Near Drowning
After reading this chapter, you will be able to:
• List the anatomic alterations of the lungs associated with near drowning.
• Describe the causes of near drowning.
• List the cardiopulmonary clinical manifestations associated with near drowning.
• Describe the general management of near drowning.
• Describe the clinical strategies and rationales of the SOAPs presented in the case study.
• Define key terms and complete self-assessment questions at the end of the chapter and on Evolve.
Anatomic Alterations of the Lungs
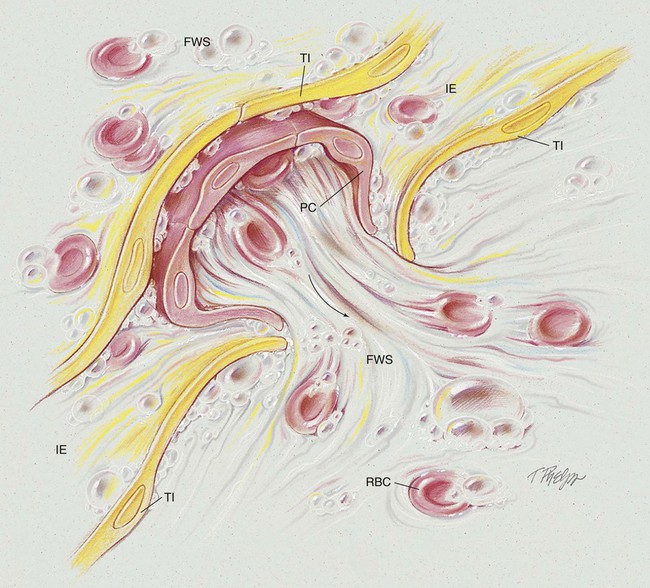
Finally, if the victim was submerged in unclean water (e.g., swamp, pond, sewage, or mud), a number of pathogens (e.g., Pseudomonas) and solid material may be aspirated. When this happens, pneumonia may occur, and in severe cases, acute respiratory distress syndrome (ARDS) may develop. Although the theory has been controversial in the past, it is now believed that the major pathologic changes of the lungs are essentially the same in fresh water and sea water wet drownings; both result in a reduction in pulmonary surfactant, alveolar injury, atelectasis, and pulmonary edema (see Figure 40-1).
The major pulmonary pathologic and structural changes associated with wet drowning are as follows:
• Interstitial edema, including engorgement of the perivascular and peribronchial spaces, alveolar walls, and interstitial spaces
• Decreased pulmonary surfactant with increased surface tension of alveolar fluid
• Frothy, white and pink secretions throughout the tracheobronchial tree
Etiology and Epidemiology
Box 40-1 summarizes the general sequence of events that occurs in drowning or near drowning. Victims submerged in cold water generally demonstrate a much higher survival rate than victims submerged in warm water. Table 40-1 lists favorable prognostic factors in cold-water near drowning.
TABLE 40-1
Favorable Prognostic Factors in Cold-Water Near Drowning
| Age | The younger, the better |
| Submersion time | The shorter, the better (60 minutes appears to be the upper limit in cold-water submersions) |
| Water temperature | The colder, the better (range, 27° F to 70° F) |
| Water quality | The cleaner, the better |
| Other injuries | None serious |
| Amount of struggle | The less struggle, the better |
| Cardiopulmonary resuscitation (CPR) quality | Good CPR technique increases the survival rate |
| Suicidal intent | Lower survival rate among victims who attempted suicide than among victims of accidental submersion |
CASE STUDY
Near Drowning
Admitting History and Physical Examination
Respiratory Assessment and Plan
S N/A (patient comatose). History of near drowning.
O Comatose. Spontaneous breathing at 10/min, BP 100/60, P 140. Crackles bilaterally. Nasotracheal suctioning yields clear fluid. Cyanotic. Spo2 on 5 L/min O2 per nasal cannula: 72%.
• Near drowning. R/O seizure disorder (history)
• Increased airway secretions (suctioning of clear fluid)
P Stat ABG on 100% oxygen, then titrate per Oxygen Therapy Protocol. Have equipment to intubate on standby. Bag-mask ventilate, and suction. Provide continuous pulse oximetry. Continue nasotracheal suctioning. Take seizure precautions. Will accompany on transfer.
Respiratory Assessment and Plan
S Anxious, dyspneic, crying. “I can’t get my breath. Where am I? Am I going to die?”
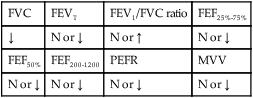
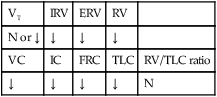
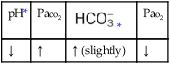
O Afebrile. BP 112/70, P 140/min, RR 60/min. Cyanotic. Paradoxic chest/abdomen movements, sternal retraction. Crackles in both lungs anteriorly. Spontaneous cough with frothy sputum production, WBC 21,000/mm3. On 80% oxygen: pH 7.29, Paco2 52,  25, Pao2 38. CXR: “White-out.”
25, Pao2 38. CXR: “White-out.”
• Pulmonary edema secondary to near drowning (frothy sputum)
• Acute ventilatory failure with metabolic acidosis (likely lactic acid) with severe hypoxemia (ABGs)
P Place on 100% O2 and bag-mask ventilate. Page physician stat. Obtain intubation equipment and prepare to place patient on ventilator. Follow oximetry. Prepare to assist in placement of Swan-Ganz catheter.
Respiratory Assessment and Plan
S N/A (patient sedated, paralyzed)
O Lungs clear. No secretions. On 50% O2 and +10 PEEP: pH 7.42, Paco2 42,  24, and Pao2 98. CXR: Considerable improvement in bilateral infiltrates.
24, and Pao2 98. CXR: Considerable improvement in bilateral infiltrates.
• Considerable improvement on CMV and PEEP (general improvement of clinical indicators)
• Acceptable ventilation and oxygenation status on present ventilatory settings (ABG)
• Frothy airway secretions no longer present (clear lungs and no secretions)
P Contact physician to wean from muscle relaxant. Wean from mechanically ventilated breaths, Fio2, and PEEP per Mechanical Ventilation Protocol. Change ventilator mode to synchronized intermittent mandatory ventilation (SIMV).
Discussion
This case demonstrates initial worsening of the near drowning victim despite intensive respiratory care. The initial ABG values showed severe hypoxemia as a result of Increased Alveolar-Capillary Membrane Thickness and alveolar flooding (see Figures 9-10 and 40-1), as well as acute ventilatory failure and metabolic (probably lactic) acidosis. Bronchospasm never developed, and aggressive respiratory care prohibited the development of atelectasis and aspiration pneumonia.


 values will be lower than expected for a particular Pa
values will be lower than expected for a particular Pa



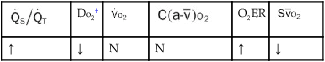
 , Arterial-venous oxygen difference; DO2, total oxygen delivery; O2ER, oxygen extraction ratio;
, Arterial-venous oxygen difference; DO2, total oxygen delivery; O2ER, oxygen extraction ratio;  , pulmonary shunt fraction;
, pulmonary shunt fraction;  , mixed venous oxygen saturation;
, mixed venous oxygen saturation;  , oxygen consumption.
, oxygen consumption.
 25, and Pa
25, and Pa 24, and Pa
24, and Pa 24, and Pa
24, and Pa 23, and Pa
23, and Pa