CHAPTER 35 Nasal Fractures
The prominence and delicate structure of the nose make it vulnerable to a broad spectrum of injury, which accounts for why it is the most frequently fractured facial bone.1–11 Sports, falls, and assaults are the usual mechanisms responsible for the majority of nasal fractures, with alcohol consumption being an important contributing factor in many cases.7,8,12–19 Males are affected approximately twice as often as females in both the adult and pediatric populations, with a peak incidence occurring during the second and third decades of life.8,12,13,15,17,20,21 Deformity, swelling, epistaxis, and periorbital ecchymosis are signs that are suggestive of nasal fracture, whereas bony crepitus and nasal segment mobility are diagnostic.
Anatomy
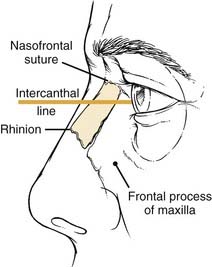
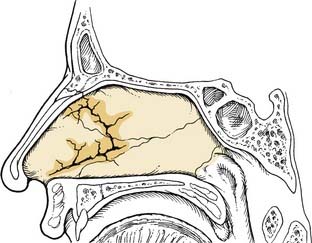
The bony vault is a pyramid-shaped structure that is composed of paired nasal bones centrally and the frontal processes of the maxilla laterally. Ossification of these bones via intramembranous bone formation starts at the end of the third trimester and continues for years after birth.22 Superiorly the thickness of the nasal bones is greater above the level of the intercanthal line as they taper upward toward the nasofrontal suture. Below the intercanthal line, the thinner nasal bone projects anteriorly to join with the upper lateral cartilages at an externally defined midline point known as the rhinion (Fig. 35-1). On the inner surface of the nose, the perpendicular plate of the ethmoid fuses in the midline with the nasal bones to provide additional support to the nasal pyramid; this construct creates a tent-like structure, with the ethmoid plate representing a pole and the nasal bones representing the side walls of the tent. This interrelationship helps explain the susceptibility of the septum to injury by the transmitted forces from the external nose to the perpendicular plate of the ethmoid (Fig. 35-2).
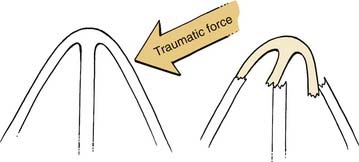
Figure 35-2. Transmitted forces from a lateral nasal bone impact resulting in fracture of the perpendicular plate of the ethmoid.
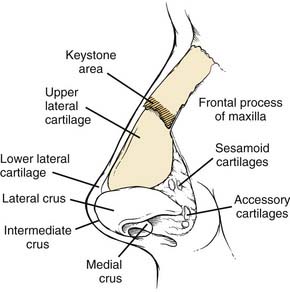
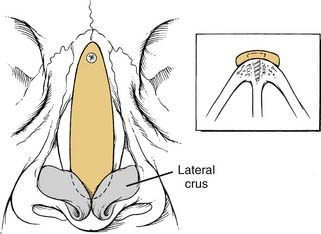
The midportion of the nose is composed of the upper lateral cartilages and the dorsal segment of the quadrangular cartilage. Made up of hyaline cartilage, these structures are fused as a single unit, with only the lower third separated by fibrous tissue.23 The cephalic ends of the upper lateral cartilages are overlapped by the nasal bones by as much as 11 mm and secured with a solid fibrous union referred to as the keystone area (Fig. 35-3).24 Laterally the upper lateral cartilages do not articulate with the bony pyramid; rather, they are attached to the frontal process of the maxilla by a fibrous aponeurosis in which the sesamoid cartilages can be found. Therefore, the preservation of the attachments of the upper lateral cartilages with the nasal bone and the septum is crucial to prevent destabilization.
The lower third of the nose is formed primarily by the alar cartilages in addition to the accessory cartilages and fibrous fatty connective tissue that define the nostrils laterally. The alar cartilages are bilobed structures composed of medial and lateral crura with an intervening middle segment (intermediate crus) that has an important role in the definition of the nasal tip. These cartilages are interconnected as a single unit by transverse, fibrous connective tissue called the interdomal ligament.25 Structural support is mainly provided by the scrolled, overlapped upper portion of the lateral crus with the lower border of the upper lateral cartilage and the medial crural attachment with the caudal septum. The dermocartilaginous ligament, which originates from the superficial fascia of the superior nose, inserts into the intermediate crus and caudal septum to provide additional tip support.26
The septum is a key element of the structure of the entire nose. The posterior bony septum is made up of the perpendicular plate of the ethmoid superiorly and the wedge-shaped vomer inferiorly. Smaller contributions from the nasal crests of the palatine bones and the maxilla underlie the vomer and terminate anteriorly at the nasal spine. Extending anteriorly toward the nasal spine, the superior edges of the vomer and nasal crest of the maxilla form a bony groove in which a thickened inferior portion of the quadrangular cartilage lies. This articulation represents the basal foundation upon which all of the overlying nasal structures rest. Mobility of the cartilage within the groove helps prevent septal fractures by allowing for slight lateral rotation during compression of the septum.25 A thickened osteocartilaginous buttress along the septoethmoid junction is the main strut for the bony and cartilaginous dorsum, whereas a thick caudal septum provides the majority of the nasal tip support.
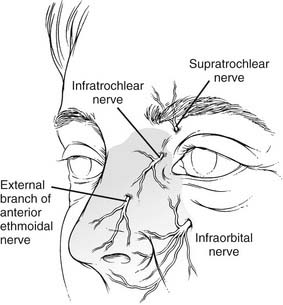
The sensory innervation of the nose is supplied by the first two divisions of the trigeminal nerve. The supratrochlear, infratrochlear, and external branches of the anterior ethmoid nerves (V1) provide sensation to the upper, dorsal, and nasal tip surfaces, whereas the infraorbital nerve (V2) supplies sensation to the side walls (Fig. 35-4). Internally along the lateral nasal wall, the anterior and posterior ethmoidal nerves provide sensation to the upper portions of the nasal cavity. The sphenopalatine ganglion (V2), which originates at the end of the middle turbinate, provides innervation throughout the posterior nasal cavity. Branches from anterior and posterior ethmoid nerves and the sphenopalatine (nasopalatine) nerve cross over superiorly and posteriorly to provide sensation to the majority of the septum.
