Nervous System
Anatomy and Physiology
Organization of the Nervous System
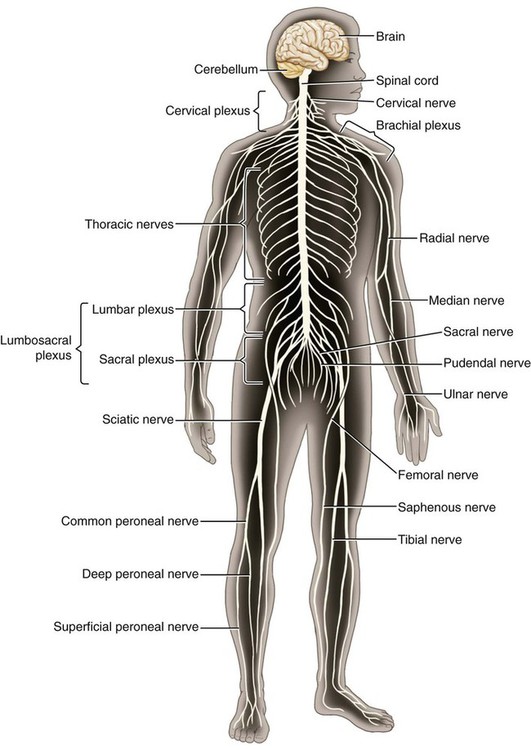
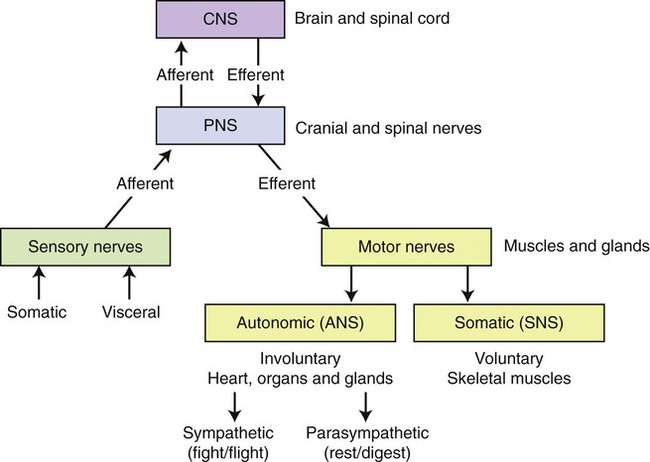
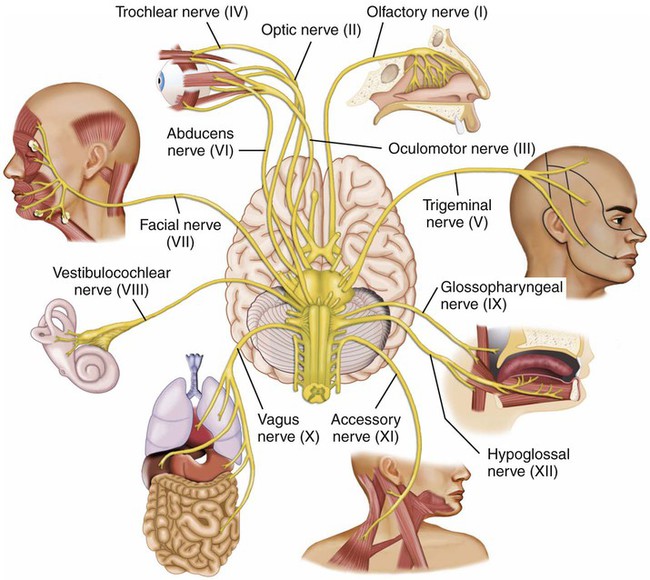
The nervous system is divided into two main systems. (See Figure 11-2 for a schematic of the divisions). The central nervous system (CNS) is composed of the brain and the spinal cord. It is the only site of nerve cells called interneurons, which connect sensory and motor neurons. The peripheral nervous system (PNS) is composed of the nerves that extend from the brain and spinal cord to the tissues of the body. These are organized into 12 pairs of cranial nerves and 31 pairs of spinal nerves. The PNS is further divided into sensory and motor nerves. Sensory (afferent) nerves carry impulses to the brain and spinal cord, whereas motor (efferent) nerves carry impulses away from the brain and spinal cord.
PNS nerves are further categorized into two subsystems:
Somatic nervous system (SNS): this system is voluntary in nature. These nerves collect information from and return instructions to the skin, muscles, and joints.
Autonomic nervous system (ANS): mostly involuntary functions are controlled by this system as sensory information from the internal environment is sent to the CNS, and, in return, motor impulses from the CNS are sent to involuntary muscles: the heart, glands, and organs.
Cells of the Nervous System
The nervous system is made up of the following two types of cells:
1. Parenchymal cells, or neurons, the cells that carry out the work of the system.
2. Stromal cells, or glia, the cells that provide a supportive function.
Neurons
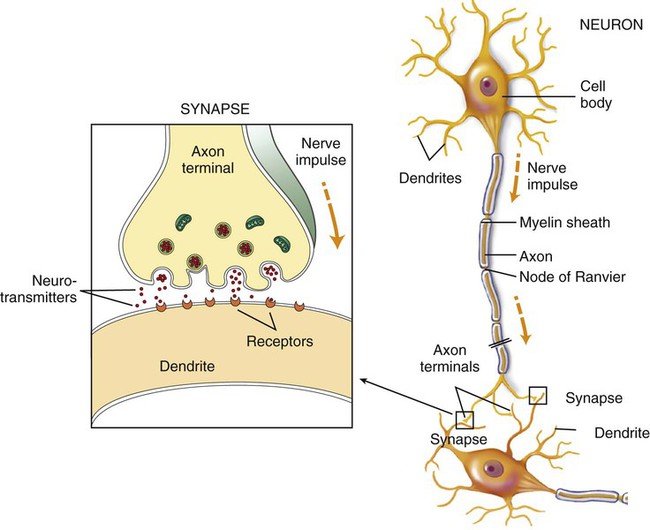
The basic unit of the nervous system is the nerve cell, or neuron (Fig. 11-3). Not all neurons are the same, but all have features in common. Dendrites, projections from the cell body, receive neural impulses, also called action potentials, from a stimulus of some kind. This impulse travels along the dendrite and into the cell body, which is the control center of the cell. This cell body contains the nucleus and surrounding cytoplasm.
From the axon’s terminal fibers, the neurotransmitter is released from the cell to travel across the space between these terminal fibers and the dendrites of the next cell. This space is called the synapse (see Fig. 11-3). The impulse continues in this manner until its destination is reached. A nerve is a group of bundled axons in the PNS. Most nerves contain both sensory and motor fibers.
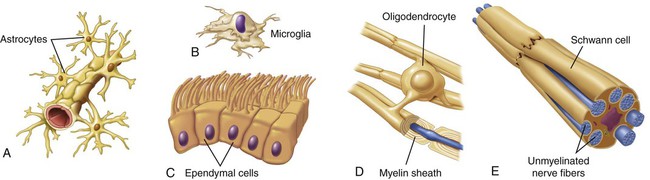
Glia
The supportive, or stromal, glia are also called neuroglia (Fig. 11-4). They accomplish their supportive function by physically holding the neurons together and also protecting them. There are different kinds of neuroglia, including astrocytes, ependymal cells, oligodendroglia, microglia, and Schwann cells. Astrocytes connect neurons and blood vessels and form a structure called the blood-brain barrier (BBB), which prevents or slows the passage of some drugs and disease-causing organisms to the CNS. Ependymal cells line the ventricles of the brain and produce cerebrospinal fluid. Oligodendroglia cover the axons of neurons in the central nervous system, forming their myelin sheath. Microglia perform an active protective function by engulfing and ingesting infectious organisms.
6. perineural ________________________________________________________________________________________
7. oligodendritic ____________________________________________________________________________________
8. microglial ________________________________________________________________________________________
The Central Nervous System
As stated previously, the CNS is composed of the brain and the spinal cord.
