gram(−) rods/anaerobes; sphenoid sinusitis (most common site)
Staphylococcus aureus (50%-60%), Streptococcus (second leading cause), gram(−) rods/anaerobes; sphenoid sinusitis (most common site)Diagnosis
H&P
 Ptosis, proptosis
Ptosis, proptosis Chemosis
Chemosis CN palsies (III, IV, V (VI and VII), VI); VI is most common
CN palsies (III, IV, V (VI and VII), VI); VI is most common Sensory deficits of the ophthalmic/maxillary branch of the fifth nerve are common.
Sensory deficits of the ophthalmic/maxillary branch of the fifth nerve are common.Labs
 CBC, ESR, blood/sinus cultures (identify infectious primary source)
CBC, ESR, blood/sinus cultures (identify infectious primary source) LP necessary to r/o meningitis
LP necessary to r/o meningitisImaging
 MRV, MRI w/gadolinium including MR angiography
MRV, MRI w/gadolinium including MR angiographyTreatment
 Rx should take into account the primary source of infection, as well as possible associated complications, such as brain abscess, meningitis, or subdural empyema.
Rx should take into account the primary source of infection, as well as possible associated complications, such as brain abscess, meningitis, or subdural empyema. Broad-spectrum IV abx are used as empiric Rx until a definite pathogen is found. Rx should include a penicillinase-resistant PCN at maximum dose plus a third- or fourth-generation ceph:
Broad-spectrum IV abx are used as empiric Rx until a definite pathogen is found. Rx should include a penicillinase-resistant PCN at maximum dose plus a third- or fourth-generation ceph: Anticoagulation w/heparin: controversial. Cerebral infarction or ICH should first be ruled out by non–contrast-enhanced CT scan before initiation of heparin Rx. Current recommendation is for early heparinization in pts w/unilateral CST to prevent clot propagation and to ↑ the incidence of septic emboli. Warfarin Rx should be avoided in the acute phase of the illness but should ultimately be instituted to achieve an INR of 2 to 3 and continued until the infection, sx, and signs of CST have resolved or significantly improved.
Anticoagulation w/heparin: controversial. Cerebral infarction or ICH should first be ruled out by non–contrast-enhanced CT scan before initiation of heparin Rx. Current recommendation is for early heparinization in pts w/unilateral CST to prevent clot propagation and to ↑ the incidence of septic emboli. Warfarin Rx should be avoided in the acute phase of the illness but should ultimately be instituted to achieve an INR of 2 to 3 and continued until the infection, sx, and signs of CST have resolved or significantly improved. Steroid Rx: controversial but may prove helpful in ↓ cranial nerve dysfunction or when progression to pituitary insufficiency occurs. Corticosteroids should be instituted only after appropriate abx coverage. Dexamethasone 10 mg q6h is the Rx of choice.
Steroid Rx: controversial but may prove helpful in ↓ cranial nerve dysfunction or when progression to pituitary insufficiency occurs. Corticosteroids should be instituted only after appropriate abx coverage. Dexamethasone 10 mg q6h is the Rx of choice. Emergency surgical drainage w/sphenoidotomy: indicated if the primary site of infection is thought to be the sphenoid sinus.
Emergency surgical drainage w/sphenoidotomy: indicated if the primary site of infection is thought to be the sphenoid sinus. All pts w/CST are usually treated w/prolonged courses (3-4 wk) of IV abx. If there is evidence of complications such as intracranial suppuration, 6 to 8 wk of total Rx may be warranted.
All pts w/CST are usually treated w/prolonged courses (3-4 wk) of IV abx. If there is evidence of complications such as intracranial suppuration, 6 to 8 wk of total Rx may be warranted. All pts should be monitored for signs of complicated infection, continued sepsis, or septic emboli while abx Rx is being administered.
All pts should be monitored for signs of complicated infection, continued sepsis, or septic emboli while abx Rx is being administered.5. Stroke Prevention: Asymptomatic Carotid Stenosis
Etiology
 Atherosclerosis (most common)
Atherosclerosis (most common) Aneurysm
Aneurysm Arteritis
Arteritis Carotid dissection
Carotid dissection Postradiation necrosis
Postradiation necrosis Vasospasm
Vasospasm Risk factors: HTN, dyslipidemia, DM, and smoking
Risk factors: HTN, dyslipidemia, DM, and smokingDiagnosis
 Carotid duplex. If carotid stenosis is suspected on carotid duplex, but results are inconclusive, MRI, CT angiography, or traditional angiography should be obtained to confirm the degree of stenosis.
Carotid duplex. If carotid stenosis is suspected on carotid duplex, but results are inconclusive, MRI, CT angiography, or traditional angiography should be obtained to confirm the degree of stenosis.H&P
 Pts with carotid stenosis are often asymptomatic, but many have presence of a carotid bruit or TIA.
Pts with carotid stenosis are often asymptomatic, but many have presence of a carotid bruit or TIA.Treatment (Table 10-11)
 CEA and carotid angioplasty and stenting are available.
CEA and carotid angioplasty and stenting are available. CEA: The selection of surgical candidates should be guided primarily by the presence or absence of symptoms and the degree of stenosis.
CEA: The selection of surgical candidates should be guided primarily by the presence or absence of symptoms and the degree of stenosis.Asymptomatic Pts
 CEA should be considered in asymptomatic pts only if the perioperative risk for stroke and death at the given surgical institution is <3%.
CEA should be considered in asymptomatic pts only if the perioperative risk for stroke and death at the given surgical institution is <3%. CEA should be considered in pts between the ages of 40 and 75 yr with an asymptomatic 60% to 99% stenosis if their life expectancy is >5 yr and the perioperative stroke and mortality rates are <3%. However, medical therapy has improved since early trials comparing medical management and revascularization, and many experts are favoring intensified medical management rather than revascularization procedures in pts with ACS.
CEA should be considered in pts between the ages of 40 and 75 yr with an asymptomatic 60% to 99% stenosis if their life expectancy is >5 yr and the perioperative stroke and mortality rates are <3%. However, medical therapy has improved since early trials comparing medical management and revascularization, and many experts are favoring intensified medical management rather than revascularization procedures in pts with ACS. All pts undergoing CEA should be started on aspirin (ASA 81 or 325 mg daily) before surgery, and aspirin should be continued indefinitely.
All pts undergoing CEA should be started on aspirin (ASA 81 or 325 mg daily) before surgery, and aspirin should be continued indefinitely.Symptomatic Pts
 CEA is recommended for recently symptomatic pts with 70% to 99% stenosis if their life expectancy is >5 yr and perioperative risk for mortality is <6%.
CEA is recommended for recently symptomatic pts with 70% to 99% stenosis if their life expectancy is >5 yr and perioperative risk for mortality is <6%. CEA is beneficial for recently symptomatic men with 50% to 69% stenosis if their life expectancy is >5 yr and perioperative risk of mortality is <6%. Medical management is recommended for pts with stenosis <50%.
CEA is beneficial for recently symptomatic men with 50% to 69% stenosis if their life expectancy is >5 yr and perioperative risk of mortality is <6%. Medical management is recommended for pts with stenosis <50%. General medical therapy should be aimed at risk factor reduction. Major risk factors for carotid stenosis are HTN, DM, lipid disorders, and smoking.
General medical therapy should be aimed at risk factor reduction. Major risk factors for carotid stenosis are HTN, DM, lipid disorders, and smoking. Antiplatelet therapy: Three antiplatelet options are available for pts with carotid stenosis: ASA, ASA plus dipyridamole, and clopidogrel.
Antiplatelet therapy: Three antiplatelet options are available for pts with carotid stenosis: ASA, ASA plus dipyridamole, and clopidogrel.TABLE 10-11
Carotid Stenosis Management
| Degree of Carotid Stenosis | <50% | 50%-69% | 70%-99% |
| Asymptomatic | Medical management | Men: CEA if stenosis >60% and age <75 yr; otherwise, medical management Women: medical management |
Men <75 yr: CEA Women: medical management |
| Symptomatic | Medical management | Men: CEA Women: medical management |
Men: CEA Women: CEA |
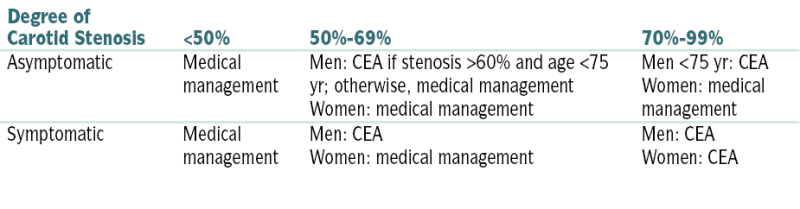
From Ferri F: Ferri’s Clinical Advisor: 5 Books in 1. 2013 edition. Philadelphia, Mosby, 2012.
D. Headaches
1. Migraine (Aura, Trigger)
Treatment
Acute Abortive Rx
 Triptans (SC, PO, and intranasal) are the drug class of choice for abortive Rx.
Triptans (SC, PO, and intranasal) are the drug class of choice for abortive Rx. Early administration improves effectiveness.
Early administration improves effectiveness.Prophylactic Rx
 Prophylactic Rx is generally indicated when headaches occur >once/wk or when symptomatic Rxs are contraindicated or not effective. All prophylaxis should be maintained for ≥3 mo before deeming the medication a failure.
Prophylactic Rx is generally indicated when headaches occur >once/wk or when symptomatic Rxs are contraindicated or not effective. All prophylaxis should be maintained for ≥3 mo before deeming the medication a failure.TABLE 10-12
Differential Diagnosis of Headache
| Headache Type | Genetics | Epidemiology | Characteristic Features | Length | Accompanying Symptoms |
| Migraine headache | Complex genetics but usually a fhx | More frequent in women | Unilateral, bilateral; throbbing; moderate to severe; worsens with activity | Hours to days | Photophobia, phonophobia, nausea and/or vomiting |
| Tension-type headache | Usually a fhx | Equally frequent in men and women | Tight bandlike pain; bilateral; pain may be mild to moderate; improves with activity | Hours to days | No nausea or vomiting; small amount of light or sound sensitivity, but not both |
| Cluster headache | Possibly a fhx | More frequent in men | Unilateral, severe pain in the face | Minutes to hour | Ipsilateral ptosis, miosis, rhinorrhea, eyelid edema, tearing |
| Paroxysmal hemicrania | Usually no fhx | More frequent in women | Unilateral pain in the face | Minutes | Ipsilateral ptosis, miosis, rhinorrhea, eyelid edema, tearing; responds to indomethacin |
| Hemicrania continua | No fhx | More frequent in women | Unilateral, continuous headache with episodic stabbing pains | Continuous | Ipsilateral autonomic features: ptosis, miosis, rhinorrhea, eyelid edema, tearing |
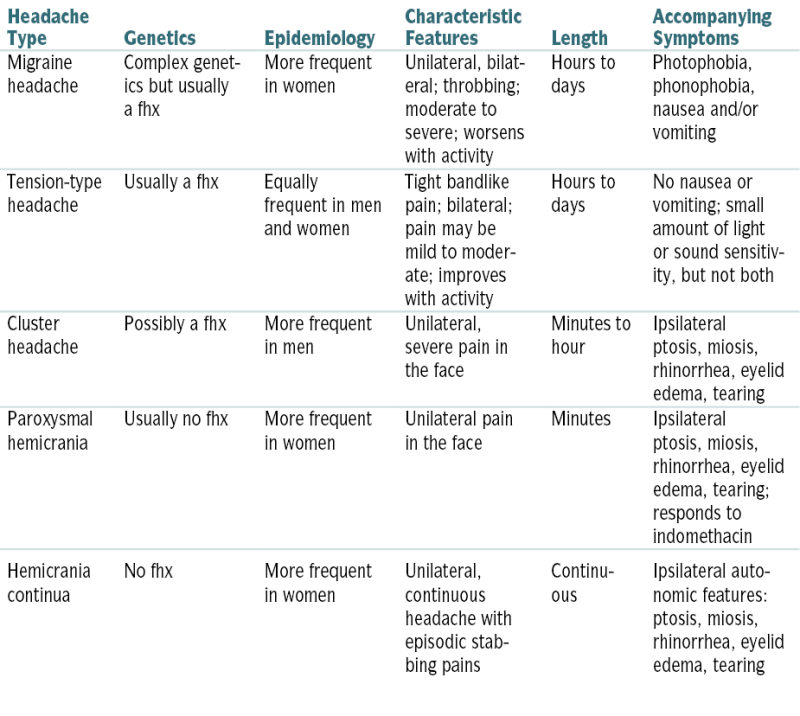
fhx = family history
From Goldman L, Schafer AI (eds): Goldman’s Cecil Medicine, 24th ed. Philadelphia, Saunders, 2012.