Pathophysiology
Understanding the process by which nasal fractures occur and how injuries to key areas of support can alter appearance and function are essential to appropriate treatment. Variables such as force, impact direction, nature of the striking object, patient’s age, and other host factors will influence the pattern of injury to both the bony and cartilaginous components of the nose. Younger adults often suffer the dislocation of major segments, whereas older individuals tend to have more comminution of brittle, osteopenic nasal bones.27 Children, on the other hand, have more cartilaginous injuries and greenstick fractures due to a greater proportion of nasal cartilage and the incomplete ossification of nasal bones.9
A combination of the projection of the nose and its relatively fragile supporting structures as compared with other facial bones make it particularly susceptible to fracture. The thinner nasal bone below the intercanthal line, which projects more prominently from the face, is fractured much more easily than the thicker bone of the nasal root above the line. Lateral forces may produce an ipsilateral depressed fracture or may outfracture the opposite nasal bone, thereby resulting in significant deviation of the entire nose. Although lateral forces are a more frequent cause of nasal injuries,3 deviated fractures can occur from either frontal or laterally directed impacts as well.28
The cartilaginous portions of the external nose are able to absorb a greater amount of force without fracture as compared with the bony components, but they are still susceptible to injury given their greater exposure. Avulsion and dislocation of the upper lateral cartilage from the nasal bone and septum will result in a hollowed-out appearance of the midportion of the nose.24 This injury may also tear the external nasal artery as it exits between the nasal bone and upper lateral cartilage, thereby causing a dorsal hematoma.29 In cases of severe frontal trauma, reduction of nasal projection and increased nasal tip rotation are indicative of fracture and telescoping of the cartilaginous portions of the anterior nose and caudal septum.30
Septal injury is one of the most crucial elements of nasal deformity and dysfunction. The thinnest portions of the septum that tend to fracture most readily are located around the superior septal angle, the central-dorsal area of the quadrangular cartilage, and the posterior portion of the perpendicular ethmoid plate. Cadaver studies done both by Harrison28 and Murray and coworkers18 found that either frontal or lateral forces produced a consistent C-shaped fracture through the cartilaginous septum and perpendicular plate. Failure to reduce these septal fractures has been shown to be responsible for many cases of decreased nasal projection and lateral deviation found after unsuccessful attempts at closed reduction.18 Transmitted impact forces from the nasal bones and upper lateral cartilages can also result in septal dislocation off the maxillary crest, thus further destabilizing overlying structures and aggravating airway obstruction. Incomplete fracture of the septal cartilage was hypothesized by Fry30A to cause the release of “interlocked stress” within the cartilage, which leads to further deformity.
Associated Injuries
Injury to the structures that surround the nose often occurs in cases of high-velocity impacts, such as those sustained in motor vehicle accidents. Epiphora from disruption of the nasolacrimal drainage system occurs with 0.2% of nasal fractures.31 Severe injuries with fracture of both the lacrimal bones and the ethmoidal complex are associated with depressed nasal fractures from frontally directed forces.27 Widening of the intercanthal distance caused by the detachment of the medial canthal tendons is a classic appearance of these fractures, and these are better known as nasal-orbital-ethmoid complex fractures. Hard palate instability and open bite deformity are signs of Le Fort’s fracture, whereas unilateral malar deformity and facial asymmetry suggest a zygomaticomaxillary complex fracture. Significant trauma to the upper portions of the facial skeleton may be associated with frontal sinus fracture, cribriform plate fracture, and dural tears leading to pneumocephalus and cerebrospinal fluid rhinorrhea.32
Classification
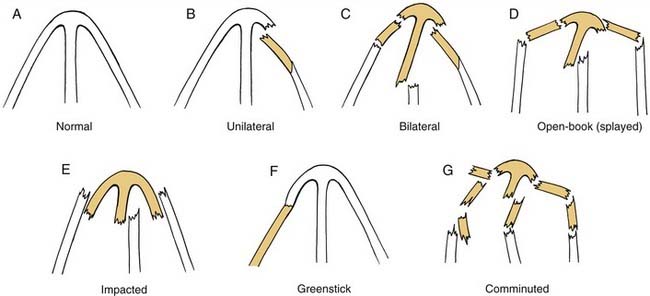
Due to the variations in individual anatomy and trauma etiology, there are several different types of nasal injuries that may be encountered. Fractures of the bony pyramid may be described as unilateral, bilateral, comminuted, depressed, open-book (splayed), impacted (telescoped), and greenstick (Fig. 35-5). Septal damage should also be documented for fractures that have caused deviation or dislocation off the maxillary crest. The extension of fractures to involve surrounding structures such as the maxilla, lacrimal bone, ethmoid complex, or frontal sinus should be included in the description as well.
Although there have been many attempts to apply an all-encompassing classification scheme to nasal fractures, the wide variety of injuries has precluded the acceptance of a single system that has practical application. Anatomic descriptions of nasal injuries often focus on the fracture pattern of the nasal bones but do not include cartilaginous components4 or do not describe the involvement of surrounding structures.28 Murray and Maran8 attempted to narrow down fractures of the nasal bones and septum to seven anatomic groupings using data collected from cadaver experiments. Although their publication is popularized for highlighting the importance of septal management to the overall success of reduction, the classification has not been widely accepted because of its complexity.
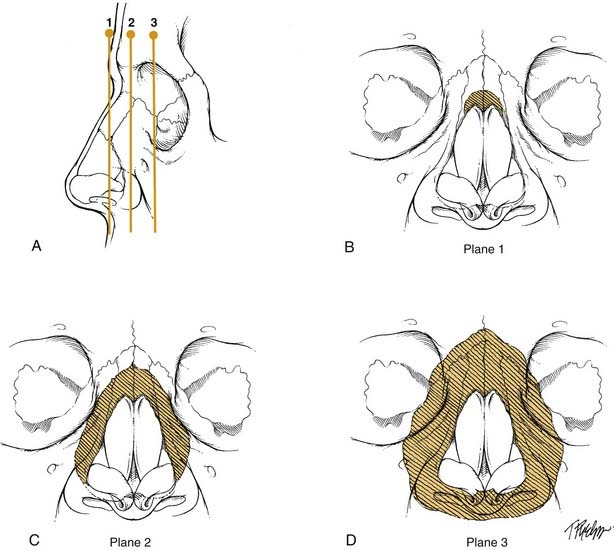
The other broad method of categorization is based on the direction of the impact force. Lateral-type injuries, which are more common, tend to have less severe damage and a better prognosis than the frontal types.27,33 Stranc and Robertson33 developed a classification system using these two main groups, with further breakdown of the frontal type into three different planes that are determined by the depth of injury from the nasal tip (planes 1 through 3) (Fig. 35-6). Each successive plane is associated with a higher likelihood of residual deformity after reduction. Plane 1 injury includes damage to the anterior nasal spine, the anterior septum, or the lower ends of the nasal bones. Dislocation and telescoping of the upper lateral cartilages and septum may be found with a plane 1 injury. Plane 2 injury results in more extensive damage to the nasal bones and ascending maxillary process but does not involve the orbital rims. The septum has a significant amount of deviation and may lack stability to support the nasal dorsum. Plane 3 injury results in nasal-orbital-ethmoid complex disruption. Patients with this injury are usually found to have other midface and cranial base fractures; the nasal bones and septum are severely comminuted and overlapped. Surgery for plane 3 injuries often is unable to fully restore the preexisting nasal appearance and function, particularly if the orbital-ethmoid complex components of the injury are not recognized and treated properly. These conclusions were supported in a study by Daw and Lewis3 that showed a significantly higher incidence of residual anatomic and functional defects in frontal injuries as compared with lateral injuries.