Brain (Encephalon)
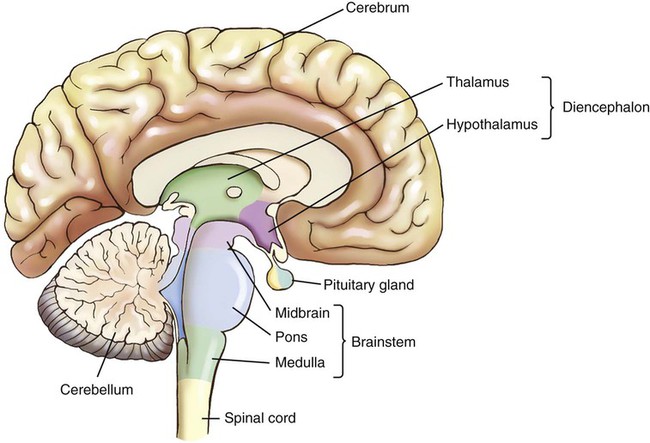
The brain is one of the most complex organs of the body. It is divided into four parts: the cerebrum, the diencephalon, the brainstem, and the cerebellum (Fig. 11-5).
Cerebrum
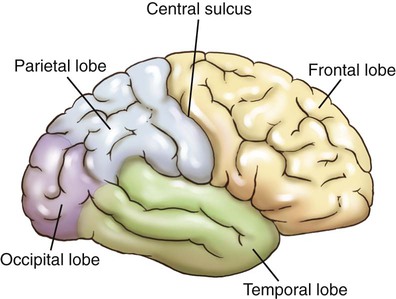
The largest portion of the brain, the cerebrum, is divided into two halves, or hemispheres (Fig. 11-6). It is responsible for thinking, reasoning, and memory. The surfaces of the hemispheres are covered with gray matter and are called the cerebral cortex. Arranged into folds, the valleys are referred to as sulci (sing. sulcus), and the ridges are called the gyri (sing. gyrus). The cerebrum is further divided into sections called lobes, each of which has its own functions:
1. The frontal lobe contains the function of speech and the motor area that controls voluntary movement on the contralateral side of the body. It also is in charge of personality, emotions, and problem solving.
2. The temporal lobes contain the auditory and olfactory areas, and is where sequencing and memory occur.
3. The parietal lobes control the sensations of touch and taste, and also is control of spatial perception.
4. The occipital lobe is responsible for vision.
5. The insular lobes, located under the frontal and temporal lobes, are responsible for empathy, interceptive (internal sensing) awareness, and cognition. The term insula is derived from the Latin word meaning “island,” probably because it is not obviously continuous with the other lobes. Synonyms for insular lobe are the island of Reil and insular cortex.
Spinal Cord
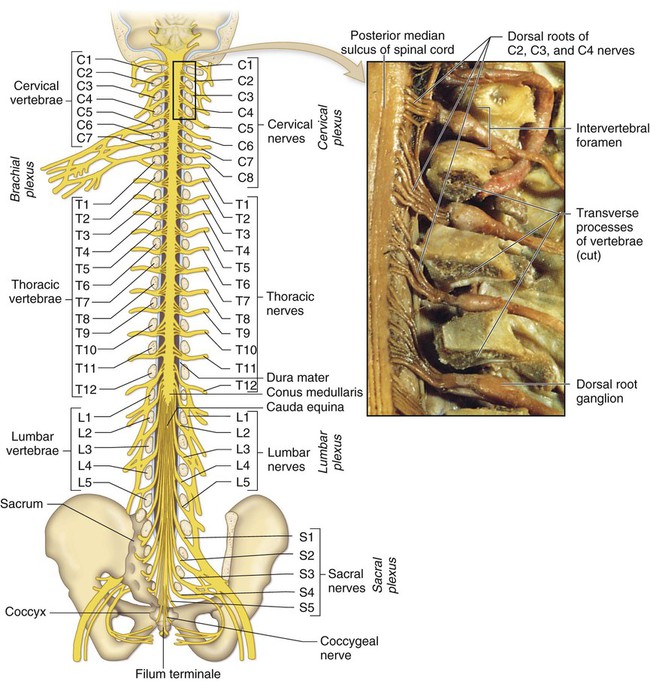
The spinal cord extends from the medulla oblongata to the first lumbar vertebra (Fig. 11-7). It then extends into a structure called the cauda equina (which means “horse’s tail” in Latin). The conus medullaris is the end of the spinal cord, whereas the cauda equina is the collection of nerve roots that extends from it.
Meninges
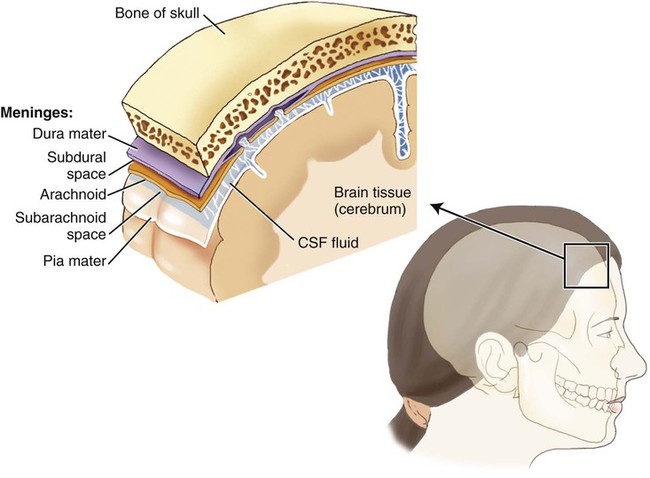
The meninges act as protective coverings for the CNS and are composed of three layers separated by spaces (Fig. 11-8). The dura mater is the tough, fibrous outer covering of the meninges. Its literal meaning is “hard mother.” The falx cerebri is the sickle-shaped fold between the hemispheres. The dura mater is classified as cranial dura mater and spinal dura mater. The tentorium cerebella is an extension of the dura mater that separates the cerebellum from the lower part of the occipital lobes. The diaphragm sellae is a small dural fold that covers the sella turcica; it has a small opening for the infundibulum of the pituitary. The space between the dura mater and arachnoid membrane is called the subdural space. If in the skull, it is the cranial subdural space; if in the spine, it is referred to as the spinal subdural space. Likewise, the subarachnoid space is further categorized as cranial subarachnoid and spinal subarachnoid spaces. The next layer is the arachnoid membrane, a thin, delicate membrane that takes its name from its spidery appearance. The subarachnoid space is the space between the arachnoid membrane and the pia mater. It contains cerebrospinal fluid (CSF), a clear fluid that protects the brain and spinal cord and removes waste products and monitors for internal changes. CSF is also present in cavities in the brain called ventricles. Finally, the pia mater is the thin, vascular membrane that is the innermost of the three meninges; its literal meaning is “soft mother.” The arachnoid and pia mater are referred to as leptomeninges for their slender appearance as opposed to the thick, tough nature of the dura mater.
The Peripheral Nervous System
The peripheral nervous system is divided into:
• 12 pairs of cranial nerves that conduct impulses between the brain and head, neck, thoracic, and abdominal areas, and
• 31 pairs of spinal nerves that closely mimic the organization of the vertebrae and provide innervations to the rest of the body.
The peripheral nerves are a combination of afferent (sensory) nerves and efferent (motor) nerves. The motor nerves are either voluntary or involuntary. The autonomic nervous system (ANS) consists of nerves that regulate involuntary function such as cardiac or smooth muscle. The ANS is further divided into the sympathetic and parasympathetic nervous systems, two opposing mechanisms that provide balance in the body:
• The sympathetic nervous system is capable of producing a “fight-or-flight” response. This is the part of the nervous system that helps the individual respond to perceived stress. The heart rate and blood pressure increase, digestive processes slow, and sweat and adrenal glands increase their secretions.
