Chapter 10 Neck Rejuvenation
Summary
Introduction
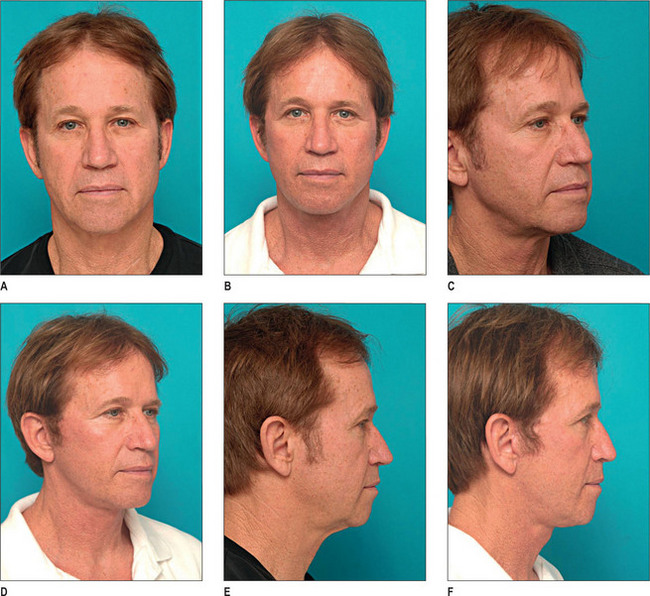
Loss of neck contour, especially at the cervicomental and cervicomandibular angles, is a common sign of aging. Procedures to rejuvenate the face and neck are among the most commonly performed cosmetic surgical procedures in the United States. The delineation of the cervicomandibular angle is an important factor in facial harmony and an overall youthful appearance.1,2 Rejuvenation of the aging neck gives a more pleasing appearance to the soft tissues in that area, and can cause the face to appear more youthful as well. The goal is to provide an even, smooth platysmal layer that closely invests the thyroid cartilage, hyoid, and floor of the mouth. Procedures to lift and redefine the jaw line and submental region are often used as adjuncts to rhytidectomy.
Anatomy and effects of aging
Traditionally, facial rejuvenation techniques have involved repositioning of portions of the superficial musculoaponeurotic system (SMAS) and skin. In the neck the SMAS blends with the platysma fascia to form a continuous sheet.3 Here, signs of cervicofacial aging are initially manifest as faint vertical platysmal bands overlying the thyroid cartilage and hyoid. These then progress to longer, more pronounced bands as more support is lost from the retaining ligaments and the platysma descends further.4 The laxity of the platysma causes a cervical obliquity, which is compounded by supra- and subplatysmal fat deposits. Subplatysmal fat can exacerbate the development of cervicomental angle obliquity. Submandibular gland ptosis may contribute to cervical fullness as well, supplying bulk laterally, below the angle of the mandible. The end result of these processes is a neck with a prematurely aged appearance.
Indications
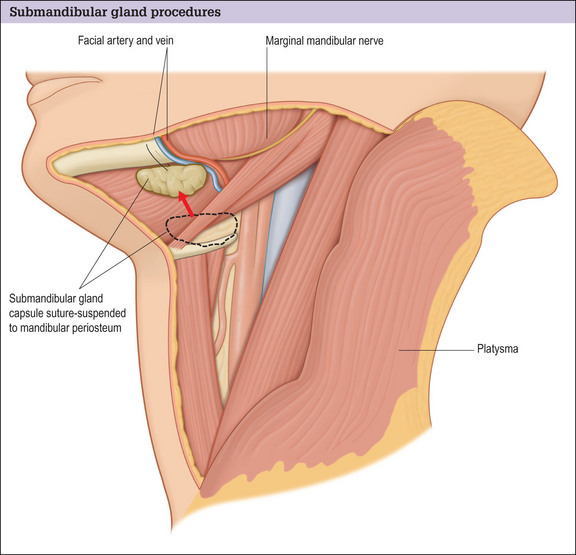
Patients with lesser degrees of submandibular gland fullness may benefit from suspension, whereas those with very significant submandibular gland ptosis or hypertrophy may be candidates for partial resection.6 The idea of aesthetics as an indication for submandibular gland resection, which is a technically challenging operation, is controversial.2,7 The primary criticism for resecting the gland is the risk of nerve injury. Prior to their widespread acceptance, SMAS-rhytidectomy techniques were similarly criticized for their risk to the facial nerve. Through multiple studies documenting the anatomy of the facial nerve and refining the surgical approach to it, SMAS procedures were accepted. Similar studies of the submandibular gland have been undertaken, but controversies remain.4 All of the nerves in the area of the gland, with the exception of the autonomic plexus, are found exterior to its capsule.
