96 Neurological bladder
Salient features
Examination
Ask the patient the following questions:
• Do you get a sensation when the bladder is full?
• Do you feel the urine passing?
• Are you able to stop urine passing in midstream at your own will?
• Does the bladder leak continually?
• Do you suddenly pass large volumes?
• The examination should concentrate on the legs, because the segments that innervate the bladder are caudal to those that innervate the lower limbs, and spinal cord involvement that affects the innervation of the bladder almost always results in lower limb signs. (Possible exceptions are lesions of the low sacral cord or conus, but only the most caudal lesions fail to produce some overactivity in the legs and extensor plantar responses.)
• Tell the examiner that in male patients you would like to take a history of impotence and examine the neurological system and spine.
Note: Cauda equina lesions at S1 and S2 may impair the ankle reflexes, and those at S3 may affect the intrinsic muscles of the foot, causing foot deformities and fasciculation of the muscles. Saddle anaesthesia is a feature of cauda equina (p. 331) or conus medullaris lesions (p. 332).
Advanced-level questions
What are the types of neurogenic bladder?
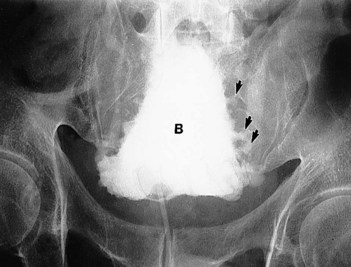
Spinal or spastic bladder. The bladder is small and spastic and holds <250 ml. A hyper-reflexive bladder usually occurs when the spinal cord lesion is at the level of T5 or higher. It is seen in lesions of the spinal cord secondary to trauma, multiple sclerosis and tumour (upper motor neuron lesion). On a contrasted study, a spastic bladder has the shape of a Christmas tree, with little outpouchings along the lateral margins (Fig. 96.1). These areas of outpouching of contrast or urine are pseudodiverticula caused by hypertrophy of the bladder musculature. Bladder fullness is not appreciated and the bladder tends to empty reflexly and suddenly—the automatic bladder. Evacuation may be incomplete unless it is massaged by pressure in the suprapubic region. These patients are prime candidates for urinary infection, calculi and bilateral collecting system dilatation.
Autonomous bladder. This results from damage to the cauda equina (i.e. lower motor neuron lesion; p. 237). These bladders are usually the result of a herniated disc, multiple sclerosis, diabetic neuropathy or lower spinal cord tumour. The patient is incontinent with continual urine dribbling and there is no sensation of bladder fullness. Despite the dribbling, there is considerable residual urine. There is loss of perineal sensation and sexual dysfunction. (In conus medullaris–cauda equina lesions, it is possible to have a flaccid lower motor neuron detrusor, with a spastic sphincter. The reverse may also occur.) Although these patients may demonstrate a large bladder, the upper urinary collecting systems are usually within normal limits, and vesicoureteral reflux is rare.
Sensory bladder. Similar to autonomous bladder and seen in tabes dorsalis, subacute combined degeneration of the cord and multiple sclerosis. There is loss of awareness of bladder fullness with a loss of spinal reflex. This results in retention of large quantities of urine, incontinence with dribbling; the high volume of residual urine can be voided by considerable straining.
Uninhibited bladder. This occurs with lesions affecting the second gyrus of the frontal lobe (e.g. frontal lobe tumours, parasagittal meningiomas, aneurysms of the anterior communicating arteries and some dementia disorders). Patient has urgency despite low bladder volumes and has sudden uncontrolled evacuation. There is no residual urine. When there is deterioration of the intellect, the patient may pass urine at any time without concern.
What do you know about the neurological control of the bladder?
• As the bladder fills, distention stimulates low-level firing of vesical afferents (pelvic nerve), which, in turn, stimulate sympathetic outflow to the bladder outlet (hypogastric nerve to contract the internal sphincter and inhibit detrusor activity) and pudendal outflow to the external urethral sphincter. These responses occur by spinal reflex pathways that promote continence.
• As the bladder becomes fuller, afferents fire more intensely and activate spinobulbospinal reflex pathways passing through the pontine micturition centre. Micturition follows activation of the parasympathetic pathways to the detrusor muscle and inhibition of the somatic input to the external urethral sphincter. The parasympathetic reflex is based in the S3 roots and S3 segments of the cord.
• Ascending afferent input from the spinal cord may pass through the periaqueductal grey matter before reaching the cortex, thereby leading to the sensation of urgency.
• The sympathetic system promotes urinary storage by increasing urethral resistance and depressing detrusor contractions. The sympathetic supply descends into the pelvis from the hypogastric reflex.
• A cortical representation of the bladder is present in the paracentral lobule, stimulation of which may evoke bladder contractions. It may play a part in initiating voluntary contractions and in stopping micturition by initiating contraction of the external sphincter.
What are the different types of urinary incontinence?
• Total incontinence where the patient loses urine at all times and in all positions. It occurs when the sphincter is damaged (surgery, cancerous infiltration and nerve damage) or when there is a fistula between the urinary tract and the skin, or ectopic ureters
• Stress incontinence: occurs when there is an increase in intra-abdominal pressure (on coughing, sneezing, lifting, exercising); it is seen in patients with a lax pelvic floor (e.g. multiparous women, patients who have undergone pelvic surgery) and urine is not lost in the supine position
• Urge incontinence: loss of urine preceded by a strong, unexpected urge to void urine; it occurs with inflammation or neurogenic disorders
• Overflow incontinence: occurs in chronic urinary retention from a chronically distended bladder
• Enuresis: a form of involuntary nocturnal incontinence, usually seen in children.