CHAPTER 34 Neuroblastoma
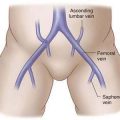
Step 1: Surgical Anatomy
Step 2: Preoperative Considerations
Staging
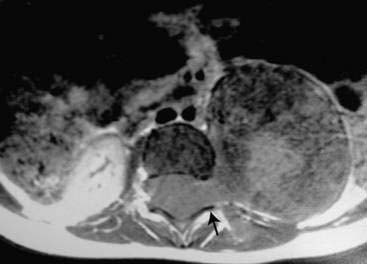
Imaging
Step 3: Operative Steps
General Surgical Principles
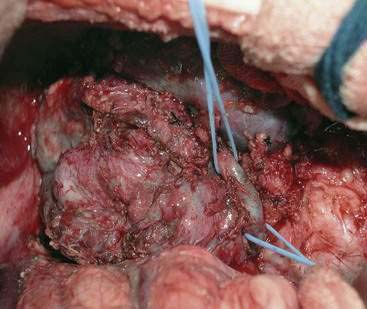
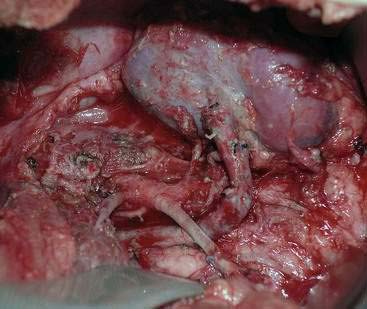
Abdominal Tumors
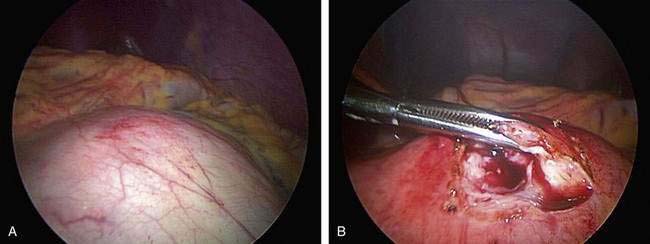
Cervical and Thoracic Tumors
Spinal Tumors
Step 4: Postoperative Care
Step 5: Pearls and Pitfalls
Attiyeh EF, London WB, Mosse YP, et al. Chromosome 1p and 11q deletions and outcome in neuroblastoma. N Engl J Med. 2005;353:2243-2253.
Bowen K, Chung DH. Recent advances in neuroblastoma. Curr Opin Pediatr. 2009;21:350-356.
Brodeur GM. Neuroblastoma: biological insights into a clinical enigma. Nature Rev Cancer. 2003;3:203-216.
Ishola TA, Chung DH. Neuroblastoma. Surg Oncol. 2007;16:149-156.
Von Allmen D, Grupp S, Diller L, et al. Aggressive surgical therapy and radiotherapy for patients with high-risk neuroblastoma treated with rapid sequence tandem transplant. J Pediatr Surg. 2005;40:936-941.