Chapter 23 Nerve Action Potential Recording
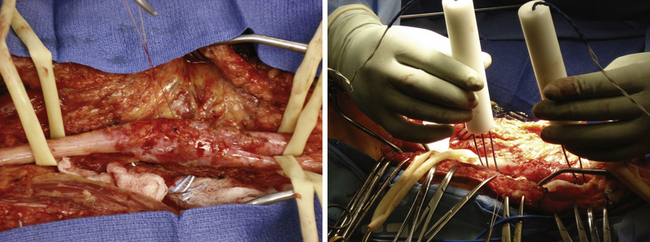
Assessing Distal Motor Function
• After external neurolysis, the next logical step in evaluation of any lesion in continuity is to stimulate the nerve both above and below the lesion, to determine whether there is any motor function distal to the lesion.
• If there is muscle contraction, then enough axons have grown to the muscle in question to provide voluntary contraction, even though the patient may not be able to do it voluntarily at the time of the stimulation.
• If stimulation above gives no muscular contraction distal to the lesion but stimulation below does, there is clearly an element of neurapraxic block involved.
• If a few months have passed since the injury and there is no response, then the lesion is predominantly neurotmetic.
• Alternatively, if the lesion is axonotmetic, either it is too far proximal to meaningful distal muscles to expect adequate regeneration, or it is too early to expect excellent regeneration to have reached them.
• When using stimulation alone, care must be taken not to mistake contraction of muscles proximal to the lesion for distal contractions. One also has to be certain that the current does not spread to adjacent and often more intact muscles or nerves. The muscles seen to contract must be in the distribution of the injured nerve.
• If one records as well as stimulates, the presence or absence of adequate regeneration can be detected relatively early after injury. Nevertheless, several months must elapse for even nerve action potential (NAP) recording to be useful. Thus, after external neurolysis and before internal neurolysis or repair (split or otherwise), we attempt to record NAPs.
Technique
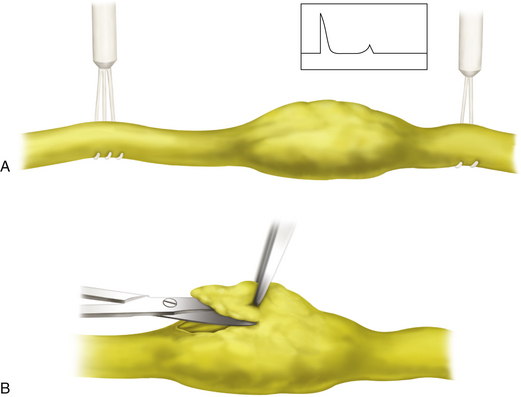
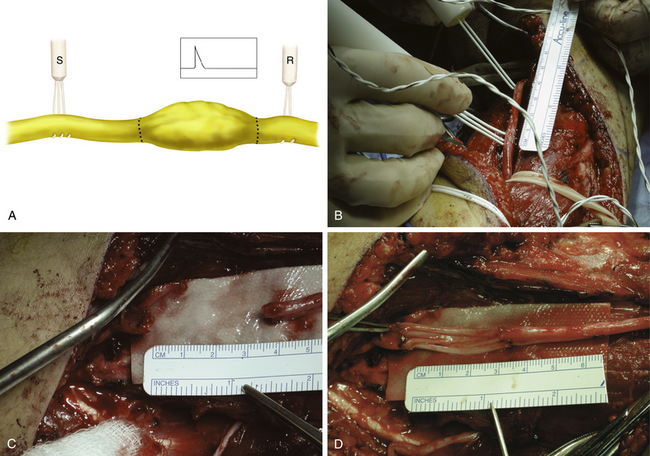
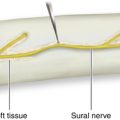
• If the lesion and the requisite surgical exposure permit it, we first record a NAP proximal to or above the lesion. We then move the recording electrodes into and then distal to the lesion to see whether the NAP transmits and how far it travels. Even to record a proximal NAP, the stimulating and recording electrodes need to be separated by at least 3 cm, or 1½ inches (Figure 23-1).
• Muscle action potentials (MUAPs) picked up by recording electrodes can be mistaken for NAPs. Latency is much greater for MUAPs than for NAPs, and responses are larger and much more complex. MUAPs have a relatively broad base and a rounded apex. NAPs can, of course, be recorded without any visible or palpable muscular contraction, whereas sizable MUAPs can seldom be recorded without such.
• When a plexus lesion is close to the spine, stimulation may have to be done close to the lesion, either just proximal or even distal to it, and NAP recording must be done more distally.
• Usually, if a proximal NAP is recorded, we gradually move the electrodes distally and re-record as we go, to see how far a response will be transmitted. Distance between the recording electrode pair should be increased to 5 mm or more when attempting to record from large nerves or when studies are done over a relatively long distance.
