Chapter 24 Nerve Transfers
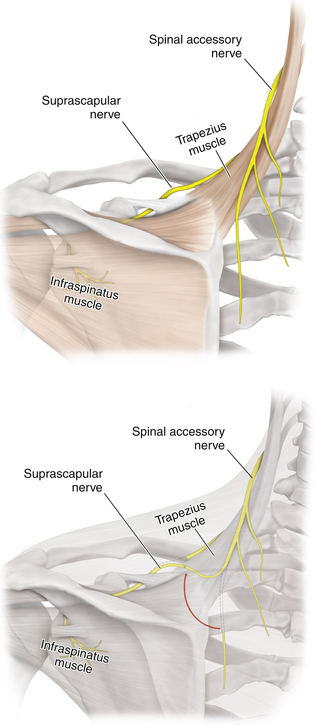
Accessory Nerve to Suprascapular Nerve (Figure 24-1)
• The distal accessory nerve can be utilized when (1) useful lead-outs from C5 or C6 are not available for neurotization of the suprascapular nerve (SCN), or (2) the surgeon wishes to use such lead-outs for other destinations in the plexus.
• The distal accessory nerve can be mobilized and sewn either end-to-end or by means of an interpositional graft to the SCN.
• Stimulation of CN XI produces muscular contraction of the trapezius and sternocleidomastoid. The SCN is dissected back into the upper trunk and is divided through viable tissue.
• The mobilized accessory nerve is divided so that it can be tunneled beneath some of the supraclavicular fat pad and sewn by 7-0 Prolene to the mobilized suprascapular nerve.
Pectoral Branches (Medial) to Musculocutaneous Nerve
• The lateral cord is traced distally to the cord’s contribution to the median nerve medially and the coracobrachialis branches and musculocutaneous nerve (MCN) laterally (see Chapter 5).
• The MCN is encircled with a Penrose drain and is usually split away from the lateral cord contribution to the median nerve more proximally. Thus a suitable entry point for anastomosis with the shorter medial pectoral branches is created so that the juxtaposition can be done gracefully and without tension.
• Medial pectoral branches, arising from the medial cord, are located by dissecting out the axillary artery. Usually the medial pectoral branches are found close to and somewhat beneath the largest pectoral arterial branches.
• The medial pectoral nerve branches reach the pectoral muscles.
• After the pectoral branches are cut close to the muscle, they are moved laterally, usually beneath the axillary artery, and sewn end-to-end with 7-0 Prolene to either a partially or a completely sectioned distal MCN.
Intercostal Nerves to Musculocutaneous Nerve
• This transfer is done to neurotize the MCN.
• The procedure provides useful biceps and brachialis function in about 40% to 50% of cases, depending on the series and the nature of the patients selected for the procedure.
• Some controversy exists over which intercostal nerves to use to maximize motor axon outflow, as well as over the level at which they should be sectioned. We prefer to use the third, fourth, fifth, and sometimes sixth intercostal nerves and usually section them at the anterior axillary line.
• The incision needs to be combined with one made to expose the plexus at the cord-to-nerve level in the axilla.
• The intercostal nerves are found under the inferior surface of their respective ribs, below the intercostal vessels, in the neurovascular plane. With upward retraction on the rib, the nerve can be identified, encircled by a Vasaloop, and then dissected away from the intercostal artery and vein.
• In women, the superficial branch of the T4 intercostal nerve can be spared and only the deep (motor or muscular) branch used. This preserves sensation on and around the nipple.
• We dissect out lengths of 4 or 5 inches, extending from the posterior axillary line.
• The intercostal nerves are sectioned anteriorly at the level of the anterior axillary line and brought back to be tunneled through axillary fat to reach the axillary level of the plexus.
• They are then sewn together directly to the MCN, which has been split away from the lateral cord contribution to the median nerve, or to the axillary nerve.
• Care must be taken not to lacerate the pleura. If this is done, it is repaired with 4-0 silk on a fine needle.
• It is sometimes useful to harvest a small piece of pectoral or intercostal muscle to be sewn in place as a stent or stamp for closure of the hole.
Descending Cervical Plexus to Upper and Middle Trunk
• Some of the most important relationships in plexus surgery are those among the C5 and C6 spinal nerves, the phrenic nerve, and the descending cervical plexus.
• The cervical plexus originates from C3 and C4. The phrenic nerve has input from C3, C4, and C5.