 Options include β-blockers (propranolol, timolol, atenolol, metoprolol), tricyclic antidepressants (amitriptyline), and the antiepileptic drug valproic acid.
Options include β-blockers (propranolol, timolol, atenolol, metoprolol), tricyclic antidepressants (amitriptyline), and the antiepileptic drug valproic acid. Less-established options include Ca2+ channel blockers, selective serotonin reuptake inhibitors, and the antiepileptic drugs gabapentin and topiramate. The FDA has approved injection of onabotulinum toxin A (Botox) for prevention of headaches in adult pts with chronic migraines (≥15 headache days/mo for ≥3 mo).
Less-established options include Ca2+ channel blockers, selective serotonin reuptake inhibitors, and the antiepileptic drugs gabapentin and topiramate. The FDA has approved injection of onabotulinum toxin A (Botox) for prevention of headaches in adult pts with chronic migraines (≥15 headache days/mo for ≥3 mo).2. Tension-Type Headache (Bilateral, Vice-Like)
Treatment
 Relaxation and cognitive-behavioral Rx (especially in adolescents and children), Schultz-type autogenic training (relaxation technique based on passive concentration and body awareness of specific sensations), transcutaneous electrical nerve stimulation, heat
Relaxation and cognitive-behavioral Rx (especially in adolescents and children), Schultz-type autogenic training (relaxation technique based on passive concentration and body awareness of specific sensations), transcutaneous electrical nerve stimulation, heatAcute General Treatment
 Nonnarcotic analgesics with limited frequency to prevent drug-induced and/or rebound headache
Nonnarcotic analgesics with limited frequency to prevent drug-induced and/or rebound headacheChronic Treatment
 Tricyclic antidepressants (amitriptyline 10-150 mg qhs) and SSRIs
Tricyclic antidepressants (amitriptyline 10-150 mg qhs) and SSRIs Avoid narcotics, limit NSAIDs, consider indomethacin; if related to cervical muscle spasm, consider a trial of muscle relaxants (e.g., metaxalone [Skelaxin] 400- 800 mg tid).
Avoid narcotics, limit NSAIDs, consider indomethacin; if related to cervical muscle spasm, consider a trial of muscle relaxants (e.g., metaxalone [Skelaxin] 400- 800 mg tid).3. Cluster Headache (Unilateral, Lacrimation, Periorbital)
Treatment
Abortive Treatment
 Inhalation of 100% O2 by face mask for 15 min often aborts an attack.
Inhalation of 100% O2 by face mask for 15 min often aborts an attack. 75% of users of triptans (sumatriptan, zolmitriptan) are pain free within 20 min.
75% of users of triptans (sumatriptan, zolmitriptan) are pain free within 20 min. Ergotamine (Cafergot), octreotide, intranasal lidocaine, or dihydroergotamine may abort an attack or prevent one if given just before a predictable episode.
Ergotamine (Cafergot), octreotide, intranasal lidocaine, or dihydroergotamine may abort an attack or prevent one if given just before a predictable episode.Prophylaxis Treatment
 Various medications have been tried without great success, although good responses may be obtained in up to 50% of cases. Examples include:
Various medications have been tried without great success, although good responses may be obtained in up to 50% of cases. Examples include:4. Idiopathic Intracranial Hypertension (IIH; Pseudotumor Cerebri)
Diagnosis
H&P
 Symptoms
Symptoms Signs
SignsLabs
 CSF analysis: ↑ opening pressure, nl protein, glucose, and cell count
CSF analysis: ↑ opening pressure, nl protein, glucose, and cell count Hypercoagulability w/up if suspicion of venous sinus thrombosis
Hypercoagulability w/up if suspicion of venous sinus thrombosisImaging
 Brain MRI r/o underlying structural lesions; empty sella sign often associated w/IIH but not pathognomonic
Brain MRI r/o underlying structural lesions; empty sella sign often associated w/IIH but not pathognomonic Cerebral venography/MRV to evaluate venous flow
Cerebral venography/MRV to evaluate venous flow CT (slit-like ventricles)
CT (slit-like ventricles)Treatment
 Weight loss in obese pts
Weight loss in obese pts CPAP if obstructive sleep apnea suspected
CPAP if obstructive sleep apnea suspected Acetazolamide 250 mg to 4 g/day: ↓ CSF production occurs by inhibition of carbonic anhydrase, occasionally causing anorexia and resultant weight loss.
Acetazolamide 250 mg to 4 g/day: ↓ CSF production occurs by inhibition of carbonic anhydrase, occasionally causing anorexia and resultant weight loss. Furosemide 40 to 120 mg/day in divided doses: Apparent mechanism of action is by ↓ Na+ transport, leading to ↓ total CSF volume.
Furosemide 40 to 120 mg/day in divided doses: Apparent mechanism of action is by ↓ Na+ transport, leading to ↓ total CSF volume. Topiramate 100 to 400 mg/day: This antiepileptic medication, reported to be effective in Rx of IIH, is a weak carbonic anhydrase inhibitor with weight loss as one of its primary side effects.
Topiramate 100 to 400 mg/day: This antiepileptic medication, reported to be effective in Rx of IIH, is a weak carbonic anhydrase inhibitor with weight loss as one of its primary side effects. Serial LP is attempted in pts with severe headaches resistant to medical Rx. Goal is to ↓ spinal fluid pressure, thus allowing immediate reduction in headache severity. This Rx should be reserved only for the most resistant cases and should be used as a conduit to future surgical intervention.
Serial LP is attempted in pts with severe headaches resistant to medical Rx. Goal is to ↓ spinal fluid pressure, thus allowing immediate reduction in headache severity. This Rx should be reserved only for the most resistant cases and should be used as a conduit to future surgical intervention. Surgical intervention is indicated in cases of Rx failure and progressive visual loss.
Surgical intervention is indicated in cases of Rx failure and progressive visual loss. Optic nerve fenestration is preferred for pts with visual loss and easily controlled headaches.
Optic nerve fenestration is preferred for pts with visual loss and easily controlled headaches.E. Movement Disorders
1. Parkinson’s Disease (PD)
Diagnosis
 The four cardinal signs used to diagnose PD are (mnemonic = TRAP):
The four cardinal signs used to diagnose PD are (mnemonic = TRAP): One need not show all four cardinal signs to make a presumptive diagnosis of PD and begin treatment.
One need not show all four cardinal signs to make a presumptive diagnosis of PD and begin treatment.Imaging
 MRI of the head may sometimes distinguish between idiopathic PD and other conditions that manifest with signs of parkinsonism.
MRI of the head may sometimes distinguish between idiopathic PD and other conditions that manifest with signs of parkinsonism.Treatment
 Physical therapy, pt education and reassurance, treatment of associated conditions (e.g., depression)
Physical therapy, pt education and reassurance, treatment of associated conditions (e.g., depression) Avoidance of drugs that can induce or worsen parkinsonism: neuroleptics (especially high potency), certain antiemetics (prochlorperazine, trimethobenzamide), metoclopramide, nonselective MAO inhibitors (may induce hypertensive crisis), reserpine, methyldopa
Avoidance of drugs that can induce or worsen parkinsonism: neuroleptics (especially high potency), certain antiemetics (prochlorperazine, trimethobenzamide), metoclopramide, nonselective MAO inhibitors (may induce hypertensive crisis), reserpine, methyldopaMedical Treatment
 Whether levodopa or dopamine agonists should be the initial treatment remains controversial. In younger pts, agonists are usually the drug of choice; in pts >70 yr, levodopa is typically the drug of choice.
Whether levodopa or dopamine agonists should be the initial treatment remains controversial. In younger pts, agonists are usually the drug of choice; in pts >70 yr, levodopa is typically the drug of choice. Levodopa is the cornerstone of symptomatic therapy. It should be used with a peripheral dopa decarboxylase inhibitor (carbidopa) to minimize side effects (nausea, lightheadedness, postural hypotension). The combination of the two drugs is marketed under the trade name Sinemet. Levodopa therapy has been found to reduce morbidity and mortality in pts w/PD.
Levodopa is the cornerstone of symptomatic therapy. It should be used with a peripheral dopa decarboxylase inhibitor (carbidopa) to minimize side effects (nausea, lightheadedness, postural hypotension). The combination of the two drugs is marketed under the trade name Sinemet. Levodopa therapy has been found to reduce morbidity and mortality in pts w/PD. Dopamine receptor agonists (Ropinirole and Pramipexole) are not as potent as levodopa, but they are often used as initial treatment in younger pts to attempt to delay the onset of complications (dyskinesias, motor fluctuations) associated with levodopa therapy. In general these drugs cause more side effects than levodopa, including nausea, vomiting, lightheadedness, peripheral edema, confusion, and somnolence. They can also cause impulse control behaviors such as hypersexuality, binge eating, and compulsive shopping and gambling. Presence of these behaviors must be assessed at each visit.
Dopamine receptor agonists (Ropinirole and Pramipexole) are not as potent as levodopa, but they are often used as initial treatment in younger pts to attempt to delay the onset of complications (dyskinesias, motor fluctuations) associated with levodopa therapy. In general these drugs cause more side effects than levodopa, including nausea, vomiting, lightheadedness, peripheral edema, confusion, and somnolence. They can also cause impulse control behaviors such as hypersexuality, binge eating, and compulsive shopping and gambling. Presence of these behaviors must be assessed at each visit. MAO-B inhibitors (rasagiline, selegiline, amantadine) can be used as monotherapy early in the disease or as adjunctive therapy in later stages. They have milder symptomatic benefit than dopamine agonists or levodopa and are well tolerated and easy to titrate. Concurrent use of stimulants and sympathomimetics should be avoided. Certain food restrictions may apply.
MAO-B inhibitors (rasagiline, selegiline, amantadine) can be used as monotherapy early in the disease or as adjunctive therapy in later stages. They have milder symptomatic benefit than dopamine agonists or levodopa and are well tolerated and easy to titrate. Concurrent use of stimulants and sympathomimetics should be avoided. Certain food restrictions may apply. Anticholinergic agents (trihexyphenidyl, benztropine) are helpful only in treating tremor and drooling in pts w/PD. Potential side effects include constipation, urinary retention, memory impairment, and hallucinations. These drugs should be avoided in elderly pts.
Anticholinergic agents (trihexyphenidyl, benztropine) are helpful only in treating tremor and drooling in pts w/PD. Potential side effects include constipation, urinary retention, memory impairment, and hallucinations. These drugs should be avoided in elderly pts.Surgical Options
 Pallidal (globus pallidus interna) and subthalamic deep brain stimulation (DBS; subthalamic nucleus) are currently the surgical options of choice for pts w/advanced PD; similar improvement in motor function and adverse effects have been reported after either procedure. Compared with ablative procedures, DBS has the advantage of being reversible and adjustable. Thalamic DBS may be useful for refractory tremor. It improves the cardinal motor symptoms, extends medication “on” time, and reduces motor fluctuations during the day. In general pts are likely to benefit from this therapy if they show a clear response to levodopa. Therefore, when considering DBS, pts should be evaluated for motor response to levodopa by stopping levodopa overnight and evaluating motor response before and after a dose of levodopa.