Operative Approach
Neck exposure is gained through an inconspicuous 3.5 cm submental incision in the shadow posterior to the submental skin crease. This allows access to the platysmal plane. Laterally the neck is approached through a conventional pre- and posterior auricular rhytidectomy incision, if rhytidectomy is part of the goal. This gives good visualization along the inferior border of the mandible, and provides an avenue for directly visualized suction lipectomy of the lateral neck.
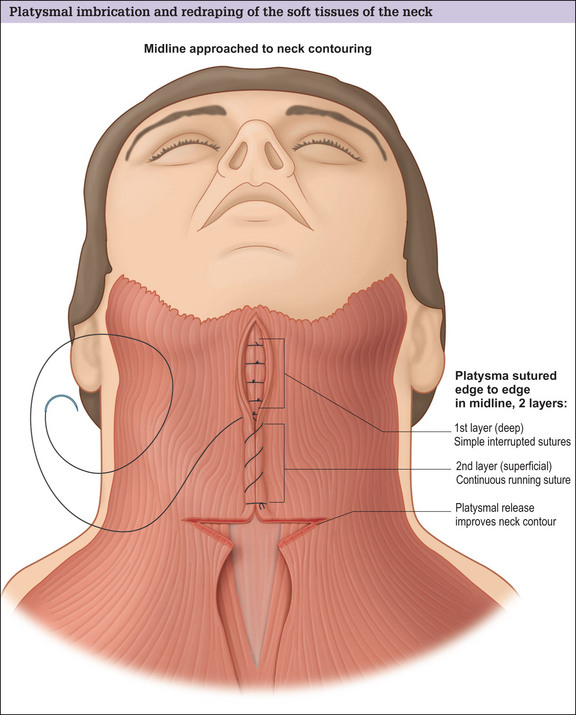
SMAS suspension and platysmal plication
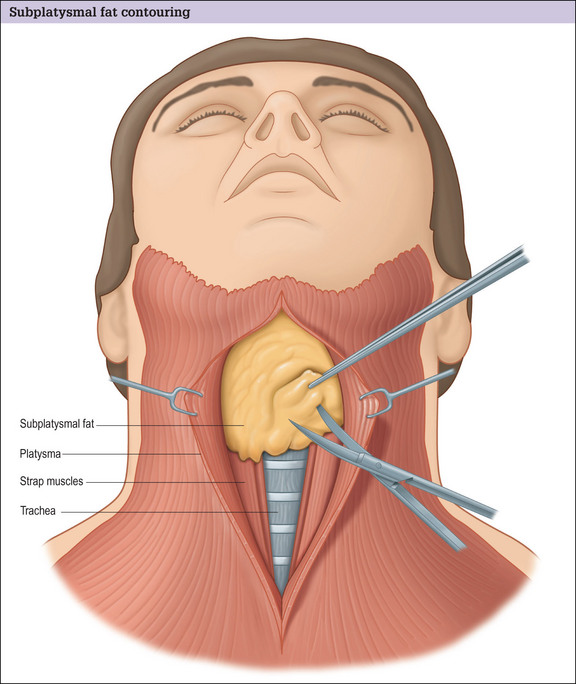
Subplatysmal fat resection
Submandibular gland suspension and resection
The medial to lateral approach to the gland is recommended because it maximally avoids the marginal mandibular nerve, and allows a caudal approach to the gland within the capsule.13 Trying to approach the gland via the submental approach is technically difficult due to limited access and the presence of variant blood supply.