• The descending cervical plexus usually consists of several branches that then branch several more times to eventually innervate the strap muscles and skin of the neck
• The descending cervical plexus can be used as a transfer to plexus divisions, although motor fibers available for neurotization are limited.
• Other transfers, such as thoracodorsal to axillary, phrenic to truncal divisions, partial ulnar to musculocutaneous nerve, or contralateral C7, are used infrequently by the authors.
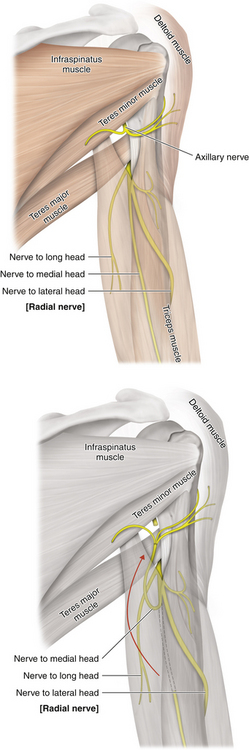
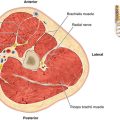
Radial Nerve to Axillary Nerve (Figure 24-2)1
• The brachial plexus is dissected first at the level of the axilla.
• Intraoperative nerve action potential examination is required to make a correct diagnosis and to repair the damaged nerve.
• The posterior cord is divided into the axillary and radial nerves. The lateral cord is divided into the musculocutaneous and median nerves. The medial cord is divided into the median and ulnar nerves.
• The radial nerve should be electrically tested after branching off the axillary nerve.
• A fascicle from the radial nerve is harvested and assessed for viability using electrical nerve stimulation. Viable nerves may possibly be transferred to the nerve branch of the triceps medial head.
• The axillary nerve is cut after branching from the posterior cord and is sutured under the microscope to the partially cut radial nerve.
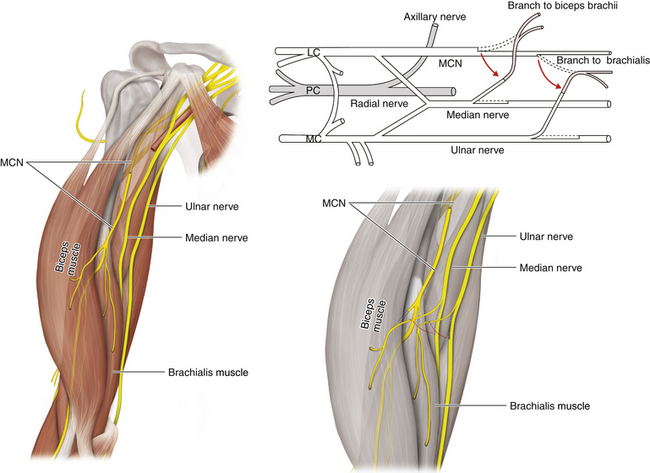
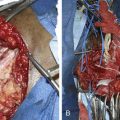
Median and Ulnar Nerve to Musculocutaneous Nerve (Figure 24-3)2
• The biceps and brachialis nerve branches (musculocutaneous nerve branches) are dissected proximally and transferred to the donor median and ulnar nerves.
• The flexor carpi radialis tendon is explored at the wrist level.
• One fascicle of the flexor carpi ulnaris on the lateral border of the ulnar nerve and one fascicle of the flexor carpi radialis on the medial border of the median nerve are harvested.
• Next, one fascicle from each of these nerves is partially cut out.
• Donor nerve fascicles are separated and are sutured to musculocutaneous nerve branches.
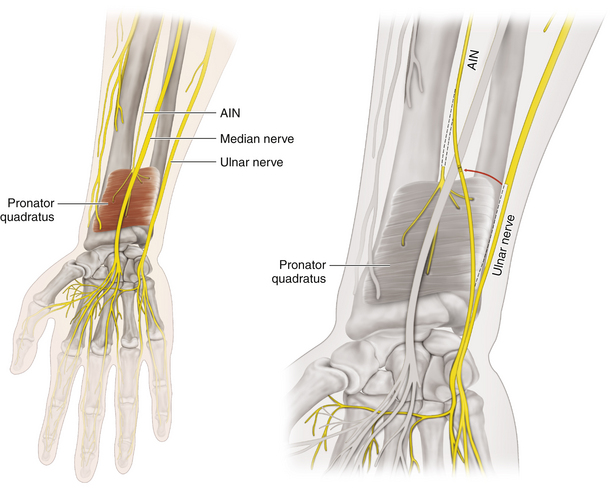
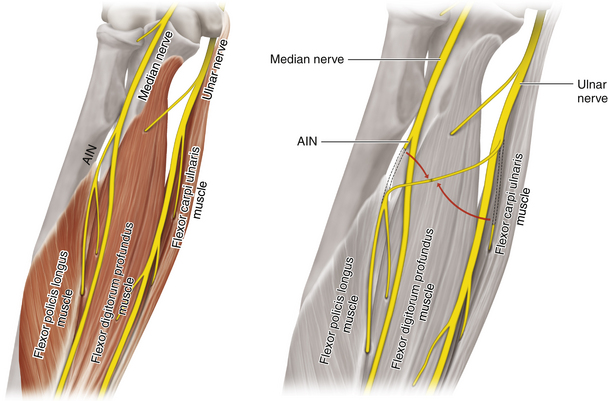
Anterior Interosseous Nerve to Ulnar Nerve (Figure 24-4)3
• An incision is made ulnar to the thenar crease in the hand.