• The parasympathetic nervous system tends to do the opposite of the sympathetic nervous system—slowing the heart rate, lowering blood pressure, increasing digestive functions, and decreasing adrenal and sweat gland activity. This is sometimes called the “rest and digest” system. An example of a sensory response follows:
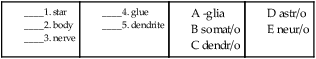
Cranial Nerves
Cranial nerves are named by their number and also their function or distribution. See Figure 11-9 and the table on the next page.
| Number | Name | Origin of Sensory Fibers | Effector Innervated by Motor Fibers |
| I | Olfactory | Olfactory epithelium of nose (smell) | None |
| II | Optic | Retina of eye (vision) | None |
| III | Oculomotor | Proprioceptors* of eyeball muscles | Muscles that move eyeball; muscles that change shape of lens; muscles that constrict pupil |
| IV | Trochlear | Proprioceptors* of eyeball muscles | Muscles that move eyeball |
| V | Trigeminal | Teeth and skin of face | Some muscles used in chewing |
| VI | Abducens | Proprioceptors* of eyeball muscles | Muscles that move eyeball |
| VII | Facial | Taste buds of anterior part of tongue | Muscles used for facial expression; submaxillary and sublingual salivary glands |
| VIII | Vestibulocochlear (auditory) | None | |
| Vestibular branch | Semicircular canals of inner ear (senses of movement, balance, and rotation) | ||
| Cochlear branch | Cochlea of inner ear (hearing) | ||
| IX | Glossopharyngeal | Taste buds of posterior third of tongue and lining of pharynx | Parotid salivary gland; muscles of pharynx used in swallowing |
| X | Vagus | Nerve endings in many of the internal organs (e.g., lungs, stomach, aorta, larynx) | Parasympathetic fibers to heart, stomach, small intestine, larynx, esophagus, and other organs |
| XI | Spinal accessory | Muscles of shoulder | Muscles of neck and shoulder |
| XII | Hypoglossal | Muscles of tongue | Muscles of tongue |
*Proprioceptors are receptors located in muscles, tendons, or joints that provide information about body position and movement.
• The olfactory bulb, the structure responsible for our sense of smell, is coded to the first cranial nerve, the olfactory nerve.
• The optic chiasma is the area of the brain where the optic nerve fibers partially cross and is coded to the second cranial nerve, the optic nerve. If damage to the optic nerve fibers occurs before (proximal to) the chiasma, the patient will exhibit loss of vision on the same side of the lesion. If the damage occurs after (distal to) the chiasma, the vision in the opposite eye is affected because of the crossing. The optic chiasma is coded to the optic nerve.
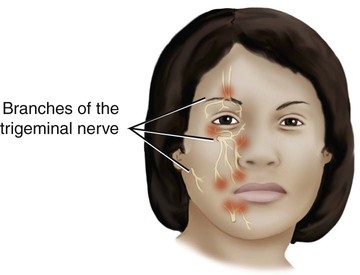
• The fifth cranial nerve, the trigeminal nerve, has three main branches: the ophthalmic nerve, the mandibular nerve, and the maxillary nerve. The ophthalmic nerve receives sensory information from several structures of the eye (except the retina) and the skin of the forehead and nose. The maxillary nerve receives information from the teeth of the upper jaw and the sinuses and skin of the midface. The mandibular nerve has both sensory and motor functions for the lower jaw. Each of these nerves arises from the Gasserian ganglion, also referred to as the trigeminal ganglion, which is a sensory ganglion. This collection of nerves is significant in that it is the site of a dormant herpes virus after a primary herpes infection.
• The facial nerve, cranial nerve VII, has several structures coded to it that have word parts associated with the ear: the chorda tympani (named for its path through the middle ear) is actually involved in the perception of taste, the greater superficial petrosal nerve (innervates the lacrimal glands), the nerve to the stapes (innervates the muscle of one of the ossicles of the ear), the parotid plexus (the location of branching of the facial nerve at one of the salivary glands near the ear), and the posterior auricular nerve (provides sensation from and innervation to the external ear and occipital region of the head). Also coded to the facial nerve are the geniculate and submandibular ganglia. The geniculate ganglion, named for its bent knee appearance, is a mix of sensory, motor, and parasympathetic nerves that provide a sense of taste and innervates several glands in the head and neck. The submandibular ganglion is part of the autonomic nervous system as one of the four parasympathetic ganglia of the head and neck.
• The vestibulocochlear nerve, cranial nerve VIII, is termed the acoustic nerve in PCS. Because its primary functions are balance and hearing, it’s not surprising that the vestibular (sensing positional information) and cochlear (carrying information about sound) nerves are coded to it. The vestibular ganglion (also called Scarpa’s ganglion) connects the vestibular nerve and semicircular canals of the inner ear. The spiral ganglion, a collection of nerve cells in the cochlea that sends sound to the cochlear nerve, is also coded to cranial nerve VIII.
• The glossopharyngeal nerve, cranial nerve IX, is used to code the carotid sinus nerve and the tympanic nerve. The carotid sinus nerve supplies the area that is the small cavity at the beginning of the internal carotid artery, the carotid sinus, along with the structure of the carotid body. This nerve carries impulses that detect pressure and changes in pH in the carotid body. The tympanic nerve (also called Jacobson’s nerve) is a mix of sensory, parasympathetic, and sympathetic nerve fibers that serve the middle ear, the parotid gland, and the carotid plexus.
• The last of the cranial nerves that require extra detail is the tenth cranial nerve, the vagus nerve. Coded to this nerve are the anterior and posterior vagal trunks that direct nerves to organs in the front and back of the body, along with the superior and recurrent (inferior) laryngeal nerves (serving the voice box) and the pharyngeal and pulmonary plexuses. The pharyngeal plexus has sensory and motor fibers for parts of the throat, whereas the pulmonary plexus supplies the lungs.
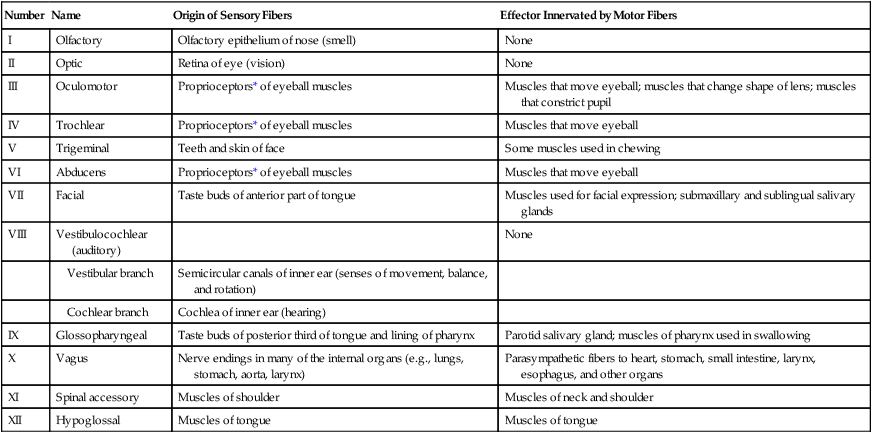
Spinal Nerves
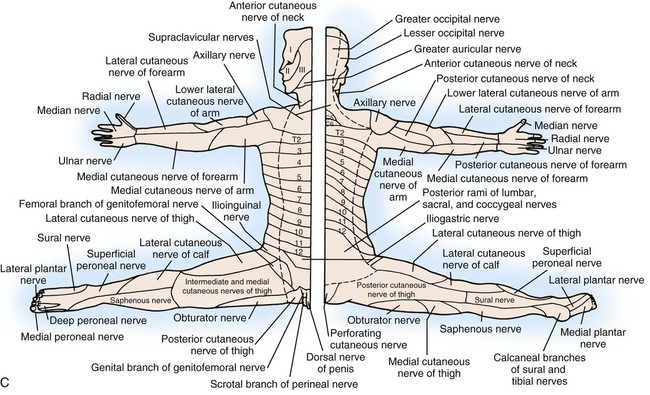
If the nerve fibers from several spinal nerves form a network, it is termed a plexus. Collections of cell bodies in the PNS are referred to as ganglia (sing. ganglion). Spinal nerves are named by their location (cervical, thoracic, lumbar, sacral, and coccygeal) and by number. These nerves are either sensory (often referred to as cutaneous) or muscular. Dermatomes are skin surface areas supplied by a single afferent spinal nerve. These areas are so specific that it is actually possible to map the body by dermatomes (Fig. 11-10, A). This specificity can be demonstrated in patients with shingles, who show similar patterns as specific peripheral nerves are affected (Fig. 11-10, B). Myotomes are the areas of muscles that are supplied by a single efferent spinal nerve (Fig. 11-10, C).