Pallidal (globus pallidus interna) and subthalamic deep brain stimulation (DBS; subthalamic nucleus) are currently the surgical options of choice for pts w/advanced PD; similar improvement in motor function and adverse effects have been reported after either procedure. Compared with ablative procedures, DBS has the advantage of being reversible and adjustable. Thalamic DBS may be useful for refractory tremor. It improves the cardinal motor symptoms, extends medication “on” time, and reduces motor fluctuations during the day. In general pts are likely to benefit from this therapy if they show a clear response to levodopa. Therefore, when considering DBS, pts should be evaluated for motor response to levodopa by stopping levodopa overnight and evaluating motor response before and after a dose of levodopa. Surgery is limited to patients with disabling, medically refractory problems, and pts must still have a good response to L-dopa to undergo surgery. DBS results in decreased dyskinesias, fluctuations, rigidity, and tremor.
Surgery is limited to patients with disabling, medically refractory problems, and pts must still have a good response to L-dopa to undergo surgery. DBS results in decreased dyskinesias, fluctuations, rigidity, and tremor.2. Ataxia
 Vertebral-basilar artery ischemia
Vertebral-basilar artery ischemia AIDS
AIDS Diabetic neuropathy
Diabetic neuropathy Vitamin B12 deficiency
Vitamin B12 deficiency MS and other demyelinating diseases
MS and other demyelinating diseases Meningomyelopathy
Meningomyelopathy Cerebellar neoplasms, hemorrhage, abscess, infarct
Cerebellar neoplasms, hemorrhage, abscess, infarct Nutritional (Wernicke’s encephalopathy)
Nutritional (Wernicke’s encephalopathy) Paraneoplastic syndromes
Paraneoplastic syndromes Parainfectious: GBS, acute ataxia of childhood and young adults
Parainfectious: GBS, acute ataxia of childhood and young adults Toxins: phenytoin, alcohol, sedatives, organophosphates
Toxins: phenytoin, alcohol, sedatives, organophosphates Wilson’s disease (hepatolenticular degeneration)
Wilson’s disease (hepatolenticular degeneration) Hypothyroidism
Hypothyroidism Myopathy
Myopathy Cerebellar and spinocerebellar degeneration: ataxia-telangiectasia, Friedreich’s ataxia
Cerebellar and spinocerebellar degeneration: ataxia-telangiectasia, Friedreich’s ataxia Frontal lobe lesions: tumors, thrombosis of anterior cerebral artery, hydrocephalus
Frontal lobe lesions: tumors, thrombosis of anterior cerebral artery, hydrocephalus Labyrinthine destruction: neoplasm, injury, inflammation, compression
Labyrinthine destruction: neoplasm, injury, inflammation, compression Hysteria
Hysteria Tabes dorsalis
Tabes dorsalis3. Essential Tremor
Etiology
 Often inherited (autosomal dominant); sporadic cases w/o an fhx also encountered
Often inherited (autosomal dominant); sporadic cases w/o an fhx also encounteredDiagnosis
 Pts complain of tremor that is most bothersome when writing or holding something, such as a newspaper, or trying to drink from a cup. It worsens under emotional duress and is made better w/alcohol ingestion.
Pts complain of tremor that is most bothersome when writing or holding something, such as a newspaper, or trying to drink from a cup. It worsens under emotional duress and is made better w/alcohol ingestion. Tremor, 4 to 12 Hz, bilateral postural and action tremor of the UEs; may also affect the head, voice, trunk, and legs. Table 10-13 compares essential tremor with cerebellar and parkinsonian tremor.
Tremor, 4 to 12 Hz, bilateral postural and action tremor of the UEs; may also affect the head, voice, trunk, and legs. Table 10-13 compares essential tremor with cerebellar and parkinsonian tremor.TABLE 10-13
Distinguishing Features of Parkinsonian, Cerebellar, and Essential Tremor
| Feature | Parkinson’s Syndrome | Cerebellar Tremor | Essential Tremor |
| Present at rest | Yes | No | Yes |
| Increased tone | Yes | No | No |
| Decreased tone | No | Yes | No |
| Postural abnlity | Yes | Yes | No |
| Head involvement | Yes | Yes | Yes |
| Intentional component | No | Yes | Yes |
| Incoordination | No | Yes | No |
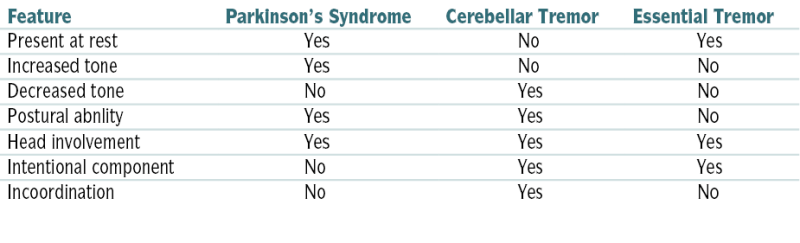
From Remmel KS, Bunyan R, Brunback R, et al: Handbook of Symptom-Oriented Neurology, 3rd ed. St. Louis, Mosby, 2002.
Treatment
 Propranolol
Propranolol Primidone
Primidone4. Dystonia
Etiology
 Primary dystonia is believed to involve ↓/abnl basal ganglia activity resulting in disinhibition of motor thalamus and cortex, thus producing abnl movement.
Primary dystonia is believed to involve ↓/abnl basal ganglia activity resulting in disinhibition of motor thalamus and cortex, thus producing abnl movement. Secondary dystonia results from CNS disease of basal ganglia (stroke, demyelination, hypoxia, trauma, Huntington’s disease, Wilson’s disease, Parkinson’s syndromes, and lysosomal storage diseases).
Secondary dystonia results from CNS disease of basal ganglia (stroke, demyelination, hypoxia, trauma, Huntington’s disease, Wilson’s disease, Parkinson’s syndromes, and lysosomal storage diseases). Acute dystonia is caused by drugs that block dopamine receptors.
Acute dystonia is caused by drugs that block dopamine receptors. TD can result from long-term Rx with antiemetics (e.g., phenothiazines), antipsychotics (e.g., haloperidol), levodopa, anticonvulsants, or ergots.
TD can result from long-term Rx with antiemetics (e.g., phenothiazines), antipsychotics (e.g., haloperidol), levodopa, anticonvulsants, or ergots.Diagnosis
 Hx (family hx, birth hx, trauma, medication use)
Hx (family hx, birth hx, trauma, medication use) Physical examination
Physical examinationH&P
 Focal dystonias
Focal dystonias Generalized dystonia
Generalized dystoniaLabs
 Usually not helpful for dx
Usually not helpful for dx Serum ceruloplasmin if Wilson’s disease is suspected
Serum ceruloplasmin if Wilson’s disease is suspectedImaging
 Primary dystonias are generally not associated with structural CNS abnormalities. CT scan or MRI of brain is indicated if a CNS lesion is suspected as a cause of secondary dystonia.
Primary dystonias are generally not associated with structural CNS abnormalities. CT scan or MRI of brain is indicated if a CNS lesion is suspected as a cause of secondary dystonia. Electrophysiologic testing can provide support for the dx.
Electrophysiologic testing can provide support for the dx.Treatment
Acute Treatment
 For acute dystonic reactions to phenothiazines/butyrophenones, use diphenhydramine 50 mg IV or benztropine 2 mg IV.
For acute dystonic reactions to phenothiazines/butyrophenones, use diphenhydramine 50 mg IV or benztropine 2 mg IV.Chronic Treatment
 Pharmacologic Rx is often ineffective.
Pharmacologic Rx is often ineffective. Slowly withdraw offending agents.
Slowly withdraw offending agents. Diazepam, baclofen, or carbamazepine may be helpful.
Diazepam, baclofen, or carbamazepine may be helpful. Intrathecal baclofen is most useful for spastic or truncal dystonia.
Intrathecal baclofen is most useful for spastic or truncal dystonia. Trihexyphenidyl or benztropine may be helpful in up to 50% of tardive dystonias.
Trihexyphenidyl or benztropine may be helpful in up to 50% of tardive dystonias. For generalized dystonia, a trial of carbidopa/levodopa may be beneficial and diagnostic of dopa-responsive dystonia (DYT5).
For generalized dystonia, a trial of carbidopa/levodopa may be beneficial and diagnostic of dopa-responsive dystonia (DYT5). Injection of botulinum toxin into the affected muscles is the standard Rx.
Injection of botulinum toxin into the affected muscles is the standard Rx. Surgical procedures, including denervation, myectomy, rhizotomy, thalamotomy (pallidotomy), or functional stereotactic surgery, may be helpful for severe, refractory cases.
Surgical procedures, including denervation, myectomy, rhizotomy, thalamotomy (pallidotomy), or functional stereotactic surgery, may be helpful for severe, refractory cases. DBS is becoming more promising, especially for refractory primary generalized dystonias.
DBS is becoming more promising, especially for refractory primary generalized dystonias.5. Chorea
Etiology
 Pathology to the basal ganglia resulting in a pattern of discrete, randomly occurring jerks or twitches, either generalized or confined to a single body part
Pathology to the basal ganglia resulting in a pattern of discrete, randomly occurring jerks or twitches, either generalized or confined to a single body part The most common type of chorea is dyskinesia produced by dopamine drugs in pts with PD.
The most common type of chorea is dyskinesia produced by dopamine drugs in pts with PD. The most common neurodegenerative choreic disorder is Huntington’s disease.
The most common neurodegenerative choreic disorder is Huntington’s disease.Treatment
 Severity ↓ by dopamine-depleting or D2 receptor-blocking agents
Severity ↓ by dopamine-depleting or D2 receptor-blocking agents6. Tardive Dyskinesia (TD)
Treatment
 Clozapine has the best evidence for improving the sx of TD, although olanzapine and amisulpride may also be of benefit.
Clozapine has the best evidence for improving the sx of TD, although olanzapine and amisulpride may also be of benefit.7. Myoclonus
Treatment
 Carefully remove or ↓ potentially causative medications.
Carefully remove or ↓ potentially causative medications. For acute Rx of epileptic myoclonus, antiepileptic drugs such as valproic acid, levetiracetam, or clonazepam are helpful.
For acute Rx of epileptic myoclonus, antiepileptic drugs such as valproic acid, levetiracetam, or clonazepam are helpful. Clonazepam, valproic acid, levetiracetam are typically used for all forms of myoclonus, and often combinations of several medications seem to be more effective.
Clonazepam, valproic acid, levetiracetam are typically used for all forms of myoclonus, and often combinations of several medications seem to be more effective.8. Tourette’s Syndrome
Treatment
 Dopamine-blocking agents may be used to ↓ severity of tics acutely (e.g., haloperidol 0.25 mg PO qhs initially). There are risks of side effects, such as acute dystonic reactions.
Dopamine-blocking agents may be used to ↓ severity of tics acutely (e.g., haloperidol 0.25 mg PO qhs initially). There are risks of side effects, such as acute dystonic reactions. Clonidine: Many choose this as a first-line agent because of fewer long-term side effects. Start at 0.05 mg and slowly titrate to approximately 0.45 mg daily (needs tid/qid dosing). May also help with sx of ADHD.
Clonidine: Many choose this as a first-line agent because of fewer long-term side effects. Start at 0.05 mg and slowly titrate to approximately 0.45 mg daily (needs tid/qid dosing). May also help with sx of ADHD. Greater improvement in symptom severity among children with Tourette’s syndrome and chronic tic disorder has been reported with a comprehensive behavioral intervention compared with supportive Rx and education.
Greater improvement in symptom severity among children with Tourette’s syndrome and chronic tic disorder has been reported with a comprehensive behavioral intervention compared with supportive Rx and education. Important components of Rx are appropriate evaluation and Rx of coexisting conditions (e.g., ADHD, OCD).
Important components of Rx are appropriate evaluation and Rx of coexisting conditions (e.g., ADHD, OCD). DBS has shown some promising results as an alternative Rx in some pts with medically refractory disease.