• It is then necessary to dissect the Guyon canal and to identify the deep motor branch of the ulnar nerve at the level of the hook of the hamate.
• The deep motor branch of the ulnar nerve is traced from about 2 inches proximally from the distal wrist crease to the proximal border of the pronator quadratus. These fascicles must then be followed to the level of the anterior interosseous nerve (AIN).
• The AIN begins to branch near the midportion of the pronator quadratus, and the nerve should be separated proximal to the split.
• A direct repair of the AIN to the deep motor branch of the ulnar nerve is then completed.
Ulnar Nerve to Anterior Interosseous Nerve (Figure 24-5)4
• An incision is made midway between the passage of the ulnar and median nerves at the elbow level.
• The ulnar nerve is dissected at its entrance through the ulnar tunnel and then also distally.
• The surgeon should then divide the flexor carpi ulnaris muscle (FCU) proximally, detach it from its proximal insertion at the medial epicondyle, and reflect it anteriorly and ventrally.
• Nerve branches to the muscle are identified and carefully dissected.
• The first and second branches to the FCU are measured, using a caliper, for their length from their emergence from the ulnar nerve and for their width in millimeters. Both branches are then separated with a scalpel.
• The point of emergence of the AIN is dissected, just proximal to the arch of the flexor digitorum superficialis and 5 to 8 cm distal to the medial epicondyle.
• Both branches to the FCU should then be sectioned as distally as possible, immediately proximal to their entry point into the muscle.
• Both branches to the FCU are then brought into contact with the AIN.
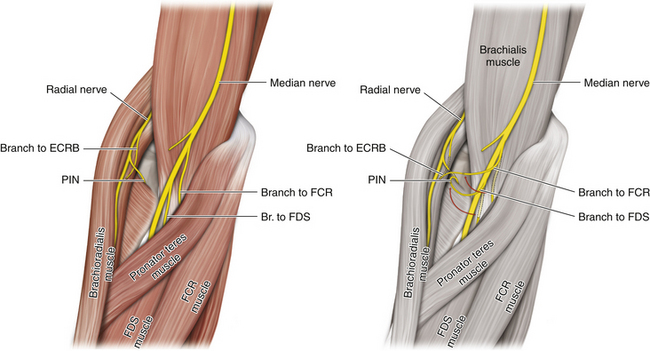
Median Nerve to Radial Nerve (Figure 24-6)5
• An incision is made in the proximal volar forearm just below the antecubital crease.
• The median nerve and its branches are identified by means of intraoperative stimulation of the flexor digitorum superficialis (FDS), flexor carpi radialis (FCR), and palmaris longus (PL) muscles, the AIN, and the main median nerve.
• Through the same incision, the radial sensory nerve can be identified and followed to identify the posterior interosseous nerve (PIN) and the branch to the extensor carpi radialis brevis (ECRB).
• In preparation for nerve transfer, the radial nerve branches to the ECRB and the PIN should be separated as proximally as possible to maximize length for the transfer.
• The nerve branch to the FDS and the FCR/PL branch of the median nerve should then be divided as distally as possible to allow a direct tension-free end-to-end coaptation to the ECRB branch and the PIN.