• Occipital nerves (greater, third, and sub-) are coded to cervical nerves that supply the skin and muscles of the head and neck.
• Head and neck sympathetic nerves are used to code the ciliary, otic, sphenopalatine (also referred to as pterygopalatine), and submandibular (formerly called submaxillary) ganglia. The internal carotid plexus and the cavernous plexus are located near the internal carotid artery. The internal carotid plexus is lateral to it, whereas the cavernous plexus is inferior and medial to it. The stellate ganglion, named for its starlike appearance, is located in the lower part of the neck; it may be cut in order to control hyperhidrosis (excessive sweating) or Raynaud’s phenomenon. The cervical ganglia (inferior and superior) are sympathetic nerves in the neck area.
• The median nerve is used to code the anterior interosseous and the palmar cutaneous nerve.
• The radial nerve is used to code the dorsal digital, musculospiral, palmar cutaneous, and posterior interosseous nerves.
• The intercostal, intercostobrachial, and subcostal nerves are coded to the thoracic nerve. Note that each incorporates the word part for the ribs (cost/o), which will help you locate these nerves to the chest.
• Thoracic autonomic nerves are used to code the cardiac, esophageal, thoracic, and pulmonary plexuses. The superior, middle, and inferior cardiac nerves, which are part of the cardiac plexus, are coded as a thoracic sympathetic nerve. The greater, lesser, and least splanchnic nerves, which are sympathetic nerves to the organs within the thorax and the thoracic ganglion, part of the thoracic plexus, are also coded as a thoracic sympathetic nerve.
• The abdominal sympathetic nerve is used to code a large number of plexuses, ganglia, and nerves. Fortunately, the word parts should be familiar to students who have completed the digestive system chapter. The celiac plexus (also called the solar plexus) and ganglion serve the belly, whereas the hepatic, gastric, renal, splenic, suprarenal, and pancreatic plexuses serve the liver, stomach, kidneys, spleen, adrenals, and pancreas respectively. The inferior and superior mesenteric plexuses and ganglia serve the mesentery, whereas the superior and inferior hypogastric plexuses serve the pelvic cavity. The myenteric plexus (also called Auerbach’s plexus) is the primary nervous supply to the digestive system and is responsible for gastric motility. The pelvic splanchnic nerves regulate the evacuation of the bowels and bladder. The submucous plexus, also called Meissner’s plexus, innervates smooth muscle, whereas the abdominal aortic plexus surrounds the abdominal aorta.
• The superior clunic and the lumbosacral trunk are coded to the lumbar nerve.
• The lumbar sympathetic nerve is used to code the lumbar ganglion and the lumbar splanchnic nerve.
• The pudendal nerve is used to code the posterior labial or posterior scrotal nerves.
• The sacral sympathetic nerve is used to code the ganglion impar (also called the ganglion of Walther), the pelvic and sacral splanchnic nerve, and the sacral ganglion.
• The saphenous nerve is coded to the entry of the femoral nerve.
• The tibial nerve is used to code the medial popliteal, medial sural cutaneous, and medial and lateral plantar nerves.
• The peroneal nerve is used to code the lateral sural cutaneous nerve.
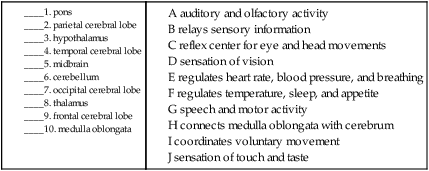
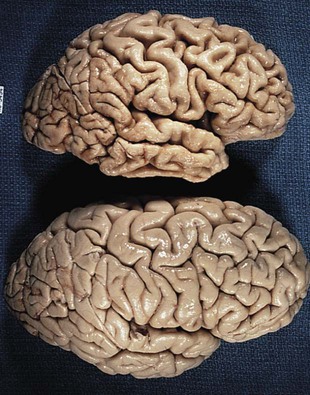
B. Match the CNS part with its combining form.
11. intraventricular __________________________________________________________________________________
12. epidural _________________________________________________________________________________________
13. paraspinal ________________________________________________________________________________________
14. infracerebellar ___________________________________________________________________________________
Combining Forms for the Anatomy and Physiology of the Nervous System
| Meaning | Combining Form |
| body | somat/o |
| brain | encephal/o |
| cerebellum | cerebell/o |
| cerebrum | cerebr/o |
| cortex | cortic/o |
| dendrite | dendr/o |
| dura mater | dur/o |
| globus pallidum | pallid/o |
| lobe | lob/o |
| meninges | mening/o, meningi/o |
| nerve | neur/o |
| nerve root | rhiz/o, radicul/o |
| same | home/o |
| skin | dermat/o |
| spinal cord | cord/o, chord/o, myel/o |
| star | astr/o |
| ventricle | ventricul/o |
| vestibule | vestibul/o |
Suffixes for the Anatomy and Physiology of the Nervous System
| Suffix | Meaning |
| -cyte | cell |
| -glia | glue |
| -on | structure |
| -stasis | stopping, controlling |
| -tome | instrument used to cut |
Pathology
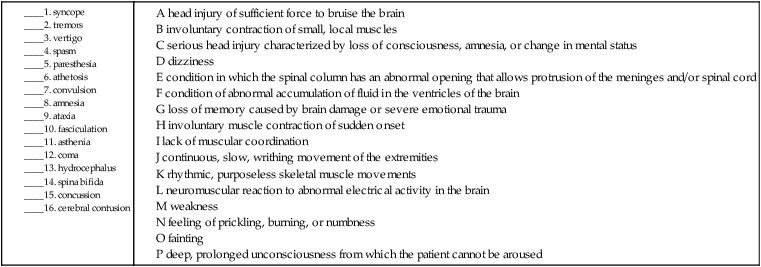
Terms Related to Symptoms and Signs of the Nervous System (R13-R56)
| Term | Word Origin | Definition |
| amnesia | Loss of memory caused by brain damage or severe emotional trauma. | |
| aphasia | a- no, not, without phas/o speech -ia condition |
Lack or impairment of the ability to form or understand speech. Less severe forms include dysphasia and dysarthria; dysarthria refers to difficulty in the articulation (pronunciation) of speech. |
| asthenia | a- no, not, without -sthenia condition of strength |
Weakness. |
| ataxia | a- no, not, without tax/o order, coordination -ia condition |
A condition of a lack of coordination. |
| athetosis | Continuous, involuntary, slow, writhing movement of the extremities. | |
| coma | Deep, prolonged unconsciousness from which the patient cannot be aroused; usually the result of a head injury, neurological disease, acute hydrocephalus, intoxication, or metabolic abnormalities. | |
| convulsion | Neuromuscular reaction to abnormal electrical activity within the brain. Causes include fever or epilepsy, a recurring seizure disorder; also called a seizure. | |
| dysphagia | dys- difficult, bad phag/o eat, swallow -ia condition |