DBS has shown some promising results as an alternative Rx in some pts with medically refractory disease.9. Wilson’s Disease
Diagnosis
H&P
 Chronic liver disease/cirrhosis with hepatosplenomegaly, ascites, ↓ serum alb, prolonged prothrombin time, portal HTN
Chronic liver disease/cirrhosis with hepatosplenomegaly, ascites, ↓ serum alb, prolonged prothrombin time, portal HTN Neurologic presentation
Neurologic presentation Ocular: The Kayser-Fleischer ring is a gold-yellow ring seen at the periphery of the iris; these should be sought with slit-lamp examination by a skilled examiner.
Ocular: The Kayser-Fleischer ring is a gold-yellow ring seen at the periphery of the iris; these should be sought with slit-lamp examination by a skilled examiner. Stigmata of acute or chronic liver disease
Stigmata of acute or chronic liver diseaseLabs
 ↓ Serum ceruloplasmin level (<200 mg/L)
↓ Serum ceruloplasmin level (<200 mg/L) ↓ Serum copper (<65 μg/L)
↓ Serum copper (<65 μg/L) 24-hr urinary copper excretion > 100 μg (nl <30 μg) to support dx; ↑ to > 1200 μg/24 hr after 500 mg of D-penicillamine (nl <500 μg/24 hr)
24-hr urinary copper excretion > 100 μg (nl <30 μg) to support dx; ↑ to > 1200 μg/24 hr after 500 mg of D-penicillamine (nl <500 μg/24 hr) Liver bx (to confirm bx): hepatic copper content (>250 μg/g of dry weight) (nl is 20-50 μg)
Liver bx (to confirm bx): hepatic copper content (>250 μg/g of dry weight) (nl is 20-50 μg)Treatment
10. Restless Legs Syndrome (RLS)
Classification
 Primary RLS is without any obvious cause, with no associated disorder.
Primary RLS is without any obvious cause, with no associated disorder. Secondary RLS is associated with other medical conditions. The most common associations are pregnancy, iron deficiency anemia, ESRD, and PD.
Secondary RLS is associated with other medical conditions. The most common associations are pregnancy, iron deficiency anemia, ESRD, and PD.Diagnosis
 Polysomnography to document periodic limb movements during sleep
Polysomnography to document periodic limb movements during sleepLabs
 Iron status: serum ferritin, total iron binding capacity, percent saturation
Iron status: serum ferritin, total iron binding capacity, percent saturation CBC for anemia, in case of iron deficiency
CBC for anemia, in case of iron deficiency Metabolic panel: BUN and serum Cr for renal insufficiency
Metabolic panel: BUN and serum Cr for renal insufficiencyTreatment
 Rx options for RLS
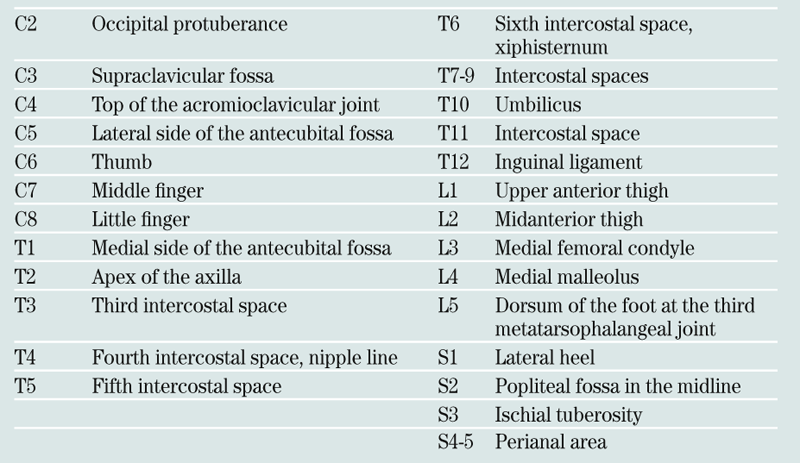
Rx options for RLSF. Dementia
Diagnosis
 There is no definitive imaging or lab test for the dx of Alzheimer’s disease and most forms of dementia; rather, dx depends on clinical history, a thorough physical and neurologic exam, and use of reliable and valid diagnostic criteria (i.e., DSM-V or NINDCS-ADRDA) such as the following:
There is no definitive imaging or lab test for the dx of Alzheimer’s disease and most forms of dementia; rather, dx depends on clinical history, a thorough physical and neurologic exam, and use of reliable and valid diagnostic criteria (i.e., DSM-V or NINDCS-ADRDA) such as the following:H&P
 Spouse or other family member, usually not the pt, notes insidious memory impairment.
Spouse or other family member, usually not the pt, notes insidious memory impairment. Pts have difficulties learning and retaining new information and handling complex tasks (e.g., balancing the checkbook), and they have impairments in reasoning, judgment, spatial ability, and orientation (e.g., difficulty driving, getting lost away from home).
Pts have difficulties learning and retaining new information and handling complex tasks (e.g., balancing the checkbook), and they have impairments in reasoning, judgment, spatial ability, and orientation (e.g., difficulty driving, getting lost away from home). Behavioral changes, such as mood changes and apathy, may accompany memory impairment. In later stages pts may develop agitation and psychosis.
Behavioral changes, such as mood changes and apathy, may accompany memory impairment. In later stages pts may develop agitation and psychosis. Atypical presentations include early and severe behavioral changes, focal findings on examination, parkinsonism, hallucinations, falls, or onset of symptoms younger than the age of 65.
Atypical presentations include early and severe behavioral changes, focal findings on examination, parkinsonism, hallucinations, falls, or onset of symptoms younger than the age of 65. Pts with isolated memory loss who lack functional impairment at home or work do not meet criteria for dementia but may have mild cognitive impairment (MCI). Identifying pts with MCI is important because pts with MCI may have a slightly higher rate of progression to dementia.
Pts with isolated memory loss who lack functional impairment at home or work do not meet criteria for dementia but may have mild cognitive impairment (MCI). Identifying pts with MCI is important because pts with MCI may have a slightly higher rate of progression to dementia. The diagnostic evaluation should include the following:
The diagnostic evaluation should include the following:TABLE 10-14
The Mini-Mental State Examination (MMSE)
| Parameter | Score |
| Orientation: What is the month, day, date, year, season? Where are you? What floor, city, country, state? (Score 1 point for each item correct.) | 10 |
| Registration: State three items (ball, flag, tree). (Score 1 point for each item that the pt registers without your having to repeat the words. You may repeat the words until the pt is able to register the words, but do not give the pt credit. You must also tell the pt that he/she should memorize those words and that you will ask him/her to recall those words later.) | 3 |
| Attention: Can you spell the word WORLD forward, then backward? Can you subtract 7 from 100, and keep subtracting 7? (100-93-86-79-72) (Do both items but give credit for the best of the two performances.) | 5 |
| Memory: Can you remember those three words I asked you to memorize? (Do not give clues or multiple choice.) | 3 |
| Language: | |
| Naming: Can you name (show) a pen and a watch? | 2 |
| Repetition: Can you repeat “No ifs, ands, or buts”? | 1 |
| Comprehension: Can you take this piece of paper in your right hand, fold it in half, then put it on the floor? (Score 1 point for each item done correctly.) | 3 |
| Reading: Read and obey “Close your eyes.” | 1 |
| Writing: Can you write a sentence? | 1 |
| Visuospatial: Have pt copy intersecting pentagons. | 1 |
| Total | 30 |
Interpretation: Traditionally, with use of a cutoff score of 23 of 30, the sensitivity and specificity of the MMSE have been reported to be 87% and 82%, respectively, for detection of delirium or dementia in hospitalized pts. However, cognitive performance as measured by the MMSE varies within the population by age and education. To adjust for these variables, it has been proposed that a cutoff score of 19 is appropriate for pts with 0 to 4 years of education and will identify those individuals performing below the level of 75% of their peers; the cutoff score should be 23 for those with 5 to 8 years of education and 27 for those with 9 to 12 years of education. A score <29 would be abnl in 75% of individuals with a college education.
Modified from Folstein MR, Folstein SE, McHugh PR: “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189, 1975.
 Of great importance is the identification of treatable causes of dementia:
Of great importance is the identification of treatable causes of dementia:Treatment
 Pursue the causes.
Pursue the causes. Avoid restraints, but use them for safety if necessary.
Avoid restraints, but use them for safety if necessary. Control hyperactivity of delirium w/haloperidol. Administer 0.5 to 1 mg IM, IV, or PO initially and the observe pt for 20 to 30 min. If the pt remains unmanageable but has not had any adverse reactions to haloperidol, double the dose and continue monitoring. Lorazepam 1 mg IM qh may also be administered if needed, but it often has a paradoxical effect in elderly pts.
Control hyperactivity of delirium w/haloperidol. Administer 0.5 to 1 mg IM, IV, or PO initially and the observe pt for 20 to 30 min. If the pt remains unmanageable but has not had any adverse reactions to haloperidol, double the dose and continue monitoring. Lorazepam 1 mg IM qh may also be administered if needed, but it often has a paradoxical effect in elderly pts. Donepezil, rivastigmine, and galantamine are reversible acetylcholinesterase inhibitors approved for Rx of mild to moderate dementia of Alzheimer’s type. They may be helpful in delaying the progression of Alzheimer’s disease if used in the early stages. They can provide modest improvement of sx and temporary stabilization of cognition by lengthening the time from assisted community living to nursing home placement. Memantine is an N-methyl-D-aspartate (NMDA) receptor blocker indicated for the Rx of moderate to severe Alzheimer’s disease. It can produce slight improvements in cognitive performance. The clinical significance of these improvements is small. Memantine can be used in combination w/anticholinesterase inhibitors.
Donepezil, rivastigmine, and galantamine are reversible acetylcholinesterase inhibitors approved for Rx of mild to moderate dementia of Alzheimer’s type. They may be helpful in delaying the progression of Alzheimer’s disease if used in the early stages. They can provide modest improvement of sx and temporary stabilization of cognition by lengthening the time from assisted community living to nursing home placement. Memantine is an N-methyl-D-aspartate (NMDA) receptor blocker indicated for the Rx of moderate to severe Alzheimer’s disease. It can produce slight improvements in cognitive performance. The clinical significance of these improvements is small. Memantine can be used in combination w/anticholinesterase inhibitors.G. Multiple Scerosis (MS)
TABLE 10-16
Summary of Revised 2005-2010 McDonald Criteria for Diagnosis of MS
| Clinical Attacks | Clinical Lesions | Paraclinical Testing Needed |
| 2 | 2 | None |
| 2 | 1 | MRI dissemination in space or two lesions on MRI consistent with MS plus positive CSF |
| 1 | 2 | MRI dissemination in time |
| 1 | 1 | MRI dissemination in space or two MRI lesions consistent with MS and positive CSF and MRI dissemination in time |
| Evidence of clinical lesions by physical examination or evoked potentials. | ||
| Diagnosis of PPMS: 1 year evidence of disease progression and two of the following: | ||
| (1) evidence for dissemination in space, (2) evidence for dissemination in time, or (3) positive CSF | ||
| MRI dissemination in space, by either (1) one or more T2 lesion in two of the four typical areas for MS lesions (periventricular, juxtacortical, infratentorial, or spinal cord) or (2) awaiting further clinical attack implicating a distinctly separate CNS region. MRI dissemination in time, a new enhancing lesion ≥3 mo or a new nonenhancing lesion ≥6 mo after the initial attack; positive CSF, positive oligoclonal bands or elevated immunoglobulin G index. | ||
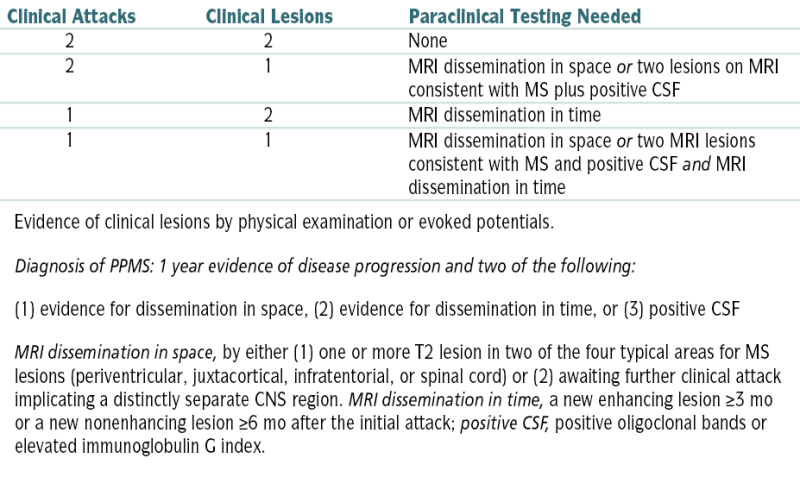
Modified from Degenhardt A: Ferri’s Clinical Advisor, 2013. St. Louis, Mosby, 2012, p. 700. Incorporates 2010 Revisions to Diagnostic criteria of MS (for details, please see original article: Polman CH, Reingold SC, Banwell B, et al: Diagnostic criteria for multiple sclerosis: 2010 revisions to McDonald’s criteria. Ann Neurol 69:292-302, 2011).
