Chapter 52. Neonatal resuscitation and transport
Cardiac arrest in a neonate (a baby less than 1 month old) may present from:
• A planned home delivery
• An unplanned birth before arrival in hospital
• An infant who has a normal birth and is discharged home and thereafter becomes ill.
The general principles remain the same:
Support of airway (A), breathing (B) and circulation (C).
Neonatal resuscitation
In most instances, the baby born outside hospital will not require any advanced interventions. If the baby is active with a normal respiratory rate and heart rate, then the only treatment required will be to dry and warm the baby, and to use suction as required. A small number of babies will require more active resuscitative measures. Hypothermia is very common and must be avoided, as it leads to poor outcomes.
Meconium
• Fetal distress during labour leads to contamination of the amniotic fluid with meconium from the baby’s gastrointestinal tract
• Wait for the baby to be fully born before applying suction
• The baby will require careful suction after the body is delivered to ensure that no further meconium is aspirated into the trachea and lower airways: the morbidity and mortality rates from meconium aspiration syndrome remain high.
Apgar scores
This system assesses the baby’s overall condition at 1 minute and 5 minutes after birth and later if required. Resuscitative measures should be started immediately, however, and not delayed for evaluation of the Apgar score.
Neonatal basic life support
• The first measure is to stimulate the child. This occurs during drying and warming, and by suctioning of the nasopharyngeal and oropharyngeal passages
• This is often enough to increase the child’s respiratory rate which, as a result of better oxygenation, increases the cardiac rate
• If, after a short period of stimulation, the clinical situation remains grave, the next measure is to maintain the airway by placing the baby in a supine position with the neck in a neutral position, thus avoiding hyperextension (a folded towel under the shoulder can facilitate this)
• Supplemental oxygen via a face mask can be applied, with further suction if copious secretions are present. Again, the hoped-for result is improved respiratory effort and consequently increased cardiac output
• If the neonate fails to respond to these measures it will be necessary to ventilate the baby using a self-inflating bag and mask
• For the neonate, the smallest self-inflating bag is used (usually 240 mL capacity). Care needs to be taken not to overinflate the lungs
• The paramedic should ventilate at a rate of 60 breaths/min for approximately 15–30 seconds. In a newborn, the first few breaths are ‘inflation’ breaths
• The pulse is then checked and if the brachial or femoral pulse rate remains at less than 60/min then chest compressions are started
• The most efficient method of delivering chest compressions is to grip the chest in such a way that the two thumbs can press on the lower third of the sternum, just below an imaginary line joining the nipples, with the fingers over the spine at the back. Compress the chest quickly and firmly reducing the diameter of the chest by one-third
• The sternum should be compressed 100–120 times per minute. The cycle for chest compressions to ventilation is 3 to 1 for a neonate.
Neonatal CPR: 3 compressions to 1 ventilation
Neonatal advanced life support
• If the neonate fails to respond or indeed goes into full cardiopulmonary arrest, more advanced life support techniques are needed
• The paramedic may elect to intubate the child to improve ventilation and to secure the airway against inhalation
• The usual size of an ET tube for a full-term baby is 3–3.5 mm.
ET tube size for a full-term baby: 3 or 3.5 mm (uncuffed)
• The next step is to achieve vascular access either through a peripheral vein or by insertion of an intraosseous needle into the tibia
• Adrenaline is given in asystole or profound bradycardia at a dose of 0.01 mg/kg (0.1 mL/kg) of adrenaline 1 in 10 000 solution intravenously or by the intraosseous route.
Adrenaline dose in neonates is 0.1 mL/kg of 1 in 10 000 solution IV or IO
• In addition to drugs, it is sometimes necessary to give the neonate a fluid challenge of 10–20 mL/kg of normal saline. This treatment is usually carried out during urgent evacuation to hospital
• Care should be taken to maintain the child’s temperature, e.g. by using warm blankets. Always remember to cover the head as well as the body. The back of the ambulance should be kept very warm (uncomfortably hot for the adults).
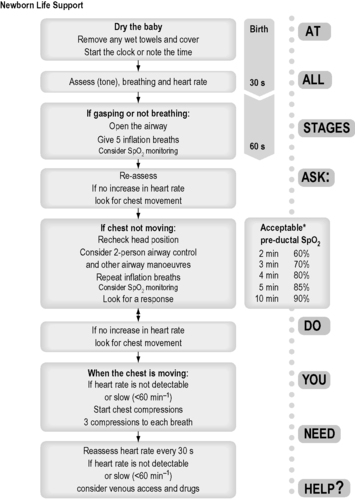 |
| Figure 52.1. |
| Newborn Life Support algorithm (Resuscitation Council UK). The authors are aware of impending changes in resuscitation guidelines (late 2010). Refer to www.resus.org.uk for further up-to-date information. |
Neonatal transport
• Neonatal transfers are common between district general hospitals and specialist neonatal or paediatric units
• Nursing staff and doctors from the peripheral hospital will usually travel with the neonate however some regions send out specialist retrieval teams
• The most important point is that the neonate should be stable prior to transfer
• The whole transfer should be well planned by the sending and the receiving hospitals, so that it is known in advance to which part of the receiving hospital the child is to be taken
• Incubators are used to maintain the child’s temperature during the transfer and possibly to provide ventilation of the neonate
• The incubator operates on a battery supply and requires the use of cylinders of oxygen and air for ventilation. When preparing for such a transfer, it is mandatory to check that sufficient oxygen and battery life are available for the intended journey, allowing some leeway for unforeseen delays or detours
• Most modern incubators can be plugged into the ambulance electrical system, although it is necessary to check that this is the case
• The transport team must have the necessary equipment and drugs available in case the child deteriorates en route
• Facilities for procedures such as reintubation and any other resuscitation techniques such as the reinsertion of intravenous access must be available
• There must be at least one person who can carry out cardiopulmonary resuscitation of the neonate before embarking on the journey.
For further information, see Ch.53 in Emergency Care: A Textbook for Paramedics.