Condition of difficulty with swallowing. |
| fasciculation | Involuntary contraction of small, local muscles. | |
| paresthesia | para- abnormal esthesi/o feeling -ia condition |
Feeling of prickling, burning, or numbness. |
| spasm | Involuntary muscle contraction of sudden onset. Examples are hiccoughs, tics, and stuttering. | |
| syncope | Fainting. A vasovagal attack is a form of syncope that results from abrupt emotional stress involving the vagus nerve’s effect on blood vessels. | |
| tremors | Rhythmic, quivering, purposeless skeletal muscle movements seen in some elderly individuals and in patients with various neurodegenerative disorders. | |
| vertigo | Dizziness; abnormal sensation of movement when there is none, either of oneself moving, or of objects moving around oneself. |
Terms Related to Congenital Malformations of the Nervous System (QØØ-QØ7)
| Term | Word Origin | Definition |
| anencephaly | an- no, not, without encephal/o brain -y condition, process of |
A congenital lack of formation of major portions of the brain. |
| craniorachischisis | crani/o skull, cranium rach/i vertebra -schisis split |
A failure of the skull and vertebral column to fuse during fetal development. |
| hydrocephalus | hydr/o water -cephalus head |
Condition of abnormal accumulation of fluid in the ventricles of the brain; may or may not result in mental retardation. Although usually diagnosed in babies, may also occur in adults as a result of stroke, trauma, or infection (Fig. 11-11). |
| spina bifida | spin/o spine bi- two -fida split |
Condition in which the spinal column has an abnormal opening that allows protrusion of the meninges and/or the spinal cord. This saclike protrusion is termed a meningocele or meningomyelocele (Fig. 11-12). |
Terms Related to Traumatic Conditions (SØ6)
| Term | Word Origin | Definition |
| concussion | Serious head injury characterized by one or more of the following: loss of consciousness, amnesia, seizures, or a change in mental status. | |
| contusion, cerebral | Head injury of sufficient force to bruise the brain. Bruising of the brain often involves the brain surface and causes extravasation of blood without rupture of the pia-arachnoid; often associated with a concussion. | |
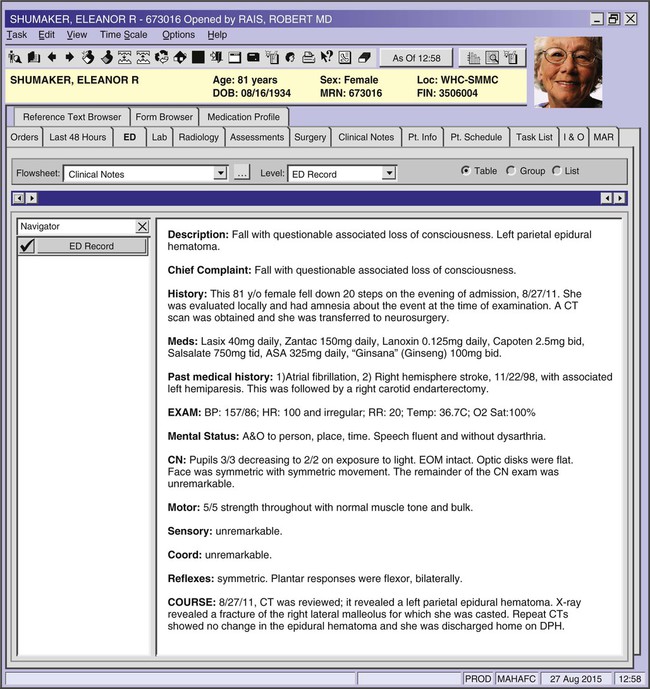
| hematoma | hemat/o blood -oma tumor, mass |
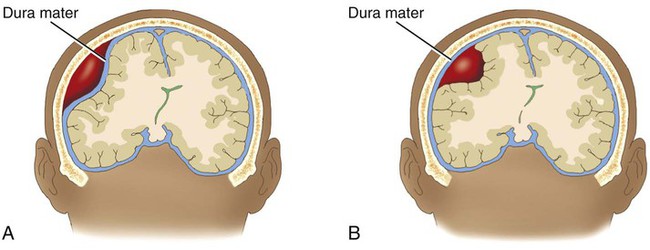
Localized collection of blood, usually clotted, in an organ, tissue, or space, due to a break in the wall of a blood vessel (Fig. 11-13). Epidural hematomas occur above the dura mater. Subdural hematomas occur between the dura mater and arachnoid meninges. May be the result of a traumatic brain injury (TBI). |
17. aphasia _________________________________________________________________________________________
18. dysphagia _______________________________________________________________________________________
19. craniorachischisis ________________________________________________________________________________
20. hematoma ______________________________________________________________________________________
21. anencephaly ____________________________________________________________________________________
Terms Related to Inflammatory Diseases of the Central Nervous System (GØØ-GØ9)
| Term | Word Origin | Definition |
| encephalitis | encephal/o brain -itis inflammation |
Inflammation of the brain, most frequently caused by a virus transmitted by the bite of an infected mosquito. |
| meningitis | mening/o meninges -itis inflammation |
Any infection or inflammation of the membranes covering the brain and spinal cord, most commonly due to viral infection, although more severe strains are bacterial or fungal. |
Terms Related to Systemic Atrophies Primarily Affecting the Central Nervous System (G1Ø-G14)
| Term | Word Origin | Definition |
| amyotrophic lateral sclerosis (ALS) | a- no, not, without my/o muscle troph/o development -ic pertaining to later/o side -al pertaining to sclerosis condition of hardening |
Degenerative, fatal disease of the motor neurons, in which patients exhibit progressive muscle weakness and atrophy; also called Lou Gehrig’s disease. |
| Huntington’s disease | Inherited disorder that manifests itself in adulthood as a progressive loss of neural control, uncontrollable jerking movements, and dementia. Also called Huntington’s chorea. Chorea is derived from the Latin word for “dance.” | |
| postpolio syndrome (PPS) | post- after poli/o gray syn- together -drome run |
Although poliomyelitis (an inflammation of the gray matter of the spinal cord) has been virtually eradicated, some patients who had polio report symptoms of exhaustion and muscle and joint pain decades after their initial illness. |
Terms Related to Extrapyramidal and Movement Disorders (G2Ø-G26)
| Term | Word Origin | Definition |
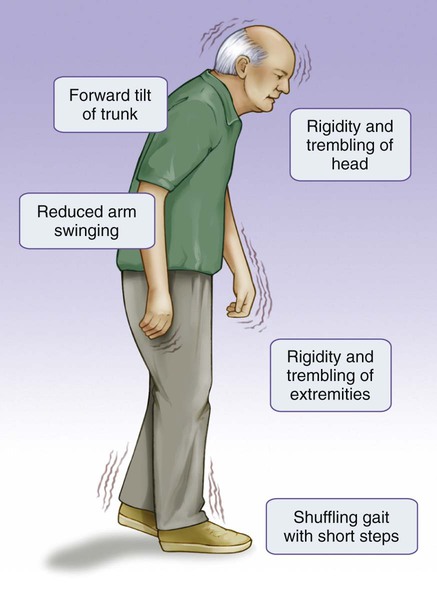
| Parkinson’s disease (PD) | Progressive neurodegenerative disease characterized by tremors, fasciculations, slow shuffling gait, bradykinesia (slow movement), dysphasia, and dysphagia. Its cause is unknown (Fig. 11-14). |
Terms Related to Other Degenerative Disorders of the Central Nervous System (G3Ø-G32)
| Term | Word Origin | Definition |
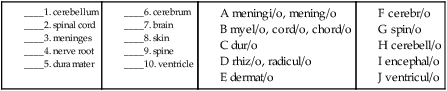
| Alzheimer’s disease (AD) | Progressive neurodegenerative disease in which patients exhibit an impairment of cognitive functioning. The cause of disease is unknown. Alzheimer’s is the most common cause of dementia (Fig. 11-15). | |
| mild cognitive impairment (MCI) | Loss or impairment of cognitive abilities, although not as severe as AD. Also called incipient dementia. |
Terms Related to Demyelinating Diseases of the Central Nervous System (G35-G37)
| Term | Word Origin | Definition |
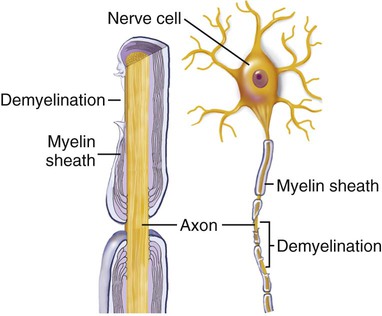