Diagnosis
 MS: based on revised 2005 McDonald criteria (see Table 10-16)
MS: based on revised 2005 McDonald criteria (see Table 10-16) RRMS: at least two relapses—two clinical lesions distinctly separated in space and time or one clinical lesion plus paraclinical testing
RRMS: at least two relapses—two clinical lesions distinctly separated in space and time or one clinical lesion plus paraclinical testing PPMS: insidious progression of disability with a positive CSF and either dissemination in both space and time or ongoing progression for ≥1 yr
PPMS: insidious progression of disability with a positive CSF and either dissemination in both space and time or ongoing progression for ≥1 yrH&P
 Visual abnlities
Visual abnlities Abnlities of reflexes
Abnlities of reflexes Lhermitte’s sign: flexion of the neck while the pt is lying down elicits an electrical sensation extending bilaterally down the arms, back, and lower trunk.
Lhermitte’s sign: flexion of the neck while the pt is lying down elicits an electrical sensation extending bilaterally down the arms, back, and lower trunk. Uhthoff’s phenomenon: exercise- or heat-induced deterioration of function
Uhthoff’s phenomenon: exercise- or heat-induced deterioration of function Charcot’s neurologic triad: nystagmus, scanning speech, and intention tremor
Charcot’s neurologic triad: nystagmus, scanning speech, and intention tremor Impaired recognition of objects by touch alone (astereognosis)
Impaired recognition of objects by touch alone (astereognosis)Imaging
 MRI of brain w/gadolinium can identify lesions as small as 3 to 4 mm and is used to assess disease load, activity, and progression.
MRI of brain w/gadolinium can identify lesions as small as 3 to 4 mm and is used to assess disease load, activity, and progression. MRI reveals multiple, predominantly periventricular plaques; however, normal MRI cannot be used to exclude MS.
MRI reveals multiple, predominantly periventricular plaques; however, normal MRI cannot be used to exclude MS. MRI of the cervical spine can also be helpful.
MRI of the cervical spine can also be helpful.Labs
 LP for all first relapses when the dx of MS is not definite. Possible CSF abnlities include ↑ protein and mononuclear WBCs (both usually only mild). CSF IgG index and (+) oligoclonal bands are seen in 70% and 90%, respectively, of clinically definite MS cases. False(+) results occur w/IgG index in CNS infections and inflammation but rarely w/oligoclonal bands.
LP for all first relapses when the dx of MS is not definite. Possible CSF abnlities include ↑ protein and mononuclear WBCs (both usually only mild). CSF IgG index and (+) oligoclonal bands are seen in 70% and 90%, respectively, of clinically definite MS cases. False(+) results occur w/IgG index in CNS infections and inflammation but rarely w/oligoclonal bands. Serum: CBC, ESR, CRP, CHEM 7, LFTs, ANA, vitamin B12, Lyme titer, TSH
Serum: CBC, ESR, CRP, CHEM 7, LFTs, ANA, vitamin B12, Lyme titer, TSHTreatment
Acute General Rx
 Relapses: high-dose IV methylprednisolone (3-5 days of 1 g/day; alternative dose is 15 mg/kg/day), often followed by a 7- to 10-day prednisone taper. No evidence suggests that high-dose corticosteroids alter the long-term course of disease.
Relapses: high-dose IV methylprednisolone (3-5 days of 1 g/day; alternative dose is 15 mg/kg/day), often followed by a 7- to 10-day prednisone taper. No evidence suggests that high-dose corticosteroids alter the long-term course of disease. If pt has marked acute disability and acute corticosteroid therapy has failed, plasma exchange (5 to 7 exchanges on alternate days) have shown benefit.
If pt has marked acute disability and acute corticosteroid therapy has failed, plasma exchange (5 to 7 exchanges on alternate days) have shown benefit.Chronic Treatment
 Disease-modifying therapy: includes interferon-β1a, interferon-β1b, and glatiramer acetate. Interferons require routine CBC and LFT checks (initially in 1 mo, q3mo thereafter), occasionally TSH. None are needed with glatiramer acetate. Interferons can frequently cause flulike symptoms.
Disease-modifying therapy: includes interferon-β1a, interferon-β1b, and glatiramer acetate. Interferons require routine CBC and LFT checks (initially in 1 mo, q3mo thereafter), occasionally TSH. None are needed with glatiramer acetate. Interferons can frequently cause flulike symptoms. Fingolimod, a sphingosine-1-phosphate receptor modulator, is approved as the first oral disease-modifying agent. Common side effects are liver toxicity, bradycardia with the first dose only, and pancytopenia. Its use may be reasonable in pts who cannot tolerate or do not benefit from alternative disease-modifying therapies and in those who have had one or more relapses or new white-matter lesions on MRI within the past year.
Fingolimod, a sphingosine-1-phosphate receptor modulator, is approved as the first oral disease-modifying agent. Common side effects are liver toxicity, bradycardia with the first dose only, and pancytopenia. Its use may be reasonable in pts who cannot tolerate or do not benefit from alternative disease-modifying therapies and in those who have had one or more relapses or new white-matter lesions on MRI within the past year. Dalfampridine is a potassium channel blocker approved to improve walking speed in patients with MS.
Dalfampridine is a potassium channel blocker approved to improve walking speed in patients with MS. Cytotoxic: Methotrexate or azathioprine is occasionally used in RRMS or PPMS. Consider cyclophosphamide or mitoxantrone (causes dose-dependent cardiotoxicity) for frequent relapses with significant disability progression and for early secondary progressive MS. Emerging potential agents with long-term immunosuppressive effects include cladribine, alemtuzumab, daclizumab, laquinimod, and teriflunomide.
Cytotoxic: Methotrexate or azathioprine is occasionally used in RRMS or PPMS. Consider cyclophosphamide or mitoxantrone (causes dose-dependent cardiotoxicity) for frequent relapses with significant disability progression and for early secondary progressive MS. Emerging potential agents with long-term immunosuppressive effects include cladribine, alemtuzumab, daclizumab, laquinimod, and teriflunomide. Monoclonal antibodies: Natalizumab is approved for treatment of RRMS in the form of monthly infusions. It has been associated with an increased risk of developing progressive multifocal leukoencephalopathy (rare and fatal brain infection). Pts taking natalizumab must enter into a registry for monitoring.
Monoclonal antibodies: Natalizumab is approved for treatment of RRMS in the form of monthly infusions. It has been associated with an increased risk of developing progressive multifocal leukoencephalopathy (rare and fatal brain infection). Pts taking natalizumab must enter into a registry for monitoring. Spasticity: Onabotulinum toxin type A injection is FDA approved as first-line therapy for upper limb spasticity. Baclofen, tizanidine, dantrolene diazepam, lorazepam, and intrathecal baclofen are other alternatives.
Spasticity: Onabotulinum toxin type A injection is FDA approved as first-line therapy for upper limb spasticity. Baclofen, tizanidine, dantrolene diazepam, lorazepam, and intrathecal baclofen are other alternatives. Pain: carbamazepine, gabapentin, or amitriptyline
Pain: carbamazepine, gabapentin, or amitriptyline Spastic bladder: oxybutynin, tolterodine, or propantheline; prazosin for spastic sphincter
Spastic bladder: oxybutynin, tolterodine, or propantheline; prazosin for spastic sphincter Fatigue: Consider amantadine 100 mg bid, modafinil (most effective for somnolence), or fluoxetine.
Fatigue: Consider amantadine 100 mg bid, modafinil (most effective for somnolence), or fluoxetine. Tremor: clonazepam, carbamazepine, propranolol, or gabapentin. Wrist splints may be helpful.
Tremor: clonazepam, carbamazepine, propranolol, or gabapentin. Wrist splints may be helpful.H. Disorders of the Spinal Cord
1. Compressive Myopathies
 Spinal cord compression is the neurologic loss of spine function. Lesions may be complete or incomplete and develop gradually or acutely. Incomplete lesions often are manifested as distinct syndromes, as follows:
Spinal cord compression is the neurologic loss of spine function. Lesions may be complete or incomplete and develop gradually or acutely. Incomplete lesions often are manifested as distinct syndromes, as follows:Etiology
 Trauma
Trauma Tumor
Tumor Infection
Infection Inflammatory processes
Inflammatory processes Degenerative disk conditions w/spinal stenosis
Degenerative disk conditions w/spinal stenosis Acute disk herniation
Acute disk herniation Cystic abnlities
Cystic abnlitiesDiagnosis
H&P
 Clinical features reflect the amount of spinal cord involvement:
Clinical features reflect the amount of spinal cord involvement: Central cord syndrome: variable quadriparesis, w/UEs more severely involved than the LEs; some sensory sparing
Central cord syndrome: variable quadriparesis, w/UEs more severely involved than the LEs; some sensory sparing Anterior cord syndrome: motor, pain, and temperature loss below the lesion
Anterior cord syndrome: motor, pain, and temperature loss below the lesion Brown-Séquard syndrome
Brown-Séquard syndrome Conus medullaris syndrome: variable motor loss in the LEs w/loss of bowel and bladder function
Conus medullaris syndrome: variable motor loss in the LEs w/loss of bowel and bladder function Cauda equina syndrome: typical low back pain, weakness in both LEs, saddle anesthesia, and loss of voluntary bladder and bowel control
Cauda equina syndrome: typical low back pain, weakness in both LEs, saddle anesthesia, and loss of voluntary bladder and bowel controlImaging
 MRI
MRITreatment
 Urgent surgical decompression
Urgent surgical decompression2. Infectious Myopathies
 HIV infection
HIV infection Viral myositis
Viral myositis Trichinosis
Trichinosis Toxoplasmosis
Toxoplasmosis Cysticercosis
Cysticercosis Bacterial infections
Bacterial infections3. Inflammatory Myopathies
 SLE, RA
SLE, RA Sarcoidosis
Sarcoidosis Paraneoplastic syndrome
Paraneoplastic syndrome Polymyositis, dermatomyositis
Polymyositis, dermatomyositis Polyarteritis nodosa
Polyarteritis nodosa MCTD
MCTD Scleroderma
Scleroderma Inclusion body myositis
Inclusion body myositis Sjögren’s syndrome
Sjögren’s syndrome Cimetidine, D-penicillamine
Cimetidine, D-penicillamine4. Endocrine-Related Myopathies
Corticosteroid-Induced Myopathy
 Proximal limb weakness (mostly legs) in chronic corticosteroid pts
Proximal limb weakness (mostly legs) in chronic corticosteroid ptsDemographics
 Women affected ×2 as men
Women affected ×2 as men ↑ Risk use high-dose (≥30 mg/day) prednisone
↑ Risk use high-dose (≥30 mg/day) prednisoneDiagnosis
 Cushingoid body habitus
Cushingoid body habitus Neurologic exam: intact ocular, facial, distal extremity strength; nl sensory exam and DTRs
Neurologic exam: intact ocular, facial, distal extremity strength; nl sensory exam and DTRs Labs: serum CK and EMG results nl (↑ CK or abnl EMG suggests recurrence of partly Rx myositis or another myopathy)
Labs: serum CK and EMG results nl (↑ CK or abnl EMG suggests recurrence of partly Rx myositis or another myopathy) Muscle biopsy: non-dx, only shows atrophy type IIb muscle fibers
Muscle biopsy: non-dx, only shows atrophy type IIb muscle fibersTreatment
 Slow tapering of corticosteroid Rx with discontinuation
Slow tapering of corticosteroid Rx with discontinuationThyrotoxic Myopathy
 Symmetric muscle weakness in pts with classic hyperthyroidism or hypothyroidism
Symmetric muscle weakness in pts with classic hyperthyroidism or hypothyroidismClinical and Presentation and Treatment
Toxic Myopathies
 Clinical presentation of proximal muscle weakness, myalgia, and cramps should prompt review of current medications (statins) as a recent ↑ dosage, switch, or addition can ↑ myopathy risk.