Diagnostic Assessment
History
A detailed account of the events surrounding nasal trauma is helpful in determining the type and severity of injuries that may be present. In cases of motor vehicle accidents, information about the speed, direction of impact, and the presence of restraining devices should be obtained. Young children who are located in the front passenger seat are at risk for head and cervical injuries related to airbag deployment, even in incidences of low-speed collisions. Patients who present after an assault should be questioned about the nature of the striking object and the direction of the blows. It is important to note that up to 30% to 60% of women with facial trauma as a result of assault are victims of domestic violence.34,35
In addition to changes in appearance, the patient history should be evaluated for functional changes in nasal breathing and smell as well as bleeding and watery drainage with a sweet/salty taste (possible cerebrospinal fluid [CSF] leak). Although loss of smell should be documented, poor nasal airflow as a result of edema is almost always present at the initial interview and therefore sense of smell should be reassessed after swelling has diminished. Persistent anosmia or hyposmia may occur in as many as 5% of individuals who suffer head injury with or without nasal trauma and has been observed to resolve spontaneously in only a third of cases.36
A review of a patient’s medical history includes any prior nasal injury, deformity, surgery, dyspnea, allergies, or sinus disease. Individuals who have had prior rhinoplasty are more susceptible to nasal fracture, even after complete healing.37 Old photographs or detailed descriptions of previous nasal deformities should be assessed for significant changes; up to 40% of normal individuals without a history of nasal trauma have evidence of significant malformation.7 A complete review of systems should also screen for associated trauma (e.g., ophthalmic or cervical spine injuries).
Physical Examination
Before the evaluation of internal structures, all necessary equipment and medications for the examination should be ready at the bedside, including materials to control epistaxis. Using a headlight and a nasal speculum, clotted blood is removed with a Frazier suction to visualize all mucosal surfaces for evidence of mucosal tears, hematoma, and active bleeding. The use of topical decongestants will aid visualization and help control bloody oozing. The septum is carefully evaluated for any abnormal soft-tissue swelling that is indicative of a hematoma. Bimanual palpation of the septum with cotton-tipped applicators helps differentiate hematoma, which tends to be more compressible than tissue edema. Areas of increased mobility are suggestive of septal fracture. The use of a 0- or 30-degree 4-mm rod telescope is particularly helpful to assess for posterior septal abnormalities and localization of occult bleeding sources. Although fracture and dislocation of the nasal septum is a common occurrence with nasal trauma, up to 50% of normal individuals without a history of significant nasal injury have a deviated nasal septum.6
If the patient can be examined while heavily sedated, a more complete assessment of the condition of the supporting nasal structures is possible. The Brown-Gruss provocation maneuvers break down the analysis of the infrastructure of the nose into upper, middle, and lower segments by applying digital pressure over each of the compartments.38 Lower vault compression (Brown-Gruss III) may show hyperrotation of the nasal tip with disruption of the septal angle or inward collapse if the supporting caudal septum is severely fragmented. Middle vault compression (Brown-Gruss II) will produce a saddle deformity when the central portion of the septum has been damaged. Upper vault compression (Brown-Gruss I) will cause collapse of the upper third of the nose in cases with severe comminution of the nasal bones and frontal processes of the maxilla. Complex fractures with two or more involved vaults will show more extensive collapse or even complete disappearance of the nose in cases in which severe trauma has affected all three vaults.
Radiography
Despite clear evidence that plain films do not have a role in the management of nasal fractures, these studies are frequently obtained to evaluate individuals after nasal trauma. An investigation by de Lacey and others39 found that plain films had a 66% false-positive reading as a result of the misinterpretation of normal suture lines or developmental thinning of the nasal bones. It is also difficult to distinguish old fractures from new ones on plain films, because only 15% of nasal bone fractures heal by ossification.40 These studies are further limited by their inability to detect cartilaginous injuries, which are more prevalent in pediatric cases. Logan and colleagues16 found that, out of 100 consecutive patients presenting with nasal trauma who had undergone nasal radiography, in no case did the plain film alter management. The diagnosis and proper treatment of the majority of nasal injuries should be successfully achieved with the use of the history and physical findings alone.
However, in cases involving more severe trauma and in which there is physical evidence of other facial fractures, computed tomography should be employed to assess the extent of bony injury. Thin cut coronal and axial views are most appropriate for the evaluation of midfacial, orbital, and frontal sinus fractures. For extensive injuries involving the nasal-orbital-ethmoidal complex, a combination of both two- and three-dimensional computed tomography is recommended for the localization of fractures and the spatial orientation of displaced fragments.41
Management
Acute Intervention
Epistaxis from nasal trauma may range from minor mucosal oozing to life-threatening, large-vessel hemorrhage. Treatment of bleeding that is not responsive to topical vasoconstriction should first be localized. Anterior sources may be cauterized with silver nitrate or sealed with topical materials such as thrombin combined with gelatin foam, FloSeal, fibrin glue, or other procoagulant substances. Formal anterior packing with an inflatable tampon or ribbon gauze is placed if more conservative measures fail. For cases in which skull base fractures may exist, caution should be used with pack placement to avoid an iatrogenic, intracranial injury. Bleeding from branches of the sphenopalatine or ethmoid vessels requires anterior-posterior packing followed by several days of close respiratory monitoring. Alternatively, initial treatment with surgical methods, such as direct endoscopic cauterization or vessel ligation, have been shown to offer better hemostasis, less patient discomfort, and less cost than management with packing.42 Angiography with embolization can also be considered.
Timing of Reduction
Appropriate timing is essential to obtaining the best realignment possible. The development of fibrous connective tissue within the fracture line becomes the limiting factor for successful reduction starting at around 10 days to 2 weeks after injury. Ideally, manipulation should be performed before this point, with some preference before 10 days43; however, some authors have suggested that attempts to reduce nasal fractures can be done as far out as 3 weeks.29 A short delay period is also recommended during the first 2 to 3 days to allow for diminution of swelling so that the nasal bone position may be best appreciated. Treatment before this delay is reasonable if the patient presents within an hour or two after injury, before edema has obscured the underlying structure.