| multiple sclerosis (MS) | sclerosis condition of hardening | Neurodegenerative disease characterized by destruction of the myelin sheaths on the CNS neurons (demyelination) and their abnormal replacement by the gradual accumulation of hardened plaques. The disease may be progressive or characterized by remissions and relapses. Cause is unknown (Fig. 11-16). |
Terms Related to Episodic and Paroxysmal Disorders (G4Ø-G47)
| Term | Word Origin | Definition |
| dyssomnia | dys- difficult somn/o sleep -ia condition |
Disorders of the sleep-wake cycles. Insomnia is the inability to sleep or stay asleep. Hypersomnia is excessive depth or length of sleep, which may be accompanied by daytime sleepiness. |
| epilepsy | epi- above -lepsy seizure |
Group of disorders characterized by some or all of the following: recurrent seizures, sensory disturbances, abnormal behavior, and/or loss of consciousness. Types of seizures include tonic clonic (grand mal), accompanied by temporary loss of consciousness and severe muscle spasms; absence seizures (petit mal), accompanied by loss of consciousness exhibited by unresponsiveness for short periods without muscle involvement. Status epilepticus is a condition of intense, unrelenting, life-threatening seizures. Pseudoseizures are false seizures. Causes may be trauma, tumor, intoxication, chemical imbalance, or vascular disturbances. |
| migraine | Headache of vascular origin. The onset of a migraine may be preceded by an aura, a sensation of light or warmth. Migraines are further classified as intractable (difficult to treat) and with/without status migrainosus (lasting longer than 72 hours). | |
| narcolepsy | narc/o sleep -lepsy seizure |
Disorder characterized by sudden attacks of sleep. Cataplexy is a loss of muscle tone that results in collapse without loss of consciousness (cata- means “down”; -plexy means “seizure”). |
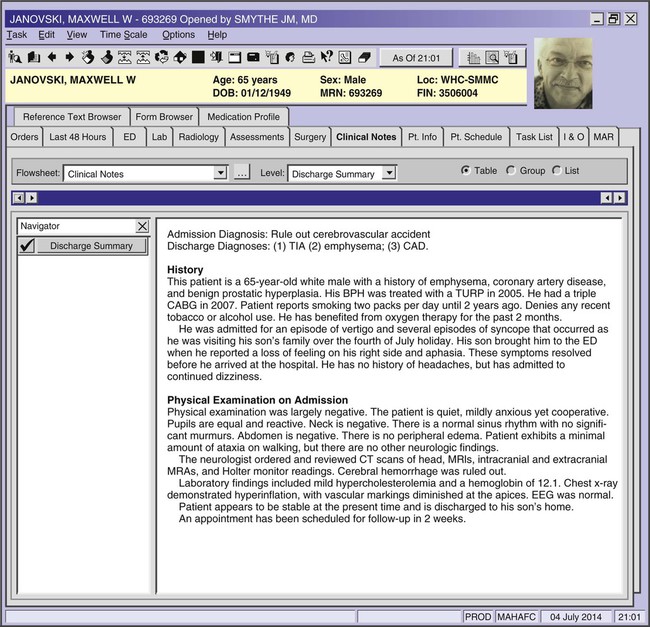
| transient ischemic attack (TIA) | Temporary ischemia of cerebral tissue due to an occlusion (blockage) from a thrombus (pl. thrombi) or embolus (pl. emboli), or as a result of a cerebral hemorrhage. Results of a TIA depend on the duration and location of the ischemia. These sequelae may include paralysis, weakness, speech defects, and sensory changes that last less than 24 hours. |
Terms Related to Nerve, Nerve Root, and Plexus Disorders (G5Ø-G59)
| Term | Word Origin | Definition |
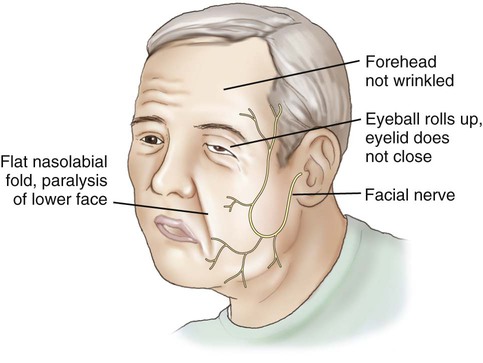
| Bell’s palsy | Paralysis of the facial nerve. Unknown in cause, the condition usually resolves on its own within 6 months (Fig. 11-17). | |
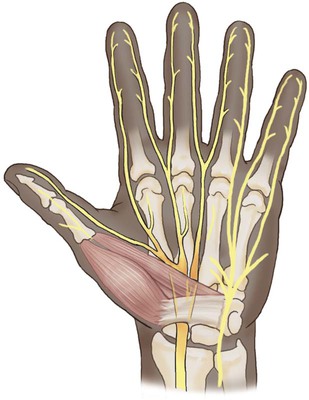
| carpal tunnel syndrome (CTS) | carp/o wrist bone -al pertaining to syn- joined together -drome to run |
Compression injury that manifests itself as fluctuating pain, numbness, and paresthesias of the hand caused by compression of the median nerve at the wrist (Fig. 11-18). |
| causalgia | caus/o burning -algia pain |
Nerve pain, described by patients as a “burning pain.” |
| meralgia paresthetica | mer/o thigh -algia pain par- abnormal -esthetica feeling, sensation |
Condition of a burning, tingling sensation in the thigh caused by injury to one of the femoral nerves. |
| trigeminal neuralgia | neur/o nerve -algia pain |
Chronic facial pain that affects the fifth cranial nerve (Fig. 11-19). Usually experienced on one side of the face. The pain is episodic and intense. Also known as tic douloureux. |
Terms Related to Polyneuropathies and Other Disorders of the PNS (G6Ø-G64)
| Term | Word Origin | Definition |
| Guillain-Barré syndrome | Autoimmune disorder of acute polyneuritis producing profound myasthenia that may lead to paralysis. | |
| polyneuropathy | poly- many neur/o nerve -pathy disease condition |
A general term describing a disorder of several peripheral nerves. |
Terms Related to Diseases of Myoneural Junction and Muscle (G7Ø-G73)
| Term | Word Origin | Definition |
| muscular dystrophy (MD) | muscul/o muscle -ar pertaining to dys- bad, abnormal troph/o development -y condition, process of |
Group of disorders characterized as an inherited progressive atrophy of skeletal muscle without neural involvement (Fig. 11-20). |
| myasthenia gravis | my/o muscle a- without, no -sthenia condition of strength gravis severe |
Usually severe condition characterized by fatigue and progressive muscle weakness, especially of the face and throat (Fig. 11-21). |
Terms Related to Cerebral Palsy and Other Paralytic Syndromes (G8Ø-G83)
| Term | Word Origin | Definition |
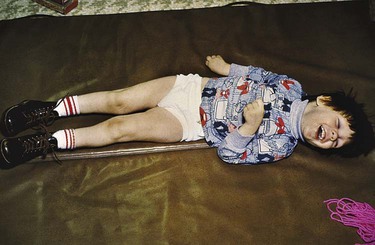
| cerebral palsy (CP) | cerebr/o cerebrum -al pertaining to |
Motor function disorder as a result of permanent, nonprogressive brain defect or lesion caused perinatally. Neural deficits may include paralysis, ataxia, athetosis, seizures, and/or impairment of sensory functions (Fig. 11-22). |
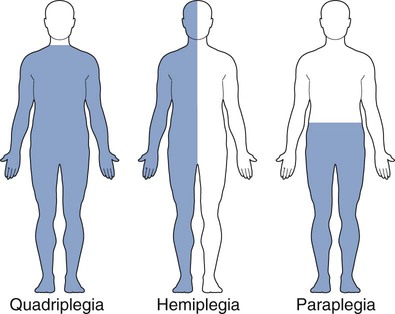
| diplegia | di- two -plegia paralysis |
Paralysis of the same body part on both sides of the body. |
| hemiparesis | hemi- half -paresis slight paralysis |
Muscular weakness or slight paralysis on the left or right side of the body. |
| hemiplegia | hemi- half -plegia paralysis |
Paralysis on the left or right side of the body (Fig. 11-23). |
| locked-in state | Damage to the upper brainstem that leaves the patient paralyzed and mute. | |
| monoplegia | mono- one -plegia paralysis |
Paralysis of one limb on the left or right side of the body. |
| paraplegia | para- abnormal -plegia paralysis |
Paralysis of the lower limbs and trunk (Fig. 11-23). |
| quadriplegia | quadri- four -plegia paralysis |
Paralysis of arms, legs, and trunk (Fig. 11-23). |
13. causalgia ________________________________________________________________________________________
14. meralgia paresthetica ____________________________________________________________________________
15. polyneuropathy _________________________________________________________________________________