Clinical presentation of proximal muscle weakness, myalgia, and cramps should prompt review of current medications (statins) as a recent ↑ dosage, switch, or addition can ↑ myopathy risk. Concomitant use of drugs that inhibit CYP3A4 (macrolides, cyclosporine, itraconazole, protease inhibitors) will ↑ risk myopathies in pts taking lovastatin, simvastatin, atorvastatin. In these pts, pravastatin, rosuvastatin, or fluvastatin (differently metabolized) may be preferable.
Concomitant use of drugs that inhibit CYP3A4 (macrolides, cyclosporine, itraconazole, protease inhibitors) will ↑ risk myopathies in pts taking lovastatin, simvastatin, atorvastatin. In these pts, pravastatin, rosuvastatin, or fluvastatin (differently metabolized) may be preferable.5. Idiopathic Transverse Myelitis
Etiology
 Demyelination due to the body’s immune response to infection, post-vaccination, may be onset of multiple sclerosis (MS), or may be idiopathic (15%30% of cases).
Demyelination due to the body’s immune response to infection, post-vaccination, may be onset of multiple sclerosis (MS), or may be idiopathic (15%30% of cases).Diagnosis
 Transverse myelitis should be suspected in pts with a hx of rapid (hr to days) onset of motor weakness, sensory abnlities referable to the spinal cord, and bladder or bowel dysfunction. The dysfunction is bilateral (not necessarily symmetric) and there is a clearly defined sensory level.
Transverse myelitis should be suspected in pts with a hx of rapid (hr to days) onset of motor weakness, sensory abnlities referable to the spinal cord, and bladder or bowel dysfunction. The dysfunction is bilateral (not necessarily symmetric) and there is a clearly defined sensory level. LP looking for oligoclonal bands for MS or infection
LP looking for oligoclonal bands for MS or infection MRI of brain and MRI of spine at level of suspected involvement
MRI of brain and MRI of spine at level of suspected involvementH&P
 The clinical signs are caused by an interruption in ascending and descending neuroanatomic pathways in the transverse plane of the spinal cord and a resulting sensory level is characteristic of transverse myelitis.
The clinical signs are caused by an interruption in ascending and descending neuroanatomic pathways in the transverse plane of the spinal cord and a resulting sensory level is characteristic of transverse myelitis. Rapid onset of symmetric or asymmetric paraparesis or paraplegia of the lower extremities over a few days, ascending paresthesia, trunk sensory level, back pain, sphincter dysfunction, and (+) Babinski with upgoing toes bilaterally. The arms may also be involved but < the legs in most cases.
Rapid onset of symmetric or asymmetric paraparesis or paraplegia of the lower extremities over a few days, ascending paresthesia, trunk sensory level, back pain, sphincter dysfunction, and (+) Babinski with upgoing toes bilaterally. The arms may also be involved but < the legs in most cases. One third to one half of pts present with localizing back pain.
One third to one half of pts present with localizing back pain. There is progression to nadir of clinical deficits between 4 hr and 21 days after symptom onset.
There is progression to nadir of clinical deficits between 4 hr and 21 days after symptom onset.Labs
 CSF: ↑ protein/nl protein, lymphocytes, and nl glucose
CSF: ↑ protein/nl protein, lymphocytes, and nl glucose Serum NMO-IgG to w/up neuromyelitis optica, which should be ruled out.
Serum NMO-IgG to w/up neuromyelitis optica, which should be ruled out. Oligoclonal bands should be absent in CSF in transverse myelitis and (+) in MS.
Oligoclonal bands should be absent in CSF in transverse myelitis and (+) in MS. Liver enzymes may help to differentiate if it is postinfectious transverse myelitis versus MS.
Liver enzymes may help to differentiate if it is postinfectious transverse myelitis versus MS. Consider autoimmune w/up for lupus.
Consider autoimmune w/up for lupus.Treatment
 High-dose IV corticosteroid (e.g., methylprednisolone 1000 mg/day for 3-5 days)
High-dose IV corticosteroid (e.g., methylprednisolone 1000 mg/day for 3-5 days) Rescue Rx with plasma exchange may be helpful in pts who do not respond to corticosteroids.
Rescue Rx with plasma exchange may be helpful in pts who do not respond to corticosteroids. Combination Rx with plasmapheresis and immunosuppressive agents (e.g., cyclophosphamide) may also be effective.
Combination Rx with plasmapheresis and immunosuppressive agents (e.g., cyclophosphamide) may also be effective. Naproxen, ibuprofen for pain
Naproxen, ibuprofen for painI. Peripheral Neuropathies
1. General Approach
2. Mononeuropathies
a. Carpal Tunnel Syndrome
Diagnosis
 Pain, paresthesia in the first, second, and third fingers and the lateral half of the fourth finger, worse at night
Pain, paresthesia in the first, second, and third fingers and the lateral half of the fourth finger, worse at night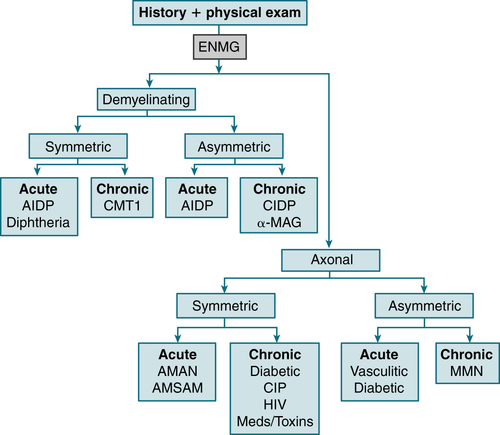
FIGURE 10-4 A systematic approach to evaluate neuropathy. The diseases listed are examples of neuropathies associated with specific neurophysiologic and clinical findings. Diabetic distal, predominantly sensory neuropathies are manifested as chronic axonal neuropathies; acute asymmetric neuropathies can also occur with diabetes. Most neuropathies caused by toxins or by side effects of medication are chronic, symmetric axonal neuropathies. Acute inflammatory demyelinating polyradiculoneuropathy (AIDP), acute motor axonal neuropathy (AMAN), and acute motor and sensory axonal neuropathy (AMSAN) are subtypes of Guillain-Barré syndrome. These and other examples are discussed in more detail in the text. CIDP, chronic inflammatory polyradiculoneuropathy; CIP, chronic illness polyneuropathy; CMT1, Charcot-Marie-Tooth disease type 1, a genetic disorder; ENMG, electroneuromyography; HIV, human immunodeficiency virus–related neuropathy; α−MAG, anti–myelin-associated glycoprotein; MMN, multifocal motor neuropathy. (From Goldman L, Schafer AI [eds]: Goldman’s Cecil Medicine, 24th ed. Philadelphia, Saunders, 2012.)
 Tinel’s sign at wrist: Tapping lightly over the median nerve on the volar surface of the wrist produces a tingling sensation radiating from the wrist to the hand.
Tinel’s sign at wrist: Tapping lightly over the median nerve on the volar surface of the wrist produces a tingling sensation radiating from the wrist to the hand. Phalen’s sign: reproduction of sx after 1 min of gentle, unforced wrist flexion
Phalen’s sign: reproduction of sx after 1 min of gentle, unforced wrist flexion EMG: impaired sensory conduction across the carpal tunnel
EMG: impaired sensory conduction across the carpal tunnelTreatment
 Activity modification
Activity modification Nocturnal wrist splint
Nocturnal wrist splint Corticosteroid injection of carpal canal on ulnar side of palmaris longus tendon proximal to wrist crease
Corticosteroid injection of carpal canal on ulnar side of palmaris longus tendon proximal to wrist crease Short-term benefit from U/S Rx
Short-term benefit from U/S Rx Ergonomic keyboards (vs standard keyboards)
Ergonomic keyboards (vs standard keyboards) Surgery in refractory cases
Surgery in refractory casesb. Bell’s Palsy
Etiology
 HSV is thought to be the most common viral pathogen, followed by herpes zoster.
HSV is thought to be the most common viral pathogen, followed by herpes zoster.Diagnosis
 Onset is usually acute to subacute over hours of unilateral facial paralysis with maximal weakness at 3 wk. One third of pts demonstrate incomplete paralysis, whereas the remaining two thirds have complete paralysis. Recovery is present within the first 6 mo.
Onset is usually acute to subacute over hours of unilateral facial paralysis with maximal weakness at 3 wk. One third of pts demonstrate incomplete paralysis, whereas the remaining two thirds have complete paralysis. Recovery is present within the first 6 mo.Treatment
 Glucocorticoid Rx: prednisone 60 to 80 mg/day for 1 wk
Glucocorticoid Rx: prednisone 60 to 80 mg/day for 1 wkDisposition
 71% of pts: complete recovery
71% of pts: complete recovery Recurrence rate is 7%. Average time to recurrence is 10 yr.
Recurrence rate is 7%. Average time to recurrence is 10 yr.3. Polyneuropathies
a. Diabetic Neuropathy
Diagnosis
 EMG can be helpful in confirming the presence, extent, and severity of neuropathy.
EMG can be helpful in confirming the presence, extent, and severity of neuropathy.H&P
 Distal symmetric polyneuropathy (DSPN)
Distal symmetric polyneuropathy (DSPN) Autonomic neuropathy
Autonomic neuropathy Regional diabetic polyneuropathy
Regional diabetic polyneuropathy Focal diabetic neuropathy
Focal diabetic neuropathyTreatment
 Topical agents: Lidocaine 5% patch can be applied to painful areas for 12 hr a day.
Topical agents: Lidocaine 5% patch can be applied to painful areas for 12 hr a day. Anticonvulsants: gabapentin (100-1200 mg tid) and pregabalin (50-100 mg tid)
Anticonvulsants: gabapentin (100-1200 mg tid) and pregabalin (50-100 mg tid) Antidepressants: amitriptyline (10-100 mg qhs), nortriptyline (25-150 mg qhs), and duloxetine (60-120 mg daily)
Antidepressants: amitriptyline (10-100 mg qhs), nortriptyline (25-150 mg qhs), and duloxetine (60-120 mg daily)b. Charcot-Marie-Tooth Disease (CMT)
Diagnosis
 Symmetric, slowly progressive distal motor neuropathy resulting in weakness and atrophy in legs, often progresses to involve hands
Symmetric, slowly progressive distal motor neuropathy resulting in weakness and atrophy in legs, often progresses to involve hands High-arched feet (pes cavus), claw toe deformities, and hammer toes
High-arched feet (pes cavus), claw toe deformities, and hammer toes Atrophy of the lower legs producing a storklike appearance (muscle wasting does not involve the upper legs)
Atrophy of the lower legs producing a storklike appearance (muscle wasting does not involve the upper legs) ↓ Proprioception and weakness of ankle dorsiflexors often interfere with balance and gait (steppage gait)
↓ Proprioception and weakness of ankle dorsiflexors often interfere with balance and gait (steppage gait)Treatment
 Symptomatic and supportive care is managed by a multidisciplinary team including physical and occupational Rx.
Symptomatic and supportive care is managed by a multidisciplinary team including physical and occupational Rx. Musculoskeletal pain may respond to acetaminophen or NSAIDs; neuropathic pain may respond to tricyclic antidepressants or drugs such as carbamazepine or gabapentin.