Open versus Closed Reduction
Many of the studies that have supported closed nasal reduction as the primary modality of treatment use patient opinion to gauge results. A study by Crowther and O’Donoghue2 found that 85% of a group of 85 patients treated with closed reduction were satisfied with appearance, and only 9% later requested septorhinoplasty. These results were similar to those of a prospective study published by Illum,6 who found that, out of a total of 88 patients, 91% were satisfied at 3 months, 87% were satisfied at three years, and only 3% were interested in secondary corrective treatment. Although in the latter study 35% of patients had evidence of nasal deformity found during a follow-up examination by the physician, this was not a significant difference from a control group of 80 normal patients. Crowther and Illum both concluded that closed nasal reduction alone is adequate treatment for most nasal fractures and that only a limited number of delayed open septorhinoplasty procedures are necessary.
However, the success rates of studies that were reported in terms of physician observations have been quite different. A summary of 13 different publications that analyzed the outcomes of closed reduction found that, overall, 79% of patients were satisfied with their appearance versus only 37% of surgeons who thought the reduction was successful.44 Although there is no clear explanation for this disparity, it has been the reason for many surgeons to look for better results in their management of nasal fractures.
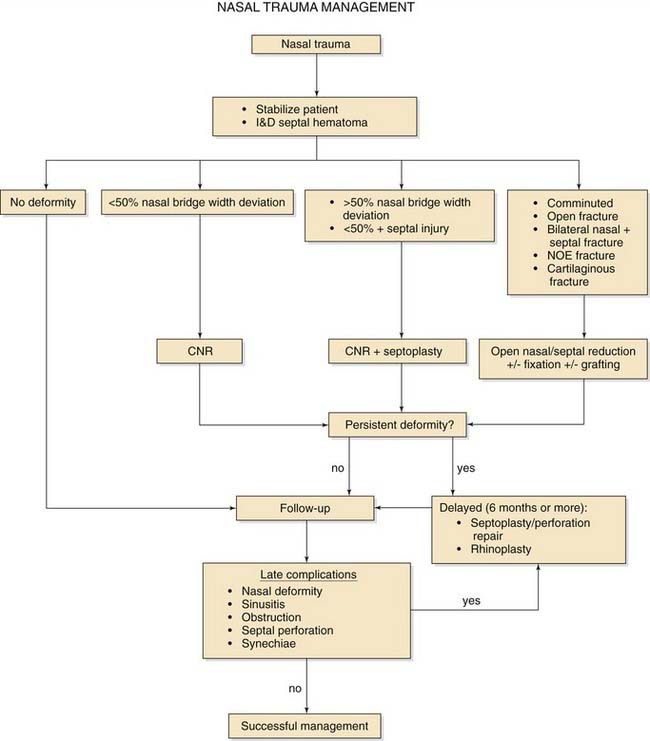
One of the most important reasons for the failure of closed nasal reduction is concurrent nasal septal fracture. Murray and Maran8 prospectively evaluated 756 consecutive nasal trauma patients and found a 30% to 40% incidence of residual deformity in patients treated with manipulation on the basis of an examiner’s score, regardless of the etiology, timing of manipulation, surgeon’s skill, type of anesthetic, or method of postoperative fixation. The authors indicated that such a uniformly high failure rate was most likely the result of poor understanding of fracture pathophysiology, so a cadaver study was designed to analyze patterns of nasal injury.18 The results showed a consistent C-shaped septal fracture (Fig. 35-7) for cases in which the external nose was deviated by at least half of the nasal bridge width; this pattern was identical to one that was found by Harrison28 in an earlier published cadaver experiment. Murray and Harrison both hypothesized that the interlocking of the septal fracture was responsible for creating tension that caused nasal bone displacement. In the same article by Murray and coworkers,18 a prospective analysis of 160 patients showed that resection of the septum along the C-shaped fracture combined with closed nasal reduction resulted in significantly better appearance as compared with manipulation alone. Murray and colleagues concluded that septoplasty plus closed nasal reduction is the treatment of choice in cases of deviation of at least half the bridge width and that, for less severe injuries, manipulation alone is sufficient.
The use of open surgical reduction has also been advocated for many commonly encountered nasal fractures.9,45 Although it is argued that the superior exposure afforded by these procedures produces better long-term results,45 there has not been much evidence to support these conclusions. Other surgeons have shown possible benefits of using a stepwise protocol of advancing from closed nasal reduction to progressively more invasive open surgical techniques until adequate nasal form and patency are achieved.44 The disadvantages of using open reduction for the majority of nasal fractures are the higher treatment costs and the increased risk of surgical complications. Ideally open surgical reduction should be limited to those cases in which it would yield significantly better results than more conservative measures to justify the drawbacks. Verwoerd’s29 outline of what he considered to be the indications for open reduction includes the following: (1) bilateral fractures with dislocation of the nasal dorsum and significant septal pathologic changes; (2) bilateral fractures with major dislocation with or without significant septal pathologic states; (3) infracture of the nasal dorsum; and (4) fractures of the cartilaginous pyramid without mobilization of the bony nasal dorsum and with or without dislocation of the upper lateral cartilages. Although using an algorithm to determine the need for operative intervention is convenient (Fig. 35-8), it should not replace clinical judgment on an individualized basis.
Anesthesia for Closed Reduction
Proper pain management has become a critical topic since the publication of the 2000-2001 standards manual by the Joint Commission on Accreditation of Healthcare Organizations.46 As a result, practitioners are subject to greater expectations to ensure that procedures will not cause undue discomfort to their patients. This expectation may have the effect of increasing the demand for general anesthesia during the performance of nasal reductions. However, this degree of pain control may not always be feasible as a result of medical risk factors, scheduling conflicts, or operating room availability. Therefore, the surgeon must consider alternative anesthetic options so that he or she provides the most appropriate pain control without sacrificing timely management.
A well-administered local nasal block provides excellent anesthesia for the majority of reductions that require both septal and nasal bone manipulation. Studies have shown that the frequency of successful nasal reduction is similar regardless of the use of either general or local anesthesia.21,47,48 The most common method of performing a nasal block is through a combination of topical and injected anesthetic. Cotton pledgets soaked with either 4% cocaine or 0.05% oxymetazoline combined with 4% topical lidocaine are placed strategically throughout the nasal cavity to cover branches of the anterior and posterior ethmoid, sphenopalatine, and nasopalatine nerves. After 5 to 10 minutes, the pledgets are removed, and 1% lidocaine with 1 : 100,000 epinephrine is injected along the septum, lateral walls, and floor of the nasal cavity. The external nasal branch is blocked via an intercartilaginous injection of the dorsum from the rhinion to the supratip region. Through the vestibule, the needle tip is passed into the facial soft tissue to a point just below the midportion of the orbital rim to anesthetize the infraorbital nerve. Branches from the nasopalatine nerve are then blocked with an injection at the base of the columella and nasal tip just inside of the nasal sill. After infiltration of the contralateral side in a similar fashion, the topical-soaked pledgets are replaced posteriorly along the deep internal nasal branches for 5 minutes to allow for maximal anesthesia.
