Chapter 3 Neurology
Neurology and neuromuscular disorders
Epilepsy
Affects 1/200 of the general population. Continue anticonvulsants perioperatively.
Anaesthetic problems
Multiple sclerosis (MS)
General anaesthesia does not exacerbate MS. Use normal doses of muscle relaxants.
Motor neurone disease
Regional anaesthesia. Avoid impairment of respiratory muscles but otherwise safe.
Autoimmune disease
Berrouschot J., Baumann I., Kalischewski P., et al. Therapy of myasthenic crisis. Crit Care Med. 1997;25:1228-1235.
Eriksson L.I. Neuromuscular disorders and anaesthesia. Curr Opin Anaesth. 1995;8:275-281.
Errington D.R., Severn A.M., Meara J. Parkinson’s disease. BJA CEPD Rev. 2002;2:69-73.
Kam P.C.A., Calcroft R.M. Perioperative stroke in general surgical patients. Anaesthesia. 1997;52:879-883.
Le Corre F., Plaud B. Neuromuscular disorders. Curr Opin Anaesth. 1998;11:333-337.
Nicholson G., Pereira A.C., Hall G.M. Parkinson’s disease and anaesthesia. Br J Anaesth. 2002;89:904-916.
Sneyd J.R. Propofol and epilepsy. Br J Anaesth. 1999;82:168-169.
Thavasothy M., Hirsch N. Myasthenia gravis. BJA CEPD Rev. 2002;2:88-90.
Neuroanaesthesia
Physiology
Intracranial pressure (ICP)
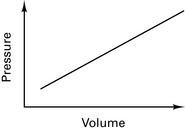
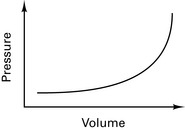
Munro–Kelly hypothesis (1852) stated that the contents of cranium are not compressible (60% water, 40% solid). Therefore, increasing the volume within the cranium causes a rapid increase in pressure (Fig. 3.1).
However, compression of veins and communication of CSF with spinal column result in a small range of compensation before pressure increases (Fig. 3.2).
Cushing reflex. Increased ICP causes hypertension and bradycardia.
Coning
Pressure waves in CSF (described by Lundberg in 1960)
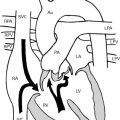
Cerebral circulation
Raised intrathoracic pressure increases CVP and reduces CPP further.
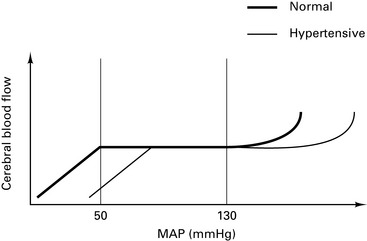
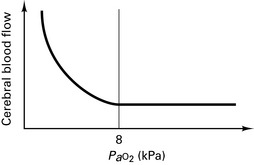
Normal brain autoregulates over a range of 50–130 mmHg (Fig. 3.3). Hypertension shifts the curve to the right. Autoregulation is lost with volatile anaesthetic agents, tumour, trauma, infarction, intracranial bleed, hypoxia, hypercarbia, seizure disorders, hypotension and hypertension. In these conditions, CBF ∝ MAP.
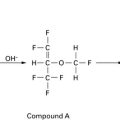
CO2
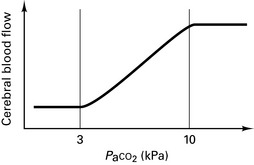
Affects CBF through vasodilation by changing the pH of extracellular fluid (ECF) (Fig. 3.4). Aim for a Paco2 of 3.5 kPa to lower ICP without excessive vasoconstriction and prevent ‘reverse steal’. Volatile agents increase effects of CO2 on vasodilation. A 3% change in CBF occurs for each 0.1 kPa change in Paco2.
Monitoring
Evoked potentials
Measure latency and amplitude.