16. hemiplegia ______________________________________________________________________________________
17. diplegia _________________________________________________________________________________________
Terms Related to Neoplasms of the CNS*
| Term | Word Origin | Definition |
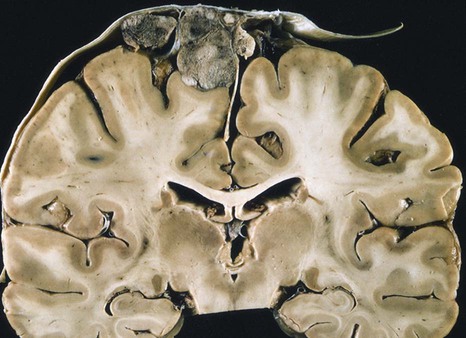
| astrocytoma | astr/o star cyt/o cell -oma tumor, mass |
Tumor arising from star-shaped glial cells that is malignant in higher grades. A grade IV astrocytoma is referred to as a glioblastoma multiforme, the most common primary brain cancer (Fig. 11-24). |
| ependymoma | Tumors of the cells that line the ventricles of the brain. In children, ependymomas are usually intracranial; in adults they are most often intraspinal. | |
| medulloblastoma | medull/o medulla blast/o embryonic -oma tumor, mass |
Tumor that arises from embryonic tissue in the cerebellum. Most commonly seen in children. |
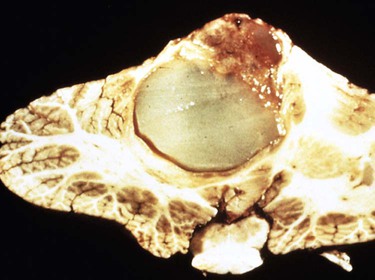
| meningioma | meningi/o meninges -oma tumor, mass |
Slow growing, usually benign tumor of the meninges. Although benign, may cause problems because of its size and location (Fig. 11-25). |
| neuroblastoma | neur/o nerve blast/o embryonic -oma tumor, mass |
Highly malignant tumor arising from either the autonomic nervous system or the adrenal medulla. Usually affects children younger than 10 years of age. |
Terms Related to Neoplasms of the PNS*
| Term | Word Origin | Definition |
| ganglioneuroma | gangli/o ganglia neur/o nerve -oma tumor, mass |
Usually benign, slow-growing tumor that originates in the autonomic nervous system cells. |
| neurofibroma | neur/o nerve fibr/o fiber -oma tumor, mass |
Benign fibrous tumors of tissue surrounding the nerve sheath. |
| schwannoma | A type of tumor, benign or malignant, that is most commonly found in the inner ear (vestibular schwannoma). |
*Most neoplasms that are related to the nervous system arise from the supportive glial cells, although a few others do occur. It is important to note the difference between primary brain cancers (those that originate in the brain) and metastatic cancers that have spread to the brain from another location.
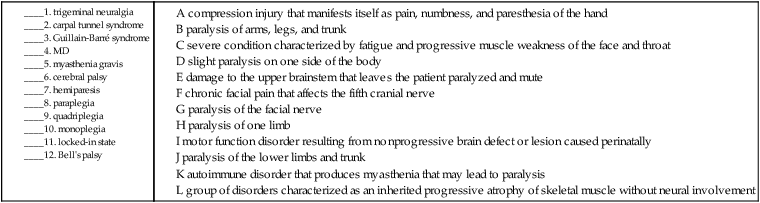
Procedures
A, Insertion of dye through a catheter in the common carotid artery outlines the vessels of the brain. B, Angiogram showing vessels. 1, internal carotid artery; 2, middle cerebral artery; 3, middle meningeal artery.
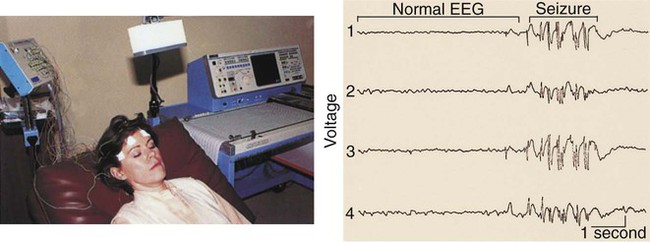
A, Photograph of person with electrodes attached. B, EEG tracing showing activity in four different places in the brain. Compare the normal activity with the explosive activity that occurs during a seizure.
| Term | Word Origin | Definition |
| cerebral angiography | cerebr/o cerebrum -al pertaining to angi/o vessel -graphy recording |
X-ray of the cerebral arteries, including the internal carotids, taken after the injection of a contrast medium (Fig. 11-26); also called cerebral arteriography. |
| chemothalamectomy | chem/o chemical, drug thalam/o thalamus -ectomy cutting out |
Injection of chemical substance to destroy part of the thalamus. Used to treat Parkinson’s and Huntington’s diseases. |
| cordotomy | cord/o spinal cord -tomy cutting |
Incision of the spinal cord to relieve pain. Also spelled chordotomy. |
| craniotomy | crani/o skull, cranium -tomy cutting |
Incision into the skull as a surgical approach or to relieve intracranial pressure; also called trephination. |
| deep tendon reflexes (DTR) | Assessment of an automatic motor response by striking a tendon. Useful in diagnosis of TIA and CVA. Babinski’s sign is the loss or diminution of the Achilles tendon reflex seen in sciatica. | |
| echoencephalography | echo -sound encephal/o brain –graphy recording |
Ultrasound exam of the brain, usually done only on newborns because sound waves do not readily penetrate bone. |
| electroencephalography (EEG) | electr/o electricity encephal/o brain -graphy recording |
Record of the electrical activity of the brain. May be used in the diagnosis of epilepsy, infection, and coma (Fig. 11-27). |
| ganglionectomy of the dorsal root | ganglion/o ganglion -ectomy cutting out |
Removal of the dorsal root ganglia to treat pain. |
| hemispherectomy | hemi- half spher/o sphere, round -ectomy cutting out |
Removal of a cerebral hemisphere to treat intractable epilepsy. |
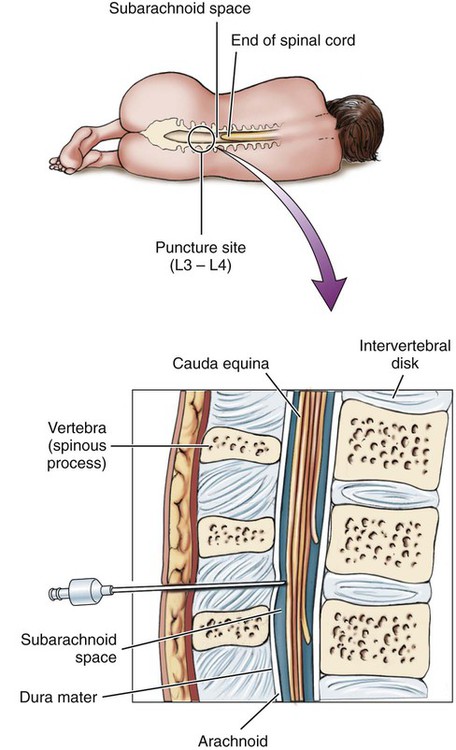
| lumbar puncture (LP) | lumb/o lower back -ar pertaining to |
Procedure to aspirate CSF from the lumbar subarachnoid space. A needle is inserted between two lumbar vertebrae to withdraw the fluid for diagnostic purposes. Once removed, the CSF is analyzed to detect pathogens and abnormalities. Also called a spinal tap (Fig. 11-28). |
| myelography | myel/o spinal cord -graphy recording |
X-ray of the spinal canal after the introduction of a radiopaque contrast. |
| nerve block | Use of anesthesia to prevent sensory nerve impulses from reaching the CNS. | |
| nerve conduction test | Test of the functioning of CNS or peripheral nerves. Conduction time (impulse travel) through a nerve is measured after a stimulus is applied; used to diagnose polyneuropathies. | |
| neurectomy | neur/o nerve -ectomy cutting out |
Excision of part or all of a nerve to alleviate pain. |
| neurexeresis | neur/o nerve -exeresis tearing out |
Removal of the fifth cranial nerve to treat trigeminal neuralgia. |
| neuroplasty | neur/o nerve -plasty surgically forming |
Surgical repair of a nerve. |
| neurotomy | neur/o nerve -tomy cutting |
Incision of a nerve. Radiofrequency ablation is used to treat facet joint pain in the neck and back. |
| pallidotomy | pallid/o globus pallidum -tomy cutting |
Destruction of the globus pallidum to treat Parkinson’s disease. The procedure relieves muscular rigidity and tremors. |