Musculoskeletal pain may respond to acetaminophen or NSAIDs; neuropathic pain may respond to tricyclic antidepressants or drugs such as carbamazepine or gabapentin. Occasionally, orthopedic surgery is required to correct severe pes cavus deformity or hip dysplasia.
Occasionally, orthopedic surgery is required to correct severe pes cavus deformity or hip dysplasia.c. Guillain-Barré Syndrome (GBS)
Etiology
 Most pts give h/o respiratory (mycoplasma)/GI illness (Campylobacter jejuni) within 30 days of neurologic sx onset.
Most pts give h/o respiratory (mycoplasma)/GI illness (Campylobacter jejuni) within 30 days of neurologic sx onset.Diagnosis
History
 Rapid progression of acute symmetric progressive weakness, usually > distally than proximally and > in the legs than in the arms
Rapid progression of acute symmetric progressive weakness, usually > distally than proximally and > in the legs than in the arms The pt often reports difficulty in ambulating, getting up from a chair, or climbing stairs.
The pt often reports difficulty in ambulating, getting up from a chair, or climbing stairs. The ascending paralysis affects motor nerves more than sensory nerves. Sensory loss (predominantly position and vibration senses) is variable but usually mild.
The ascending paralysis affects motor nerves more than sensory nerves. Sensory loss (predominantly position and vibration senses) is variable but usually mild. In some pts, the initial manifestations may involve the cranial musculature or the UEs (e.g., tingling of the hands).
In some pts, the initial manifestations may involve the cranial musculature or the UEs (e.g., tingling of the hands). As a general rule, weakness reaches its max within 14 days.
As a general rule, weakness reaches its max within 14 days.Physical Exam
 Symmetric weakness, initially involving proximal muscles, subsequently both proximal and distal muscles
Symmetric weakness, initially involving proximal muscles, subsequently both proximal and distal muscles ↓ Or absent reflexes bilaterally early in the disease
↓ Or absent reflexes bilaterally early in the disease Minimum to moderate glove and stocking anesthesia
Minimum to moderate glove and stocking anesthesia Ataxia and pain in a segmental distribution possible in some pts (caused by involvement of posterior nerve roots)
Ataxia and pain in a segmental distribution possible in some pts (caused by involvement of posterior nerve roots) Autonomic abnlities (bradycardia or tachycardia, hypotension or HTN) also possible
Autonomic abnlities (bradycardia or tachycardia, hypotension or HTN) also possible Respiratory insufficiency (caused by weakness of intercostal muscles)
Respiratory insufficiency (caused by weakness of intercostal muscles) Facial paresis, difficulty swallowing (secondary to cranial nerve involvement)
Facial paresis, difficulty swallowing (secondary to cranial nerve involvement)Labs
 LP: Typical findings include ↑ CSF protein (especially IgG) and presence of few mononuclear leukocytes (albuminocytologic dissociation).
LP: Typical findings include ↑ CSF protein (especially IgG) and presence of few mononuclear leukocytes (albuminocytologic dissociation).EMG/NCS
 Slowed conduction velocities; motor, sensory, and F wave latencies. EMG may be nl in first 7 to 10 days.
Slowed conduction velocities; motor, sensory, and F wave latencies. EMG may be nl in first 7 to 10 days.Treatment
 Close monitoring of respiratory function (frequent [q1h initially] bedside measurements of FVC and (−) inspiratory force to assess pulmonary muscle strength) because respiratory failure is the major potential problem in GBS.
Close monitoring of respiratory function (frequent [q1h initially] bedside measurements of FVC and (−) inspiratory force to assess pulmonary muscle strength) because respiratory failure is the major potential problem in GBS. Infusion of IVIG (0.4 g/kg/day for 5 days). Always check serum IgA levels before infusion to prevent anaphylaxis in deficient pts.
Infusion of IVIG (0.4 g/kg/day for 5 days). Always check serum IgA levels before infusion to prevent anaphylaxis in deficient pts. Plasma exchange: 200 to 250 mL/kg during five sessions qod
Plasma exchange: 200 to 250 mL/kg during five sessions qod IVIG and plasma exchange are equally effective. The selection of one or the other is determined by availability and risk of particular complications. For example, plasma exchange should be avoided in pts w/prominent autonomic dysfunction.
IVIG and plasma exchange are equally effective. The selection of one or the other is determined by availability and risk of particular complications. For example, plasma exchange should be avoided in pts w/prominent autonomic dysfunction. There is no proven benefit of combining IVIG and plasma exchange.
There is no proven benefit of combining IVIG and plasma exchange. Ventilatory support may be necessary in 10% to 20% of pts. Adequate fluid/electrolyte support and nutrition are necessary, especially in pts w/dysautonomia or bulbar dysfunction.
Ventilatory support may be necessary in 10% to 20% of pts. Adequate fluid/electrolyte support and nutrition are necessary, especially in pts w/dysautonomia or bulbar dysfunction. Aggressive nursing care is required to prevent decubitus ulcers, infections, fecal impactions, and pressure nerve palsies and for mouth care to prevent ventilator-associated pneumonias.
Aggressive nursing care is required to prevent decubitus ulcers, infections, fecal impactions, and pressure nerve palsies and for mouth care to prevent ventilator-associated pneumonias. Monitor and treat autonomic dysfunction (bradyarrhythmias or tachyarrhythmias, orthostatic hypotension, systemic HTN, altered sweating).
Monitor and treat autonomic dysfunction (bradyarrhythmias or tachyarrhythmias, orthostatic hypotension, systemic HTN, altered sweating). Treat back pain and dysesthesia w/low-dose tricyclic antidepressants, gabapentin, and the like. Opiate narcotics can be used cautiously in the short term but may compound dysautonomia.
Treat back pain and dysesthesia w/low-dose tricyclic antidepressants, gabapentin, and the like. Opiate narcotics can be used cautiously in the short term but may compound dysautonomia. DVT prophylaxis
DVT prophylaxisd. Chronic Inflammatory Demyelinating Polyneuropathy (CIDP)
Diagnosis
 NCS: features of demyelination including prolonged distal latencies and F-waves, slowed velocities, and at least one nerve demonstrating partial conduction block (feature of acquired demyelination)
NCS: features of demyelination including prolonged distal latencies and F-waves, slowed velocities, and at least one nerve demonstrating partial conduction block (feature of acquired demyelination)H&P
 Characterized by occurrence of symmetric weakness in both proximal and distal muscles that progressively ↑ over 2 mo
Characterized by occurrence of symmetric weakness in both proximal and distal muscles that progressively ↑ over 2 mo Associated with impaired sensation, postural instability, ↓ or absent DTRs, and variable craniofacial-bulbar involvement
Associated with impaired sensation, postural instability, ↓ or absent DTRs, and variable craniofacial-bulbar involvementLabs
 CSF analysis to assess for albumin-cytologic dissociation (i.e., ↑ protein with nl cell count), along with appropriate laboratory studies to exclude associated conditions
CSF analysis to assess for albumin-cytologic dissociation (i.e., ↑ protein with nl cell count), along with appropriate laboratory studies to exclude associated conditionsTreatment
 IVIG, plasmapheresis/plasma exchange, and corticosteroids. There is no difference in efficacy among these three modalities of Rx.
IVIG, plasmapheresis/plasma exchange, and corticosteroids. There is no difference in efficacy among these three modalities of Rx. Azathioprine, mycophenolate mofetil, cyclophosphamide, rituximab, and cyclosporine may be used as secondary agents.
Azathioprine, mycophenolate mofetil, cyclophosphamide, rituximab, and cyclosporine may be used as secondary agents.J. Amyotrophic Lateral Sclerosis (ALS)
Etiology
 90% to 95% sporadic
90% to 95% sporadic Of the familial cases, 10% to 20% associated w/genetic defect in copper-zinc superoxide dismutase enzyme
Of the familial cases, 10% to 20% associated w/genetic defect in copper-zinc superoxide dismutase enzymeDiagnosis
 EMG and NCS (El Escorial criteria)
EMG and NCS (El Escorial criteria) Assessment of respiratory function (forced vital capacity [FVC], [−] inspiratory force)
Assessment of respiratory function (forced vital capacity [FVC], [−] inspiratory force)H&P
 LMN signs: weakness, hypotonia, wasting, fasciculations, hyporeflexia or areflexia
LMN signs: weakness, hypotonia, wasting, fasciculations, hyporeflexia or areflexia UMN signs: loss of fine motor dexterity, spasticity, extensor plantar responses, hyperreflexia, clonus
UMN signs: loss of fine motor dexterity, spasticity, extensor plantar responses, hyperreflexia, clonus Preservation of extraocular movements, sensation, bowel and bladder function
Preservation of extraocular movements, sensation, bowel and bladder function Dysarthria, dysphagia, pseudobulbar affect, frontal lobe dysfunction
Dysarthria, dysphagia, pseudobulbar affect, frontal lobe dysfunction Respiratory insufficiency, typically late in the disease
Respiratory insufficiency, typically late in the disease ALS comprises approximately 90% of adult-onset motor neuron diseases. Other presentations of motor neuron disease include progressive muscular atrophy, primary lateral sclerosis, progressive bulbar palsy, progressive pseudobulbar palsy, and ALS-parkinsonism-dementia complex.
ALS comprises approximately 90% of adult-onset motor neuron diseases. Other presentations of motor neuron disease include progressive muscular atrophy, primary lateral sclerosis, progressive bulbar palsy, progressive pseudobulbar palsy, and ALS-parkinsonism-dementia complex.Labs
 Vitamin B12, thyroid function, parathyroid hormone, HIV may be considered.
Vitamin B12, thyroid function, parathyroid hormone, HIV may be considered. Serum protein and immunofixation electrophoresis
Serum protein and immunofixation electrophoresis DNA studies for SMA or bulbospinal atrophy, hexosaminidase levels in pure LMN syndrome
DNA studies for SMA or bulbospinal atrophy, hexosaminidase levels in pure LMN syndrome 24-hour urine for heavy metals if indicated
24-hour urine for heavy metals if indicatedImaging
 MRI to r/o brain and spinal cord disorders
MRI to r/o brain and spinal cord disorders Modified barium swallow to evaluate aspiration risk
Modified barium swallow to evaluate aspiration riskTreatment
 PEG tube placement improves nutritional intake, promotes weight stabilization, and eases medication administration.
PEG tube placement improves nutritional intake, promotes weight stabilization, and eases medication administration. Nutrition, speech Rx, physical and occupational Rx services are indicated.
Nutrition, speech Rx, physical and occupational Rx services are indicated. Suction device is used for sialorrhea.
Suction device is used for sialorrhea. Communication may be eased with computerized assistive devices.
Communication may be eased with computerized assistive devices. Early discussion should cover living will, resuscitation orders, desire for PEG and tracheostomy, potential long-term care options.
Early discussion should cover living will, resuscitation orders, desire for PEG and tracheostomy, potential long-term care options. Riluzole, a glutamate antagonist, is the only FDA-approved medication known to extend tracheostomy-free survival in pts with ALS.
Riluzole, a glutamate antagonist, is the only FDA-approved medication known to extend tracheostomy-free survival in pts with ALS. Spasticity may be treated pharmacologically with baclofen, tizanidine, clonazepam.
Spasticity may be treated pharmacologically with baclofen, tizanidine, clonazepam. Pseudobulbar affect may improve with amitriptyline, sertraline, or dextromethorphan/quinine.
Pseudobulbar affect may improve with amitriptyline, sertraline, or dextromethorphan/quinine.Disposition
 Mean duration of sx is 3 to 5 yr.
Mean duration of sx is 3 to 5 yr. Approximately 20% of pts survive >5 yr.
Approximately 20% of pts survive >5 yr.K. Neuromuscular Junction Disorders
1. Myasthenia Gravis (MG)
Diagnosis
H&P
 The hallmark of MG is weakness made worse w/exercise and improved by rest. Sx fluctuate and are often better in the morning.
The hallmark of MG is weakness made worse w/exercise and improved by rest. Sx fluctuate and are often better in the morning. >50% of pts present initially w/ptosis, ocular muscle weakness, or both.