The process of placing a nasal block is often more painful than the reduction itself; several strategies and alternatives may help reduce this discomfort. Buffering the lidocaine with 7.5% sodium bicarbonate solution in a 1 : 5 dilution by volume (e.g., 2 mL sodium bicarbonate and 10 mL lidocaine) significantly reduces the burning sensation associated with the acidity of the anesthetic preparation.49 Infiltration should be done slowly, using a thin needle (27 gauge or less) within the dermal-subdermal or mucosal-submucosal plane to lessen pain from soft tissue dissection by the local anesthetic.50 Patients may have less discomfort with percutaneous injection of the infraorbital, infratrochlear, and external nasal nerves as compared with the intranasal approach.20 There is also evidence that the use of EMLA cream applied over the nose an hour before reduction, in combination with intranasal topical anesthetics, provides similar nasal anesthesia for reduction with significantly less discomfort than needle infiltration.51,52
Technique
Closed Reduction
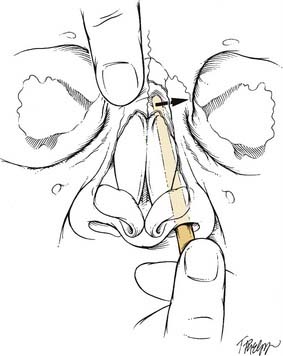
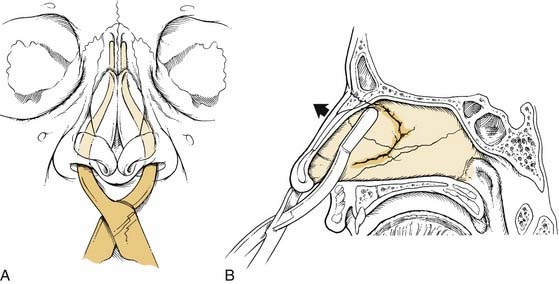
The use of a blunt elevator is recommended for most closed reductions, especially for cases in which there is significant medial collapse. Several different instruments, such as a Boies or Joker elevator (Fig. 35-9), can provide the surgeon with good tactile feedback and control of segment positioning. Before manipulation, the proper depth of insertion is determined by placing the instrument against the skin surface of the lateral nose, with the distal tip at the intercanthal line. The surgeon marks the position of the elevator at the alar rim and inserts it into the nasal cavity approximately 1 cm less than the measured depth. With only the tip of the instrument contacting the medial side of the nasal bone, the elevator is lifted anteriorly and laterally until the depressed segment is in proper position. The hand not holding the instrument can be used to pinch the nasal bones to mold the segments and prevent unnatural widening of the bridge. In the presence of a contralateral outfracture, the thumb places medial pressure on the opposite nasal bone so that both sides of the nasal pyramid are repositioned in a simultaneous, coordinated movement (Fig. 35-10).
Because of its role as the central support of the entire nasal complex, the septum is one of the most important structures to properly realign after a traumatic injury. Reduction of the septum before the nasal bone manipulation will release tension that is often responsible for relapse of an external nasal deformity.38 Closed reduction of the septum is often more challenging than nasal bone reduction due to the complexity of the forces exerted by surrounding structures and the frequent occurrence of preexisting deformities. The best results are usually obtained with the use of Asch forceps. Each arm of the instrument is inserted on either side of the septum and positioned superiorly just underneath the dorsum (Fig. 35-11). Using an upward and outward force perpendicular to the plane of the dorsum, the surgeon lifts the septum out of overlap and then uses the arms to push the ends back into realignment.
The correction of cartilaginous injuries with closed reduction techniques is difficult and often unsuccessful. For upper lateral cartilage avulsion with medial displacement, reduction may be possible if it is performed soon after injury and followed by 10 to 14 days of internal packing to maintain the union of the keystone area. If treatment is attempted beyond 2 weeks, an open approach through an intercartilaginous incision with the removal of fibrous adhesions between the nasal bone and superior upper lateral cartilage is necessary before reduction and stenting.24 For patients with poor results, delayed cartilage grafting may be offered to restore the external nasal contour after the injury has completely healed.53,54
Persistent deviation of the external nasal complex after an attempt at reduction is usually the result of inadequate understanding of the injury or poor timing. The most common reason for a failed reduction that is performed within the first week to 10 days is an unreduced septal fracture.10 For injuries that are more than 2 weeks old, fibrous tissue formation and early osseous remodeling are the causes of inadequate realignment. Osteotomy refracture to lyse these adhesions can be considered if reduction is desired acutely. If persistent deviation occurs after an appropriately timed reduction of a minor external deformity and a septal injury has been ruled out, an incomplete nasal bone fracture (greenstick) is likely. Conversion of the greenstick fracture to a complete fracture with an osteotome is necessary if internal stenting is unable to maintain the appropriate position. For the remaining cases of inadequate reduction, the surgeon should consider an unrecognized injury to the nasal cartilages or midfacial bones. Severe injuries that affect underlying support to the nasal pyramid will require open reduction and rigid fixation with or without bone grafting.
