Chapter 24 Neurological emergencies
COMA OR IMPAIRED CONSCIOUSNESS
Impaired consciousness is recognised and described by observation of response to sound, light, touch or painful stimulus. The Glasgow Coma Scale (GCS) gives a standard way of recording and monitoring the level of consciousness (see Chapter 15, ‘Neurosurgical emergencies’).
Examination
Investigations
EPILEPSY
Fits are usually self-limiting and no urgent drug treatment is needed. During fits:
After the fit, ask if there is a history of fits.
Prolonged fitting or frequent fitting (status epilepticus)
Partial seizures may be prolonged or frequently recurrent without major hazard.
Major generalised seizures lasting more than 5–10 minutes or recurring rapidly are life-threatening. This situation demands prompt and adequate IV drug therapy, monitoring and support.
Treatment
CEREBROVASCULAR DISEASE
Initial assessment and management of stroke
Investigations
Stroke management checklist
Thrombolytic therapy in stroke
Transient ischaemic attack (TIA)
Overall risk of stroke following TIA is around 8–10% at 1 week.
Hospital admission should be considered for TIA to avoid any delay in stroke prevention.
Intracerebral haemorrhage
Treatment
Treatment is as per stroke management check list with the following modifications:
HEADACHE
Important diagnoses to be considered:
Meningitis
Clinical features
Investigations
Treatment
Lumbar puncture (LP)
Indications
The major role for LP in the emergency department is the diagnosis of infection or bleeding within the central nervous system (refer to Chapter 3, ‘Resuscitation and emergency procedures’).
Preparation
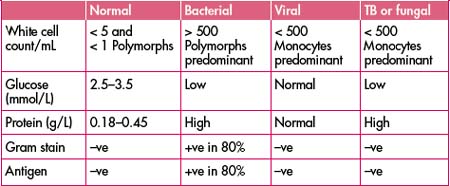
Interpretation of CSF findings
Encephalitis
Clinical features
There is overlap between meningitis and encephalitis.
Herpes simplex encephalitis demands early diagnosis as treatment is life-saving.
Immunocompromised patients can present with parasitic or fungal as well as viral infections, e.g. toxoplasmosis, cytomegalovirus, progressive multifocal leuco-encephalopathy.
Investigations
Subarachnoid haemorrhage (SAH)
(See also Chapter 15, ‘Neurosurgical emergencies’.)
Clinical features
SAH should be considered in any new headache as the diagnosis is often missed.
Note: Migraine is not a likely diagnosis in a first-time severe headache.
Investigations
Treatment
Migraine
Clinical features
Investigations will be normal and should be directed towards excluding other serious diseases as suggested by the clinical features—subarachnoid haemorrhage, meningitis, etc.
Treatment
If previous experience with these measures has failed:
If treatment with the above measures has also failed, consider:
PARAPLEGIA
Clinical features
Investigations
CONFUSION
Acute confusion
Adams R.D., Victor M., Ropper A.H. Principles of neurology, 7th edn. New York: McGraw-Hill; 2001.
Cameron P., Jelinek G., Kelly A.-M., et al. Textbook of adult emergency medicine. New York: Churchill Livingstone; 2000.
Dunn R.J.. The emergency medicine manual, 4th edn. Venom Publishing, South Australia, 2006.
Holdgate A., Cuthbert K. Perils and pitfalls of lumbar puncture in the emergency department. Emergency Medicine. 2001;13:351-358.
Khaja A.M., Grotta J.C. Established treatments for acute ischaemic stroke. Review. Lancet. 2007;369(9558):319-330.
Longmore J.M. Oxford handbook of clinical medicine, 5th edn. Oxford, New York: Oxford University Press; 2001.