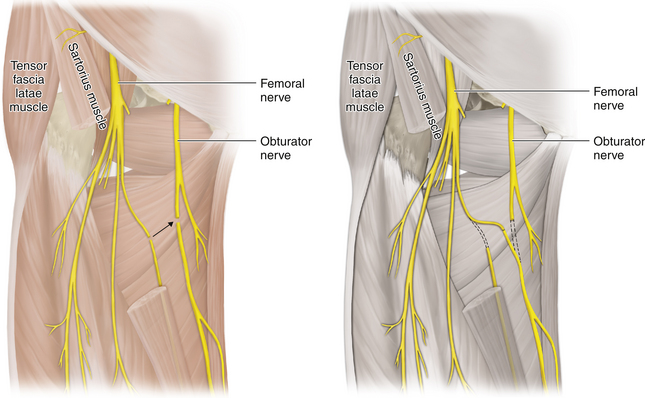
Femoral Branch to Obturator Nerve Transfer (Figure 24-7)6
• A linear paramedian incision is made approximately 2 or 3cm below the right inguinal ligament.
• The obturator nerve is dissected as it exits from the obturator foramen proximally.
• The nerve should be skeletonized and transected at the level of the obturator foramen.
• A small medial branch of the femoral nerve that innervates the proximal portion of the quadriceps muscle and which has approximately the same diameter as the cut end of the obturator nerve should be transected distally.
• The distal end of the femoral nerve branch is then curved inward and passed below the femoral artery and vein. It is then directly sutured to the proximal end of the obturator nerve under microscopic magnification.
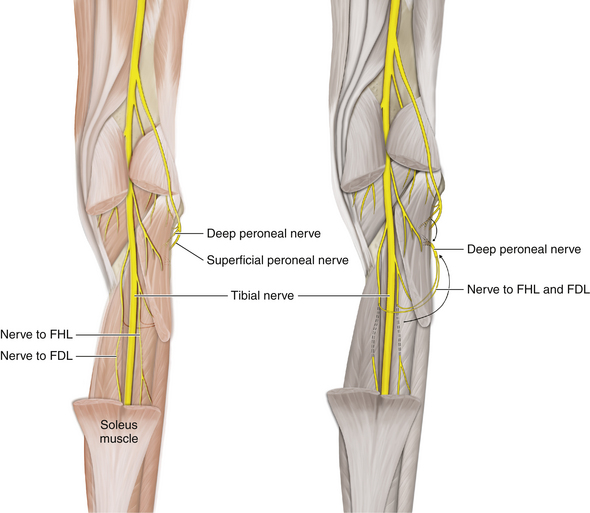
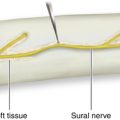
Tibial Nerve Motor Branches (Flexor Hallucis Longus and Flexor Digitorum Longus Muscles) to the Deep Peroneal Nerve Distal to the Bifurcation of the Common Peroneal Nerve (Figure 24-8)7
• The deep peroneal nerve is dissected sufficiently that its most proximal branch to the tibialis anterior muscle can be identified.
• The deep peroneal nerve proximal to this motor branch is selected for nerve transfer.
• Each motor branch from the tibial nerve should be analyzed for adequacy in reaching the target connection site on the deep peroneal nerve.
• Both tibial nerve motor branches are then brought into contact with the deep peroneal nerve.
1. Kawai H., Akita S. Shoulder muscle reconstruction in the upper type of the brachial plexus injury by partial radial nerve transfer to the axillary nerve. Tech Hand Up Extrem Surg. 2004;8(1):51–55.
2. Tung T.H., Mackinnon S.E. Nerve transfers: indications, techniques, and outcomes. J Hand Surg Am. 2010;35(2):332–341.
3. Novak C.B., Mackinnon S.E. Distal anterior interosseous nerve transfer to the deep motor branch of the ulnar nerve for reconstruction of high ulnar nerve injuries. J Reconstr Microsurg. 2002;18(6):459–464.
4. Socolovsky M., Bonilla G., Masi G.D., Bianchi H. Transfer of flexor carpi ulnaris branches to selectively restore AIN function in median nerve sections: Anatomical feasibility study and case report. Surg Neurol Int. 2011;2:102.
5. Mackinnon S.E., Roque B., Tung T.H. Median to radial nerve transfer for treatment of radial nerve palsy. Case report. J Neurosurg. 2007;107(3):666–671.
6. Spiliopoulos K., Williams Z. Femoral branch to obturator nerve transfer for restoration of thigh adduction following iatrogenic injury. J Neurosurg. 2011;114(6):1529–1533.
7. Bodily K.D., Spinner R.J., Bishop A.T. Restoration of motor function of the deep fibular (peroneal) nerve by direct nerve transfer of branches from the tibial nerve: an anatomical study. Clin Anat. 2004;17(3):201–205.