Care after Reduction
In an attempt to prevent collapse of the postreduction framework, intranasal packing may be placed under the mobile fracture segments to provide greater internal support.4,9,15 Additionally, intranasal synechiae formation may be reduced or prevented. Several different materials may be used for this task, including tampon sponges (e.g., Merocel), folded Telfa sheets, or ribbon gauze. The packs are coated in antibiotic ointment and placed superiorly within the nasal cavity to support the fracture without causing overdisplacement of the fragments. The material is removed after 3 to 5 days but can be left in as long as a week for cases of severe instability. Patients are placed on oral antibiotics during this period to prevent rhinitis and sinusitis. Other potential complications from pack placement include pain, epistaxis, and septal perforation55; these factors should be considered on an individual basis before nasal packing is used. Although Illum and coworkers7 found that internal packing was associated with a trend toward decreased nasal obstruction and better cosmetic appearance, there was not a statistically significant improvement for the entire group to justify its use in all patients. Some authors have advocated nasal packing only in cases of severe fracture instability,43 whereas others do not use it at all.21,52,56
The role of septal splints after nasal fractures has also been somewhat unclear. Splints have been advocated to provide additional support after septal reduction, prevention of hematoma, and intranasal adhesions,4,9,27 but there has been little evidence to support routine use in nasal fractures. The most likely benefit from their use is in cases with extensive mucosal injury and comminuted septal fractures that do not maintain alignment. Splints are custom-trimmed silicone sheets or manufactured products in various sizes and shapes with magnets or tubed nasal lumens (Doyle splints). The splint is coated with antibiotic ointment, inserted along each side of the septum, and secured with a loose anterior septal suture. Further reinforcement using packing material on the lateral surface of the splints should place even pressure on the septum. Splints are removed after 1 week but may be kept in place for longer periods in cases of greater instability. The potential complications from splints include increased pain,57 obstruction, septal perforation, and toxic shock syndrome.58,59
External nasal splinting is routinely performed at the conclusion of reduction.4,9,27,43 The skin is cleansed thoroughly with an alcohol or skin-preparation swab before the application of skin adhesive (e.g., Mastisol). After the surface is dry, a paper tape dressing (e.g., layered Steri-Strips) is applied to cover the nasal skin; the tape is generally thought to help prevent excessive swelling over the dorsum, resist hematoma formation, and protect the skin from potentially irritating splint adhesives.60 One of several different types of splinting material (e.g., plaster of Paris, Denver Splint, Thermoplast, Aquaplast) is custom molded to the surface of the nose, with care taken to not displace underlying bony fragments. The splint is left in place for seven to 10 days and kept dry to maintain adhesion. Illum’s7 prospective trial that evaluated the efficacy of fixation found that patients treated with an external plaster cast had significantly better appearance than those who received adhesive tapes alone. This was in contrast with the results published by Houghton and colleagues,56 who found no benefit to the use of external splinting. Despite conflicting evidence, the use of external nasal splinting is recommended, considering that it is usually well tolerated by the patient and provides a useful reminder to avoid potentially traumatizing activities.
Open Reduction
Repair of acquired nasal deformities by open reduction can represent two different types of surgical management. The first, which will be discussed in this chapter, is the immediate repair of displaced nasal fractures using wide surgical exposure, reduction, fixation, and reconstruction of severely damaged structures. The second is a delayed correction (usually 6 months or more) of persistent nasal deformities using the standard techniques of rhinoplasty (e.g., osteotomy, dorsal rasping, cartilage graft augmentation). Although the postponement of surgery in this situation is to allow for fracture healing and stabilization, the use of these procedures during the immediate postinjury phase has been recommended as an alternative to closed nasal reduction alone.44 Further discussion of this technique may be found in the chapters that cover rhinoplasty.
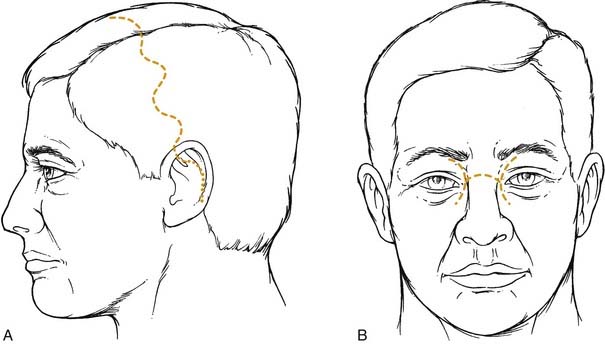
The most appropriate approach necessary to reconstruct a nasal deformity is dictated by the location of the injury and the type of reconstruction that is anticipated. For injuries of the upper third of the nose, an “open sky” incision through the nasofrontal crease provides direct access to comminuted nasal and ethmoid complex fractures, whereas a lateral rhinotomy can be used for unilateral nasal deformities; these incisions tend to leave a fairly visible scar. Preexisting lacerations in these areas can be extended within skin creases to allow for sufficient exposure. A bicoronal scalp flap is an excellent utility incision that can expose the superior nasal complex as well as other upper facial skeletal injuries (e.g., zygomatic arch and frontal sinus fractures) without creating conspicuous scarring (Fig. 35-12). This approach is also employed for cases in which calvarial bone may be necessary for defect reconstruction; the midfacial degloving incision can be used to expose the nasal bones as well. Lower nasal pyramid injuries can be accessed with a standard open rhinoplasty approach via bilateral marginal and transcolumellar incisions. Decortication is carried out superiorly to visualize the nasal cartilages and the caudal septum; this exposure may be inadequate if reduction and fixation of nasal bone fractures is required, and it also should not be used if there are dorsal and alar lacerations that may have disrupted the superiorly based blood supply that is vital to the columellar flap.11
After the fracture line has been adequately exposed and realigned, fixation is performed using one of several different methods to stabilize the reduction. Small-gauge wires (26 or greater) passed through predrilled holes can secure fracture segments to stable areas of the maxilla or frontal bone. Renner9 recommended that slow-absorbing sutures be used instead of wire to avoid palpable sharp edges underneath the skin surface. Titanium microplates are also less likely to be palpable through skin, and they provide the additional benefit of more versatile fragment positioning as compared with wiring techniques. The potential complications of using any metal fixation materials include bone erosion, skin breakdown, infection, migration, and localized pain. Rigid fixation techniques also preclude future rhinoplasty unless the hardware is first removed. Some of these problems may be avoidable with the use of bioabsorbable plates, but their efficacy in nasal reconstruction is yet to be established.
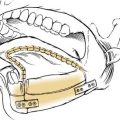
For more severe injuries that have poor underlying structural support or a significant loss of dorsal bone or cartilage, reconstruction using a cantilever graft is indicated. Although fracture segments should be conserved as much as possible, small fragments that do not contribute to the structure of the nasal complex should be removed to avoid their serving as a nidus for infection. The defect is then reconstructed with a graft that extends from the nasion to just beneath the cephalic border of the alar cartilages (Fig. 35-13). Autologous cranial bone, rib bone or cartilage, or homograft bone or cartilage are commonly used. Lag screw fixation to stable bone proximally is usually successful, but graft mobility has been reported in a portion of cases during long-term follow-up.61 Increased stability may be possible by anchoring the graft with a plate secured from the distal undersurface to the anterior nasal spine.38
Septal injuries that cannot be realigned with closed reduction should also be addressed with open techniques. Fracture lines are exposed with a hemitransfixion incision, or they can be more widely visualized with an open rhinoplasty approach. The edges of overlapping segments are placed under traction; then, if necessary, they are conservatively trimmed until end-to-end reduction is possible. In cases of anterior septal dislocation, a small strip of cartilage is removed inferiorly so that the quadrangular cartilage can be replaced within the maxillary crest. Fry62 suggested that scoring of the concave surface of a deformed cartilage surface may also help straighten the septum by releasing interlocked stress. If severe trauma has completely destroyed the integrity of the anterior septum, graft reconstruction is necessary to restore tip support and prevent columella retraction, saddle deformity, and internal nasal valve collapse. Posterior septal bone and split calvarium have been recommended as donor sources for reconstruction.63 Replacing the anterior septum with bone, however, may impart undesirable rigidity to the anterior aspect of the nose. The authors prefer replacing the damaged anterior septum with a cartilaginous graft such as auricular or costal cartilage.