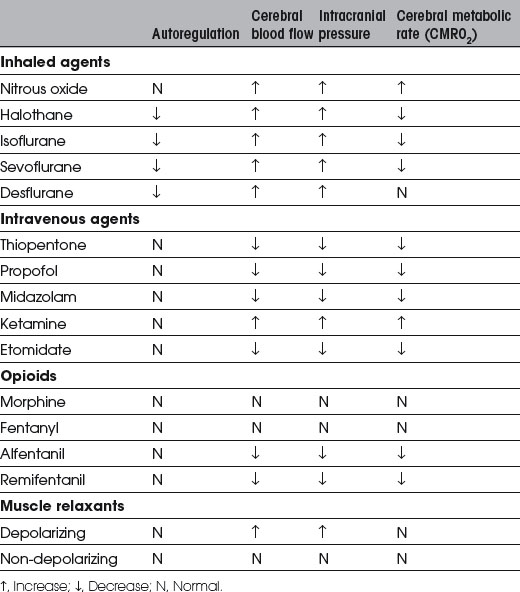
Anaesthetic drugs
Volatile agents
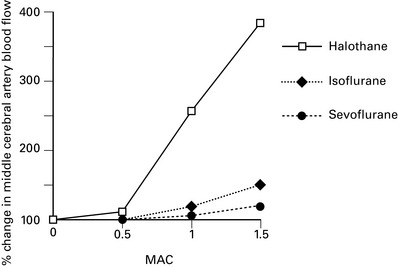
All volatiles with the exception of desflurane reduce cerebral metabolism and oxygen demand. Effect is most marked with isoflurane. All increase ICP and abolish autoregulation in sufficient doses. Halothane causes most cerebral vasodilation (Table 3.2). At 1 MAC (minimum alveolar concentration), isoflurane has minimal effect on ICP, autoregulation or EEG depression. At 2.5 MAC, the EEG becomes isoelectric. Isoflurane reduces cerebral O2 demand more than any other volatile and reduces cerebral blood flow without evidence of ischaemia. Sevoflurane and desflurane appear similar to isoflurane in their CNS and CVS effects.
Anaesthesia for neurosurgery
Fluids
Maintain plasma osmolality at the upper end of normal. Avoid fluids with low osmolality which increase free brain water (Table 3.3). Avoid glucose-containing solutions which accelerate anaerobic metabolism and may worsen neurological morbidity.
| Solution | Osmolality (mOsm.L−1) |
|---|---|
| Normal saline | 310 |
| Mannitol | 300 |
| Hartmann’s solution | 272 |
| Dextrose saline | 262 |
| 5% dextrose | 250 |
Treatment of raised ICP
Recommendations for the Safe Transfer of Patients with Brain Injury
Association of Anaesthetists of Great Britain and Ireland 2006
Summary
Association of Anaesthetists of Great Britain and Ireland. Recommedations for The Safe Transfer of Patients With brain injury. Reproduced with the kind permission of the Association of anaesthetists of Great Britain and Ireland, 2006.
Dinsmore J. Anaesthesia for elective neurosurgery. Br J Anaesth. 2007;99:68-74.
Hancock S.M., Nathanson M.H. Nitrous oxide or remifentanil for the ‘at risk’ brain. Anaesthesia. 2004;59:313-315.
Hirsch N. Advances in neuroanaesthesia. Anaesthesia. 2003;58:1162-1165.
Moss E. The cerebral circulation. BJA CEPD Rev. 2001;1:67-71.
Pasternak J.J., William L.W. Neuroanesthesiology update. J Neurosurg Anesth. 2009;21:73-97.
Autonomic Nervous System
Foëx P. The heart and autonomic nervous system. In: Nimmo W.S., Rowbotham D.J., Smith G., editors. Anaesthesia. ed 2. Oxford: Blackwell Scientific Publications; 1994:195-242.
Keyl C., Lemberger P., Palitzsch K.D., et al. Cardiovascular autonomic dysfunction and haemodynamic response to anesthetic induction in patients with coronary artery disease and diabetes mellitus. Anesth Analg. 1999;88:985-991.
Tusiewicz K. The autonomic nervous system. In: Kaufman L., editor. Anaesthesia Review 5. Edinburgh: Churchill Livingstone; 1988:54-66.

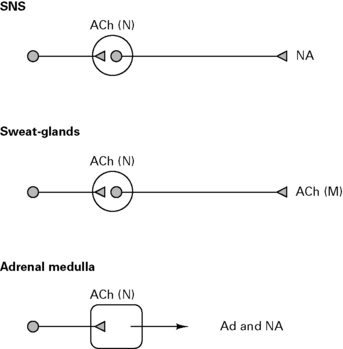
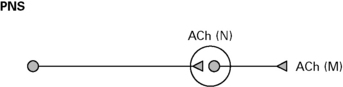
 , ganglia;
, ganglia;  , adrenal medulla.
, adrenal medulla.