Submandibular resection may be a difficult procedure, but can produce dramatic results in selected patients. Codner and Nahai found that submandibular resection was carried out more often in patients undergoing secondary rather than primary rhytidectomies.11 The resection can be done after careful isolation of the gland, ligation of the facial branches entering the gland and Stenon’s duct. Partial removal can be accomplished with electrocautery.
Submaxillary glands should not be removed from patients who have xerostomia or who wear dentures.
Suction drains using TLS vacuum system may minimize the collection of blood or seromas in the neck.
Optimizing outcomes
Complications and Side Effects
Complication rates for neck rejuvenation procedures are similar to those seen after rhytidectomy. Commonly, the side effects of neck lifts are technical. Intraoperative errors in judgment or technique compromise outcomes, but most adverse outcomes can be avoided with due diligence in preoperative planning and careful meticulous surgery.
Resection of the submandibular gland
The literature supports low complication rates for resection of the submandibular gland.14–17 DePina and Quinta published their experience for eight patients with 12 partially excised submaxillary glands.1,2 Despite occasionally using a direct approach to the gland, rather than the rhytidectomy approach, there were no complications and no salivary fistulas.
1. De Pina D.P. Diagnosis and technical refinements in rhytidectomy: a personal approach. Aesthetic Plast Surg. 1987;1:7-14.
2. De Pina D.P., Quinta W.C. Aesthetic resection of the submandibular salivary gland. Plast Reconstr Surg. 1991;5:779-787.
3. Gardetto A., Dabernig J., Rainer C., et al. Does a superficial musculoaponeurotic system exist in the neck? An anatomic study by the tissue plastination technique. Plast Reconstr Surg. 2003;111(2):664-672.
4. Stuzin J.M., Baker T.J. Aging face and neck. In: Stephen Mathes, editor. Plastic surgery. 2nd edn. Philadelphia: Elsevier; 2006:159-214.
5. Sullivan P.K., Freeman M.B., Schmidt S. Contouring the aging neck with submandibular gland suspension. Aesthetic Surg J. 2006;26(4):465-471.
6. Marten T.J. Submandibular gland resection in rejuvenation of the aging neck. American Society for Aesthetic Plastic Surgery, May 2001.
7. Baker D.C. Face lift with submandibular gland and digastric muscle resection: radical neck rhytidectomy. Aesthetic Surg J. 2006;26:85-92.
8. Zins J.E., Fardo D. The ‘anterior-only’ approach to neck rejuvenation: an alternative to facelift surgery. Plast Reconstr Surg. 2005;115(6):1761-1768.
9. Goddio A.S. Skin retraction following suction lipectomy by treatment site: a study of 500 procedures in 458 selected subjects. Plast Reconstr Surg. 1991;87(1):66-75.
10. Adamson P.A., Cormier R., Tropper G.J., et al. Cervicofacial liposuction: results and controversies. J Otolaryngol. 1991;19(4):267-273.
11. Codner M.C., Nahai F. Submandibular gland I: an anatomic evaluation and surgical approach to submandibular gland resection for facial rejuvenation. Discussion. Plast Reconstr Surg. 2003;112(4):1155-1156.
12. Connell B.F., Shamoun J.M. The significance of digastric muscle contouring for rejuvenation of the submental area of the face. Plast Reconstr Surg. 1997;99(6):1586-1590.
13. Singer D.P., Sullivan P.K. Submandibular gland I: an anatomic evaluation and surgical approach to submandibular gland resection for facial rejuvenation. Plast Reconstr Surg. 2003;112(4):1150-1154.
14. Ballenger J.J., Snow J.B. Otolaryngology head and neck surgery, 15th edn. Baltimore: Williams & Wilkins, 1996.
15. Cummings C.W. Otolaryngology head and neck surgery, 3rd edn. St Louis: Mosby-Year Book, 1998.
16. Ramirez O.M. Comprehensive approach to rejuvenation of the neck. Facial Plast Surg. 2001;17:129-140.
17. Sinha U.K., Ng M. Surgery of the salivary gland. Otolaryngol Clin North Am. 1999;32:887-906.
Feldman J.J. Corset platysmaplasty. Plast Reconstr Surg. 1990;85:333.