Alternative Reduction Methods
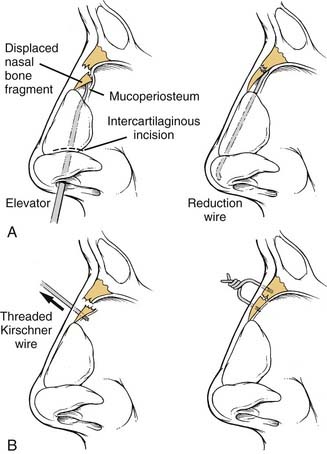
There have been attempts to find other minimally invasive methods of nasal realignment as alternatives to open reduction. Burm and Oh64 described an intranasal approach through an intercartilaginous incision to reduce a depressed nasal bone fracture. After mucoperiosteal tunnel dissection under the displaced segment, a wire is placed distally beneath the unfractured nasal root and over the distal lower lateral cartilage to keep the fragment elevated (Fig. 35-14A). The wire is trimmed, and a small piece is left exposed in the nasal cavity to allow for retrieval after 10 to 14 days. A success rate of 85% was reported in a group of 27 patients treated with this method, although there was no control group in the study.
Won Kim and coworkers65 proposed another technique for unfavorable fractures that involved the use of percutaneous wire fixation. With the use of fluoroscopic imaging, a threaded Kirschner wire is secured perpendicularly through the midpoint of the bony fragment. The segment is then aligned, and the wire is secured to a second wire that has been placed into stable bone to maintain reduction (see Fig. 35-14B). After 2 weeks, a repeat x-ray study is obtained, and the Kirschner wires are removed. Satisfactory results were noted in all cases, although only eight patients were treated in this study, and no control group was used for comparison.
Pediatric Nasal Fractures
Nasal fractures in children are quite different than those in adults and often prove to be more challenging to diagnose and manage. Anatomically, the child’s nose is more malleable because it has a greater cartilaginous composition and has less frontal projection. Traumatic forces are therefore easily spread to surrounding structures, which accounts for the higher incidence of concurrent facial fractures.66 The softer, more flexible nose is prone to greenstick fractures, which are difficult to palpate as compared with the more obvious stepoff deformities seen in adults. Palpation is also complicated by the presence of facial edema that quickly masks subtle deformities. Plain film studies are even less reliable in children given the incomplete ossification of nasal bones; therefore, the possibility of nasal fracture should be carefully considered in any case of pediatric facial or anterior cranial trauma. The most common alerting signs are asymmetry, epistaxis, edema, periorbital ecchymosis, skin lacerations, and nasal bone crepitus.67
One of the most important factors related to nasal trauma during early life is the risk of damage to the growth centers that are responsible for normal nasal and facial development. Normal growth of the child’s nose is mainly dependent on the septal cartilage. Animal studies have shown that removal of the septum during early life results in stunted nasal proportions, midfacial hypoplasia, relative mandibular prognathism, and malocclusion.68 The greatest amount of septal growth in children occurs in two different stages.69 The first stage is from birth to 5 years of age for both boys and girls; the second stage is from ages 10 to 14 years for boys and ages 8 to 12 for girls. Closed reduction of displaced fractures is generally considered safe in young children, but any elective open surgical correction should be postponed if at all possible until after these critical growth phases are complete.
If a displaced nasal fracture requires treatment, closed reduction should be carried out as soon as swelling no longer inhibits the assessment of underlying structures. Because of faster rates of bone healing, realignment in children should ideally be performed within four days of injury for best results.70 General anesthesia is almost always necessary for these cases. The correction of nasal and septal deformities is performed using an appropriately sized blunt instrument that will not excessively traumatize the nasal airway. Synechia formation and/or stenosis are more common in the smaller pediatric nasal cavity. The use of postreduction nasal splints and packing usually increases discomfort without significantly improving outcomes and therefore is not recommended; an exception may be considered for infants less than 6 months old who are obligate nasal breathers. Goode and Spooner67 suggested the use of intranasal silicone rubber tubing to stent the nasal passages in these children for a period of 4 to 5 days after manipulation until nasal edema subsides.
Although most deviated nasal fractures in children are successfully treated with conservative measures, there is an important role for open surgical reduction for the most severe trauma cases. Comminuted nasal and septal injuries that cannot be corrected with closed reduction are likely to produce long-term complications with poor nasal breathing and cosmetic malformation.71 Several authors have published evidence supporting the use of rhinoplasty in children with such injuries, citing that surgical correction can improve appearance and function without compromising nasal-facial development.71–76 This lack of growth disturbance may be due to the fact that the procedures did not damage the overlying mucoperichondrium, which has been shown to regenerate septal cartilage in young mammals after partial submucosal resection.77,78 Therefore, open surgical correction may be performed in cases of severe deformity, with the goal being realignment and reconstruction using as little dissection and tissue resection as possible. If total loss of the septum has occurred by trauma or infection, acute reconstruction with bone or cartilage grafts is necessary to reduce long-term complications.19 Schrader and Jahnke79 reported successful reconstruction using tragal cartilage and recommended it over posterior septal bone to avoid further risk of damage to important growth centers. For children who have septal destruction due to infection, immediate graft implantation has not been associated with a significant incidence of graft loss and is therefore recommended shortly after incision and drainage.63,79
Complications
Septal hematoma is one of the most severe early complications of nasal trauma. Blood collection under the perichondrium separates the vascular supply from the underlying cartilage, and this results in necrosis within 3 days.80 Immediate treatment is necessary to prevent long-term problems such as saddle deformity, perforation, columellar retraction, and nasal base widening. For children who are more likely to develop hematoma because of increased shear trauma to the softer nasal tissues, septal destruction can lead to devastating nasal and midfacial growth abnormalities.19 Incision and evacuation of the collection is performed, and several small openings are left to allow for dependent drainage. Splints or transseptal dissolving sutures are placed to obliterate the potential space and prevent re-collection. If the hematoma is not treated, bacterial seeding of the collection will result in abscess formation 6 to 7 days after trauma.81 Contiguous spread of the septal infection can then lead to further complications, such as osteomyelitis, orbital and intracranial abscesses, meningitis, and cavernous sinus thrombosis.82,83
CSF leakage is also a common complication of severe nasal, nasal-orbital-ethmoid complex, and frontal sinus fractures. CSF rhinorrhea is confirmed with β2-transferrin levels, and the location of the fistula is usually best identified with high-resolution computed tomography scanning.84 Most CSF leaks will spontaneously resolve with bedrest, head elevation, and possible lumbar CSF drainage. Persistent fistulas that do not resolve after 1 week of conservative treatment should be repaired surgically to prevent intracranial infection and pneumocephalus.