| phrenemphraxis | phren/o diaphragm, phrenic nerve -emphraxis obstructing, crushing |
Crushing of the phrenic nerve to cause its paralysis. Also called phrenicotripsy and phreniclasis. |
| polysomnography (PSG) | poly- many somn/o sleep -graphy recording |
Measurement and record of a number of functions while the patient is asleep (e.g., cardiac, muscular, brain, ocular, and respiratory functions). Most often used to diagnose sleep apnea (Fig. 11-29). |
| rhizotomy | rhiz/o spinal nerve root -tomy cutting |
Resection of the dorsal root of a spinal nerve to relieve pain. |
| sympathectomy | sympath/o to feel with -ectomy cutting out |
Surgical interruption of part of the sympathetic pathways for the relief of chronic pain or to promote vasodilation. |
| tractotomy | tract/o tract, pathway -tomy cutting |
Cutting of a nerve tract to alleviate pain. |
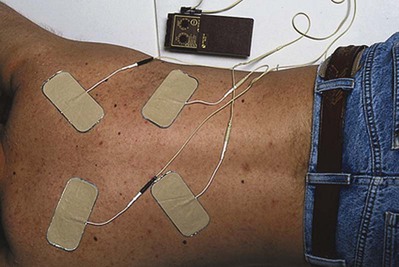
| transcutaneous electrical nerve stimulation (TENS) | trans- through cutane/o skin -ous pertaining to |
Method of pain control effected by the application of electrical impulses through the skin (Fig. 11-30). |
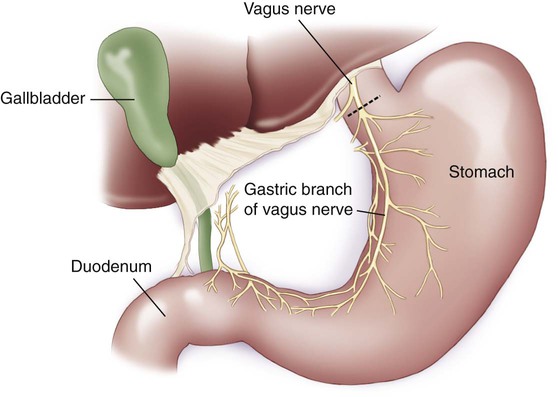
| vagotomy | vag/o vagus nerve -tomy cutting |
Cutting of a branch of the vagus nerve to reduce the secretion of gastric acid (Fig. 11-31). |
| ventriculocisternostomy | ventricul/o ventricle cistern/o box, cistern -stomy making a new opening |
The creation of a new opening between a blocked ventricle and a cerebral cistern. Used to treat hydrocephalus. |
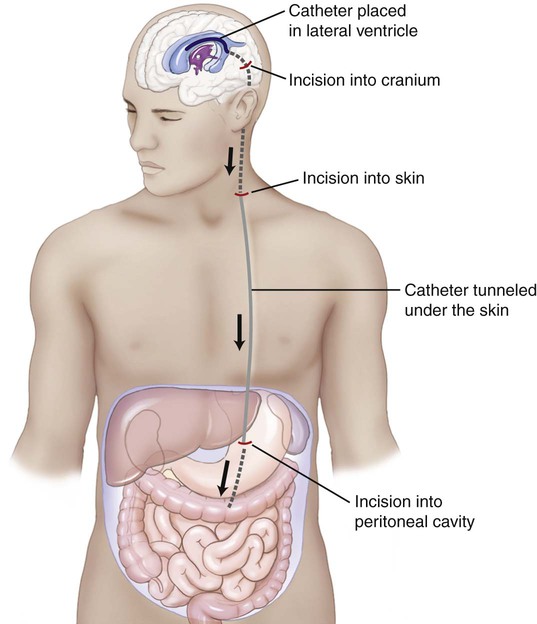
| ventriculoperitoneostomy | ventricul/o ventricle peritone/o peritoneum -stomy making a new opening |
Procedure to drain fluid from brain ventricles through a shunt, catheter, and valve that leads to the abdominal cavity (Fig. 11-32). Neuroendoscopy, a procedure that uses a fiberoptic camera to visualize neural structures, is used to place the shunt. |
| ventriculostomy, endoscopic | endo- within -scopic pertaining to viewing ventricul/o ventricle -stomy making a new opening |
A new opening between the third ventricle and the subarachnoid space; used to treat one type of hydrocephalus. |
Recognizing Suffixes for PCS
Suffixes and Root Operations for the Nervous System
| Suffix | Root Operation |
| -ectomy | Excision, resection, destruction |
| -emphraxis | Destruction |
| -exeresis | Extraction |
| -plasty | Repair, supplement |
| -stomy | Bypass, drainage |
| -tomy | Drainage, division, destruction |
15. chemothalamectomy ____________________________________________________________________________
16. phrenemphraxis __________________________________________________________________________________
17. echoencephalography ____________________________________________________________________________
18. vagotomy _______________________________________________________________________________________
19. neuroplasty _____________________________________________________________________________________
20. ventriculoperitoneostomy ________________________________________________________________________
Pharmacology
analgesics: Reduce pain. Narcotic analgesics have a CNS effect and include NSAIDs (nonsteroidal antiinflammatory drugs), opioids, or COX-2 inhibitors. Examples include morphine (MS Contin), hydrocodone (Vicodin or Lortab, in combination with acetaminophen), sumatriptan (Imitrex), acetaminophen (Tylenol), and naproxen (Anaprox).
anesthetics: Cause a loss of feeling or sensation. They can act either locally (local anesthetic) or systemically (general anesthetic), and a general anesthetic can induce unconsciousness. Examples include propofol (Diprivan) and lidocaine (Xylocaine, Lidoderm).
anticonvulsants: Reduce the frequency and severity of epileptic or other convulsive seizures. Examples include clonazepam (Klonopin), carbamazepine (Tegretol), and phenytoin (Dilantin).
antiparkinsonian drugs: Effective against Parkinson’s disease. Examples include levodopa and carbidopa (Sinemet) and tolcapone (Tasmar).
antipyretics: Reduce fever. Examples include aspirin (Bayer), acetaminophen (Tylenol), and ibuprofen (Advil, Motrin).
hypnotics: Promote sleep. They may also be referred to as soporifics or somnifacients. Many hypnotics have a sedative effect also. Examples include temazepam (Restoril), zolpidem (Ambien), and flurazepam (Dalmane).
neuromuscular blockers: Drugs that block the action of acetylcholine at the motor nerve end plate to cause paralysis. May be used in surgery to minimize patient movement. Examples include pancuronium (Pavulon), vecuronium (Norcuron), and succinylcholine (Anectine).
sedatives: Inhibit neuronal activity to calm and relax. Many sedatives also have hypnotic effects. Examples include alprazolam (Xanax), lorazepam (Ativan), and phenobarbitol (Luminal).
stimulants: Increase synaptic activity of targeted neurons in the CNS to treat narcolepsy, attention-deficit disorder with hyperactivity, and fatigue, and to suppress the appetite. Examples include dextroamphetamine (Dexedrine), methylphenidate (Ritalin), caffeine, and phentermine (Adipex-P).
| Abbreviation | Meaning |
| AD | Alzheimer’s disease |
| ALS | amyotrophic lateral sclerosis |
| ANS | autonomic nervous system |
| BBB | blood-brain barrier |
| C1-C8 | cervical nerves |
| CNS | central nervous system |
| CP | cerebral palsy |
| CSF | cerebrospinal fluid |
| CTS | carpal tunnel syndrome |
| EEG | electroencephalogram |
| L1-L5 | lumbar nerves |
| LP | lumbar puncture |
| MCI | mild cognitive impairment |
| MD | muscular dystrophy |
| MS | multiple sclerosis |
| PD | Parkinson’s disease |
| PNS | peripheral nervous system |
| PPS | postpolio syndrome |
| PSG | polysomnography |
| S1-S5 | sacral nerves |
| SNS | somatic nervous system |
| T1-T12 | thoracic nerves |
| TBI | traumatic brain injury |
| TENS | transcutaneous electrical nerve stimulation |
| TIA | transient ischemic attack |