161
Neurofibromatosis
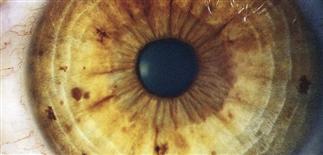
Lisch nodules are pigmented, melanocytic, iris hamartomas. They increase in number with age and are asymptomatic. Slit-lamp examination is essential for differentiations from iris freckles.

Neurofibroma tumors are usually not present in childhood, but they begin to appear at puberty. Tumors increase in both number and size as the patient ages.

Neurofibromatosis is characterized by café-au-lait macules, neurofibromas, and axillary and groin freckling. Axillary freckling is also called Crowe sign.

Multiple large café-au-lait macules are characteristic in neurofibromas. More than 6 lesions larger than 5 mm strongly suggests the diagnosis.
DESCRIPTION
An inherited disorder of the skin and central nervous system made up of at least seven clinical variants. Neurofibromatosis type 1 is the most common variant. It is also called von Recklinghausen disease.
HISTORY
• Inheritance is autosomal dominant; however, 50% of cases arise from a new mutation. • Incidence is estimated at 1 in 3000. • Affects both genders equally. • Pathogenesis is believed to be a defect in the neurofibromin gene.
PHYSICAL FINDINGS
• Typically pink to flesh-colored, soft, pedunculated papules that may be tender. • The number present varies from a few to hundreds or thousands in severe cases. • Dermal and subcutaneous neurofibromas can be present around 5 years of age, but typically start appearing around puberty and increase in number with age and with pregnancy. • Café-au-lait macules (CALMs) are randomly distributed tan to brown patches that increase in number and size in the first 5 years of life; more than six CALMs over 5 mm in diameter suggests the presence of neurofibromatosis type 1. • Axillary or inguinal freckling (Crowe sign) is specific to the disease. • Plexiform neurofibromas occur along the course of peripheral nerves, creating large, tender nodules or poorly demarcated masses, often with overlying hyperpigmentation and hypertrichosis. • About 20% of neurofibromatosis patients have plexiform neurofibromas. When present, these tumors are highly diagnostic. • Malignant degeneration of cutaneous neural tumors occurs in 2% of patients but is rare before age 40. • Lisch nodules are asymptomatic iris hamartomas and occur in more than 90% of neurofibromatosis patients over age 6. Because Lisch nodules are rare in the general population, their presence in patients older than 6 years and suspected of having neurofibromatosis is virtually diagnostic. • Optic gliomas, astrocytomas, meningioma, vestibular schwannoma (acoustic neuroma), and ependymomas also commonly occur in neurofibromatosis patients. • Non-central nervous system tumors occurring in neurofibromatosis type 1 include neurofibrosarcoma, rhabdomyosarcoma, pheochromocytoma, and Wilms tumor. • Skeletal abnormalities include short stature, scoliosis, sphenoid wing dysplasia, and macrocephaly. Renovascular abnormalities may include renal artery stenosis.
TREATMENT
• A multidisciplinary approach with regular follow-up by the primary care physician, ophthalmologist, neurologist, and dermatologist is best. • Head circumference and blood pressure should be monitored closely in children. • Hypertension in a child may indicate renal artery stenosis. In an adult, it may suggest pheochromocytoma. • First-degree relatives should be screened for cutaneous and ophthalmologic signs of neurofibromatosis. • Genetic counseling of patients and their families is recommended.