Required Equipment
• For stimulation, a tripolar electrode as designed by Happel is preferable to a bipolar one, because it decreases the size and the “runoff” of the stimulus artifact. Brief shocks of 0.05 msec or less are preferable to longer shocks, so a higher voltage is needed than that used for stimulation and recording along longer lengths of nerve, where the stimulus duration can be longer.
• Electrodes are usually made of medical-grade stainless steel and are typically No. 18 in caliber. The tips are bent like shepherd’s crooks so that the nerve can be gently suspended and lifted away from surrounding tissues. We prefer drilled-out Delrin rods as holders for the electrodes.
• The No. 18 stainless steel wire is soldered to the end of insulated wires for eventual plug-in to the stimulating and recording instruments. Because the stimulating and recording electrodes are usually placed relatively close together, the stimulus artifact can be quite large.
• The runoff of this stimulus artifact can obscure NAPs when the distances are relatively short. As mentioned earlier, we prefer a tripolar stimulator. The outermost two electrode tips are a common anode and are interconnected; the middle electrode serves as a cathode. This arrangement tends to limit the longitudinal spread of the current so that the site of stimulation is more precise. It also reduces the size and the runoff of the stimulus artifact.
Troubleshooting Electrodes and Connecting Wires
• Recording of NAPs with bipolar electrodes depends on one recording electrode, usually the initial or more proximal one, being on an active transmitting segment of the nerve and the other being on a less active portion so that a potential difference exists. Thus, if the recording electrode tips are too close together, the amplitude of the evoked NAPs can be reduced, or the NAP may not be recorded at all.
• This is especially so if the distance between the stimulating and recording electrodes is great or if the volume of the nerve being recorded is relatively large. Thus, under such circumstances, the recording tips may have to be separated by more than 5 mm.
• The connecting wires for the electrodes are usually shielded with silicone. Stimulating and recording wires are usually placed well apart to reduce capacitance. We prefer to unplug the Bovie unit, bipolar electrodes, Bair Hugger (used to keep the patient warm), electric heaters, x-ray viewboxes, radios, and other electronic gear to minimize the 60-cycle artifact. If necessary, further grounding can be provided by a lead-out from a Bovie pad placed on the patient to the grounding post of the recording instrument.
Stimulation and Recording Settings
• Both stimulation and recording can be done with the help of an electromyographic (EMG) machine. Most EMG machines manufactured in the last decade or so have more than sufficient stimulation parameters and also differential recording capabilities.
• Frequency filters are usually set at 5 to 10 Hz for the low one and 2500 Hz or higher for the high one. These settings can be changed once an evoked response is present on the screen to optimize it. The stimulating duration is usually 0.05 to 0.10 msec.
• Electrodes are placed beneath and somewhat around the nerve and are usually held in place by hand. The voltage on the stimulating electrode is gradually turned up. The frequency is kept at two to three per second.
• Because the stimulus duration is brief, a relatively high voltage is necessary (20 V or more). Recording amplification is also gradually increased. NAPs, if present, can usually be recorded at amplitude settings between 50µV and 5 mV per division.
• We usually try to record a response proximal to the lesion; then, using these settings as a starting point, we gradually increase them to see whether we can evoke a NAP into and then beyond the lesion in continuity as we move the electrodes distally.
• If a proximal segment of healthy nerve or plexus element is not available, we begin by recording from a more intact nerve or plexus element nearby. These settings are then used as a starting point for the lesioned nerve.
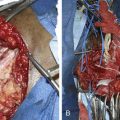
Categorizing the Nerve action potential Response
• The purpose of NAP recording is to see whether a response is conducted beyond the lesion. If so, this would lead to neurolysis rather than lesion resection. In the early months to a year after injury, NAP amplitude and velocity are of interest but are not as critical as whether there is any NAP response at all (Figure 23-2).
• Presence of a NAP indicates axons of sufficient number, caliber, and maturation to presage useful recovery of function for at least a portion of the cross section of nerve (Figure 23-3).
• Absence of a NAP several months after injury indicates a nerve lesion that will not recover without resection and repair.
• NAPs can be blocked or obliterated if the lesion in continuity is handled in a rough fashion, a local anesthetic reaches the nerve, the wound temperature is too low (or less likely, too high), a tourniquet is not released for 15 to 20 minutes before recordings are attempted, or stimulating and recording equipment is broken or faulty.
• A NAP should be recordable not only from the segment of nerve proximal to the injury but also from an adjacent and known intact nerve. If not, then one or more of the preceding sources of difficulty should be sought out.
• Curare-like or other muscle-blocking agents do not interfere with NAP recordings but of course, obscure the results of simple stimulation without recordings.