>50% of pts present initially w/ptosis, ocular muscle weakness, or both. Pts have difficulty in chewing, abnl smile, dysarthria, dysphagia.
Pts have difficulty in chewing, abnl smile, dysarthria, dysphagia. Involvement of the respiratory muscles may require intubation and assisted ventilation.
Involvement of the respiratory muscles may require intubation and assisted ventilation. Pain may occur in fatigued muscles (e.g., neck muscles).
Pain may occur in fatigued muscles (e.g., neck muscles). Clinical manifestations reproducible w/exercise. Observation of the pt performing repetitive muscle contractions of involved muscles will demonstrate rapidly developing weakness.
Clinical manifestations reproducible w/exercise. Observation of the pt performing repetitive muscle contractions of involved muscles will demonstrate rapidly developing weakness. PE may be nl at rest.
PE may be nl at rest. Pts w/h/o ptosis will demonstrate fatigue weakness and ptosis when asked to sustain upward gaze for >3 min w/o interruption.
Pts w/h/o ptosis will demonstrate fatigue weakness and ptosis when asked to sustain upward gaze for >3 min w/o interruption.Labs and Other Tests
 Edrophonium test: improvement of sx after use of anticholinesterase medications (edrophonium)
Edrophonium test: improvement of sx after use of anticholinesterase medications (edrophonium) EMG: single-fiber electromyography: sensitivity >90 % but nonspecific
EMG: single-fiber electromyography: sensitivity >90 % but nonspecific MRI or CT of anterior mediastinum: thymoma found in 12%
MRI or CT of anterior mediastinum: thymoma found in 12% TSH: thyroid disease found in 30% of pts
TSH: thyroid disease found in 30% of pts Vitamin B12 level: r/o pernicious anemia
Vitamin B12 level: r/o pernicious anemia ANA, RF ( association w/SLE, RA)
ANA, RF ( association w/SLE, RA) (+ ) Ab against MuSK receptors
(+ ) Ab against MuSK receptorsTreatment
 Acetylcholinesterase inhibitors: Pyridostigmine is first-line Rx.
Acetylcholinesterase inhibitors: Pyridostigmine is first-line Rx. Immunosuppressants: corticosteroids, azathioprine, mycophenolate mofetil, rituximab for more severe or generalized disease
Immunosuppressants: corticosteroids, azathioprine, mycophenolate mofetil, rituximab for more severe or generalized disease Plasmapheresis and IVIG in refractory cases
Plasmapheresis and IVIG in refractory cases Thymectomy in thymomatous MG
Thymectomy in thymomatous MG2. Lambert-Eaton Myasthenic Syndrome
Diagnosis
H&P
 Weakness w/↓ or absent muscle stretch reflexes
Weakness w/↓ or absent muscle stretch reflexes Proximal LE muscles affected most
Proximal LE muscles affected most Transient strength improvement w/brief exercise
Transient strength improvement w/brief exercise Autonomic dysfunction common (dry mouth in 75%, sexual dysfunction, blurred vision, constipation, orthostasis)
Autonomic dysfunction common (dry mouth in 75%, sexual dysfunction, blurred vision, constipation, orthostasis)Treatment
 Acute: plasma exchange (200-250 mL/kg over 10-14 days) or IVIG (2 g/kg over 2-5 days)
Acute: plasma exchange (200-250 mL/kg over 10-14 days) or IVIG (2 g/kg over 2-5 days) Chronic Rx: anticholinesterase agents (pyridostigmine )
Chronic Rx: anticholinesterase agents (pyridostigmine )L. Head Injury
1. Epidural Hematoma
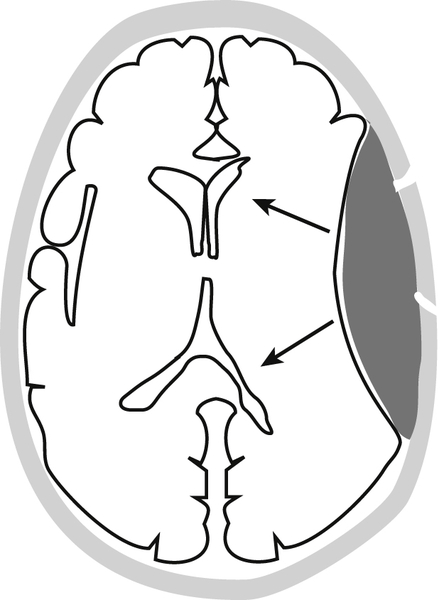
FIGURE 10-5 Epidural hematoma. The arrows show the pattern of brain displacement. (From Weissleder R, Wittenberg J, Harisinghani M, Chen JW [eds]: Primer of Diagnostic Imaging, 5th ed. St. Louis, Mosby, 2011.)
Etiology
 Head trauma causing temporal bone fracture resulting in middle meningeal artery tear
Head trauma causing temporal bone fracture resulting in middle meningeal artery tear Neoplasms that have spread into the epidural space
Neoplasms that have spread into the epidural spaceDiagnosis
H&P
 Lucid interval after the head trauma is followed by progressive reduction in the level of consciousness as the hematoma enlarges and the underlying brain is displaced inward.
Lucid interval after the head trauma is followed by progressive reduction in the level of consciousness as the hematoma enlarges and the underlying brain is displaced inward. The initial injury causes brain concussion and loss of consciousness from which the pt awakens and may have some headache but seems otherwise to have recovered.
The initial injury causes brain concussion and loss of consciousness from which the pt awakens and may have some headache but seems otherwise to have recovered. Downward transtentorial herniation may develop rapidly, causing third nerve compression and an ipsilateral hemiparesis.
Downward transtentorial herniation may develop rapidly, causing third nerve compression and an ipsilateral hemiparesis.Imaging
 Brain CT
Brain CTTreatment
 Emergency surgical evacuation
Emergency surgical evacuation2. Subdural Hematoma
Diagnosis
H&P
 Vague headache, often worse in morning than evening
Vague headache, often worse in morning than evening Some apathy, confusion, and clouding of consciousness is common, although frank coma may complicate late cases. Chronic subdural hematomas may cause a dementia picture.
Some apathy, confusion, and clouding of consciousness is common, although frank coma may complicate late cases. Chronic subdural hematomas may cause a dementia picture. Neurologic sx may be transient, simulating TIA.
Neurologic sx may be transient, simulating TIA. Almost any sign of cortical dysfunction may occur, including hemiparesis, sensory deficits, and language abnlities, depending on which part of the cortex is compressed by the hematoma.
Almost any sign of cortical dysfunction may occur, including hemiparesis, sensory deficits, and language abnlities, depending on which part of the cortex is compressed by the hematoma.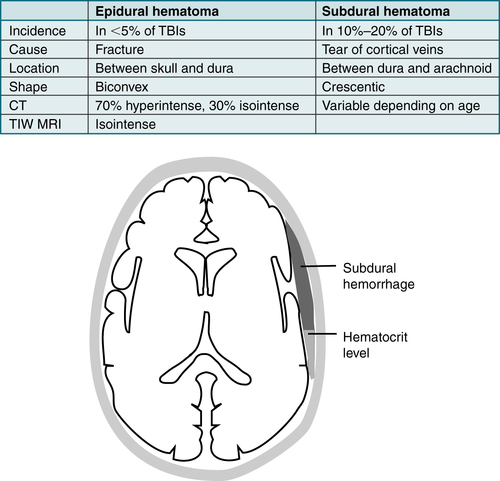
FIGURE 10-6 Subdural hematoma and comparison with epidural hematoma. (From Weissleder R, Wittenberg J, Harisinghani M, Chen JW [eds]: Primer of Diagnostic Imaging, 5th ed. St. Louis, Mosby, 2011.)
Labs
 Hct, Plt count, PTT, and PT/INR
Hct, Plt count, PTT, and PT/INRImaging
 CT of brain
CT of brainTreatment
 Small subdural hematomas may be left untreated and the pt observed; but if there is an underlying cause, such as anticoagulation, this should be rapidly corrected to prevent further accumulation of blood.
Small subdural hematomas may be left untreated and the pt observed; but if there is an underlying cause, such as anticoagulation, this should be rapidly corrected to prevent further accumulation of blood. Neurosurgical drainage of blood from subdural space through burr hole is the definitive procedure, although it is common for the hematoma to reaccumulate.
Neurosurgical drainage of blood from subdural space through burr hole is the definitive procedure, although it is common for the hematoma to reaccumulate.3. Concussion
 Complex pathophysiologic process affecting the brain. When traumatic biomechanical rotational/angular acceleration forces are applied to the brain, they cause shear strain of underlying neural elements. Although not required, it may be associated with direct trauma.
Complex pathophysiologic process affecting the brain. When traumatic biomechanical rotational/angular acceleration forces are applied to the brain, they cause shear strain of underlying neural elements. Although not required, it may be associated with direct trauma. Concussions typically result in rapid onset of a short-lived neurologic functional deficit that spontaneously resolves. Chronic injury may result in long-term neuropathologic changes.
Concussions typically result in rapid onset of a short-lived neurologic functional deficit that spontaneously resolves. Chronic injury may result in long-term neuropathologic changes. Concussion results in a graded set of clinical syndromes that may or may not involve loss of consciousness. Table 10-17 describes commonly used grading scales for concussion. Resolution of the clinical sx typically follows a sequential course. It is typically associated with grossly nl structural neuroimaging.
Concussion results in a graded set of clinical syndromes that may or may not involve loss of consciousness. Table 10-17 describes commonly used grading scales for concussion. Resolution of the clinical sx typically follows a sequential course. It is typically associated with grossly nl structural neuroimaging.Diagnosis
Workup
 Sideline assessment
Sideline assessment Neurocognitive testing
Neurocognitive testing Gait/balance testing with a tool such as the Balance Error Scoring System (BESS)
Gait/balance testing with a tool such as the Balance Error Scoring System (BESS)TABLE 10-17
Grading Scales for Concussion
| Scale | Grade of Concussion | ||
| I | II | III | |
| Colorado | Confusion; no LOC; PTA <30 min | LOC <5 min; confusion; PTA >30 min | LOC >5 min; PTA >24 h |
| Cantu | PTA <30 min; no LOC | LOC <5 min; PTA 30 min to 24 h | LOC >5 min; PTA >24 h |
| AAN | Transient confusion; symptoms <15 min; no LOC | No LOC; transient confusion; symptoms >15 min | Any LOC |
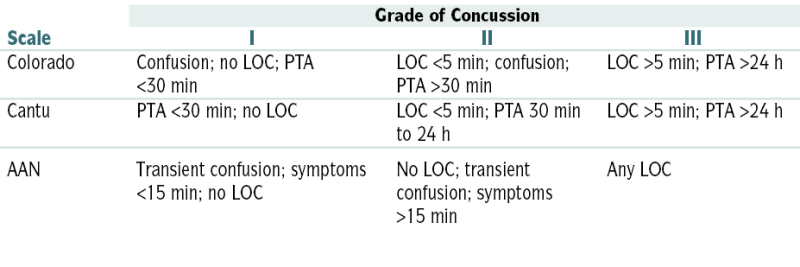
AAN, American Academy of Neurology; LOC, loss of consciousness; PTA, posttraumatic amnesia.
Modified from Vincent JL, Abraham E, Moore FA, et al (eds): Textbook of Critical Care, 6th ed. Philadelphia, Saunders, 2011.
 When used in combination, symptom assessment, balance assessment, and neurocognitive testing provide a sensitivity of >90% for the identification of concussion.
When used in combination, symptom assessment, balance assessment, and neurocognitive testing provide a sensitivity of >90% for the identification of concussion.Imaging
 Head CT or MRI for grade II or III concussion with persistent abnlities on exam or symptoms lasting >1 wk
Head CT or MRI for grade II or III concussion with persistent abnlities on exam or symptoms lasting >1 wkTreatment
 Immediate removal of athlete from game/athletic activity
Immediate removal of athlete from game/athletic activity Physical rest: no return to play until asymptomatic for atleast 24 hours
Physical rest: no return to play until asymptomatic for atleast 24 hours Cognitive rest to limit sx
Cognitive rest to limit sx