62. Neurofibromatosis
Definition
Neurofibromatosis is a familial, multisystem, genetic disorder characterized by developmental changes in the nervous system, muscles, bones, and skin. It is marked by the formation of neurofibromas over the entire body and associated with areas of pigmentation. Neurofibromatosis is also known as von Recklinghausen’s disease.
Incidence
The estimated frequency of neurofibromatosis is 1:3000 to 1:4000 people. The actual incidence may be higher.
Etiology
The cause of neurofibromatosis is mutation or deletion of the NF1 gene, which is found on the long arm of chromosome 17, resulting in decreased production of neurofibromin. The precise role of neurofibromin is still not fully understood, but this gene product has a multitude of effects and diverse functions in several tissues.
Diagnostic Criteria for Neurofibromatosis
Diagnosis requires the presence of two or more of the following seven criteria:
1. Six or more café-au-lait spots or hyperpigmented macules (5 mm in diameter for children younger than 10 years of age or 15 mm in adults)
2. Axillary or inguinal freckles
3. Two or more neurofibromas or one plexiform neurofibroma
4. Two or more iris hamartomas (Lisch nodules)
5. Sphenoid dysplasia or long-bone abnormalities (e.g., pseudoarthrosis)
6. First-degree relative with neurofibromatosis
7. Optic nerve glioma
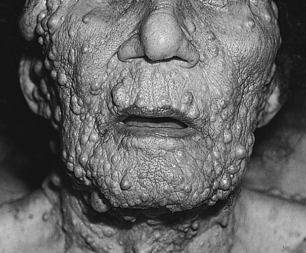 |
| Neurofibromatosis. Neurofibromas. |
Signs and Symptoms
• Axillary or inguinal freckles
• Café-au-lait spots
• Congenital pseudoarthrosis
• Forearm bowing
• Hypertension
• Macrocephaly
• Noncorrectable vision loss
• Optic nerve tumors
• Plexiform neurofibromas with or without hypertrichosis or hyperpigmentation
• Pruritus
• Scoliosis with or without kyphosis
• Sphenoid bone dysplasia
• Subcutaneous or cutaneous neurofibromas
• Thinning and angulation of long bones
Medical Management
Physical examination(s) should be performed at least annually and should focus on detection of potential complications. Early detection helps reduce morbidity and improves the patient’s quality of life. Each annual examination should look for development of new neurofibromas and document the progression of previously existing fibromas.
Physical Examination Documentation for the Patient with Neurofibromatosis
• Blood pressure: Evaluate on every visit; treat hypertension promptly; evaluate for pheochromocytoma or renal artery stenosis
• Cutaneous examination: Neurofibromas or progression of existing neurofibromas; evidence of bony erosion or nerve entrapment
• Neurologic: Development of paresthesia or radiculopathy; weakness or muscle atrophy; incontinence; symptoms of spinal cord neurofibromas
• Skeletal: Scoliosis, hemihypertrophy, long-bone modeling defects
Surgical Interventions for the Patient with Neurofibromatosis
• Angioplasty for renal artery stenosis
• Peripheral nerve sheath tumors, particularly along the brachial and/or sacral plexuses
• Pseudoarthrosis; may require amputation despite attempts at bracing, casting, or other limb-sparing interventions
• Resection and grafting of renal artery stenosis
• Resection for neurofibromas pressing on vital structures, obstructing vision, or growing rapidly
• Resection of neurofibromas for cosmetic and/or aesthetic reasons
• Spinal cord tumor excision
Aside from periodic examination and evaluation, there is no medical therapy that is documented or known to be beneficial to patients with neurofibromatosis. At times pruritus associated with cutaneous neurofibromas may respond to the administration of diphenhydramine; also, carboplatin combined with vincristine sulfate has demonstrated efficacy in treating optic nerve lesions. Surgical interventions include resection of neurofibromas that create cosmetic/aesthetic concerns or that encroach or press on vital structures, obstruct vision, or grow rapidly.
Complications
• Attention deficit disorder
• Attention deficit hyperactivity disorder
• Brachial plexus neurofibroma
• Brain tumors
• Cervical kyphosis
• Dumbbell-shaped spinal cord neurofibromas
• Hypertension secondary to pheochromocytoma
• Kyphosis
• Learning disabilities
• Leukemia
• Locally invasive plexiform neurofibromas
• Long-bone congenital bowing
• Mental retardation
• Neural crest origin malignancies
• Optic nerve lesions
• Paraplegia
• Pathologic fractures
• Peripheral neuropathy
• Pseudoarthrosis
• Renal vascular stenosis secondary to fibromuscular dysplasia
• Sacral plexus neurofibroma
• Sacrolumbar meningocele
• Scoliosis
• Thoracic cage asymmetry
• Tibial pseudoarthrosis
Anesthesia Implications
Because neurofibromas may originate virtually anywhere in the patient’s body, the airway must be thoroughly—almost exhaustively—evaluated. The evaluation should include computed tomography (CT), magnetic resonance imaging (MRI), and/or indirect laryngoscopy. Use of a laryngeal mask airway may be appropriate for many surgical procedures. Neurofibromas may obstruct the patient’s airway on induction of general anesthesia. The patient may quickly become a “can’t ventilate/can’t intubate” patient. It may be necessary to secure the airway via awake fiberoptic means. Fiberoptic methods may not be successful and a tracheotomy may be required to secure the patient’s airway.
Pulmonary complaints and exercise tolerance should be carefully documented. A patient with kyphoscoliosis and chronic lung disease should be evaluated with chest x-ray, arterial blood gas analysis, static and dynamic lung volume determinations, and forced expiratory volumes (gas flow rates).
Regional anesthesia is an entirely appropriate technique for the patient with neurofibromatosis. However, the patient’s back should be closely examined when considering whether to use regional anesthesia for the proposed surgical procedure. The anesthetist must remember that asymptomatic interspace neurofibromas, sacrolumbar meningocele, or severe kyphoscoliosis may seriously impede or completely obstruct identification of and/or entry into the epidural or subarachnoid space.
Pathologic fractures are one of the many complications associated with neurofibromatosis. The anesthetist must take great caution in positioning the patient and ensuring that adequate and proper padding of extremities and other pressure points is provided.
The patient should be evaluated for the presence of a pheochromocytoma by determining the urinary catecholamine concentrations. The anesthetist must have medications to treat a hypertensive crisis easily within reach to avoid any treatment delay.
As yet, no anesthetic drug or technique is strongly recommended for the patient with neurofibromatosis. If the patient has spinal cord lesions higher than the midthoracic level, the condition may be complicated by the development of autonomic hyperreflexia and all its myriad implications. The patient with significant muscle atrophy or wasting should probably not receive succinylcholine.