There are several delayed nasal complications that are often seen after a fracture. Worsening septal deviation, spurs, internal nasal valve collapse, and synechiae can all cause nasal airflow obstruction with growth. Blockage of mucociliary clearance can lead to a higher incidence of acute and chronic sinus infections. Illum and colleagues7 found that a significant increase in saddle deformity and dorsal humps occurred in patients who were reexamined 3 years after their injuries; some of these problems may be worse in children who have more profound deformations after injury during the critical developmental phases of the nose. Regeneration of destroyed or missing cartilage may also result in overgrowth of the septum, thereby leading to a late onset of internal and external deformity.74 Patients with significant nasal injuries should be followed up for at least a year or more to evaluate for these complications.
Anderson PJ. Fractures of the nasal skeleton in children. Injury. 1995;26:47.
Cox AJ. Nasal fractures—the details. Facial Plast Surg. 2000;16:87.
Daw JL, Lewis VL. Lateral force compared with frontal impact nasal fractures: need for reoperation. J Craniomaxillofac Trauma. 1995;1:50.
Frodel JL. Management of the nasal dorsum in central facial injuries: indications for calvarial bone grafting. Arch Otolaryngol Head Neck Surg. 1995;121:307.
Logan M, Odriscoll K, Masterson J. The utility of nasal bone radiographs in nasal trauma. Clin Radiol. 1994;49:192.
Murray JA, Maran AG, Busuttil A, et al. A pathological classification of nasal fractures. Injury. 1986;17:338.
Murray JA, Maran AG, Mackenzie IJ, et al. Open versus closed reduction of the fractured nose. Arch Otolaryngol. 1984;110:797.
Murray JAM, Maran AGD. The treatment of nasal injuries by manipulation. J Laryngol Otol. 1980;94:1405.
Pollock RA. Nasal trauma: pathomechanics and surgical management of acute injuries. Clin Plast Surg. 1992;19:133.
Rohrich RJ, Adams WP. Nasal fracture management: minimizing secondary nasal deformities. Plast Reconstr Surg. 2000;106:266.
Stranc MF, Robertson GA. A classification of injuries of the nasal skeleton. Ann Plast Surg. 1979;2:468.
Verwoerd CD. Present day treatment of nasal fractures: closed versus open reduction. Facial Plast Surg. 1992;8:220.
Werther JR. External rhinoplasty approach for repair of posttraumatic nasal deformity. J Craniomaxillofac Trauma. 1996;2:12.
Won Kim S, Pio Hong J, Kee Min W, et al. Accurate, firm stabilization using external pins: a proposal for closed reduction of unfavorable nasal bone fractures and their simple classification. Plast Reconstr Surg. 2002;110:1240.
1. Alvi A, Doherty T, Lewen G. Facial fractures and concomitant injuries in trauma patients. Laryngoscope. 2003;113:102.
2. Crowther JA, O’Donoghue GM. The broken nose: does familiarity breed neglect? Ann R Coll Surg Engl. 1987;62:259.
3. Daw JL, Lewis VL. Lateral force compared with frontal impact nasal fractures: need for reoperation. J Craniomaxillofac Trauma. 1995;1:50.
4. Haug RH, Prather JL. The closed reduction of nasal fractures: an evaluation of two techniques. J Oral Maxillofac Surg. 1991;49:1288.
5. Holt GR. Biomechanics of nasal septal trauma. Otolaryngol Clin North Am. 1999;32:615.
6. Illum P. Long-term results after treatment of nasal fractures. J Laryngol Otol. 1986;100:273.
7. Illum P, Kristensen S, Jorgensen K, et al. Role of fixation in the treatment of nasal fractures. Clin Otolaryngol. 1983;8:191.
8. Murray JAM, Maran AGD. The treatment of nasal injuries by manipulation. J Laryngol Otol. 1980;94:1405.
9. Renner GJ. Management of nasal fractures. Otolaryngol Clin North Am. 1991;24:195.
10. Rohrich RJ, Adams WP. Nasal fracture management: minimizing secondary nasal deformities. Plast Reconstr Surg. 2000;106:266.
11. Werther JR. External rhinoplasty approach for repair of posttraumatic nasal deformity. J Craniomaxillofac Trauma. 1996;2:12.
12. Anderson PJ. Fractures of the nasal skeleton in children. Injury. 1995;26:47.
13. Dickson MG, Sharpe DT. A prospective study of nasal fractures. J Laryngol Otol. 1986;100:543.
14. East CA, O’Donoghue G. Acute nasal trauma in children. J Pediatr Surg. 1987;22:308.
15. Green KM. Reduction of nasal fractures under local anaesthetic. Rhinology. 2001;39:43.
16. Logan M, Odriscoll K, Masterson J. The utility of nasal bone radiographs in nasal trauma. Clin Radiol. 1994;49:192.
17. Muraoka M, Nakai Y. Twenty years of statistics and observation of facial bone fracture. Acta Otolaryngol Suppl. 1998;538:261.
18. Murray JA, Maran AG, Mackenzie IJ, et al. Open versus closed reduction of the fractured nose. Arch Otolaryngol. 1984;110:797.
19. Olsen KD, Carpenter RJ, Kern EB. Nasal septal injury in children. Arch Otolaryngol. 1980;106:317.
20. Cook JA, Murrant NJ, Evans K, et al. Manipulation of the fractured nose under local anaesthesia. Clin Otolaryngol. 1992;17:337.
21. Cook JA, Murrant NJ, Evans K, et al. A randomized comparison of manipulation of the fractured nose under general anaesthesia. Clin Otolaryngol. 1990;15:343.
22. Lanza DC, Kennedy DW, Koltai PJ. Applied nasal anatomy and embryology. Ear Nose Throat J. 1991;70:416.
23. McKinney P, Johnson P, Walloch J. Anatomy of the nasal hump. Plast Reconstr Surg. 1986;77:404.
24. Parkes ML, Kanodia R. Avulsion of the upper lateral cartilage: etiology, diagnosis, surgical anatomy and management. Laryngoscope. 1981;91:758.
25. Oneal RM, Beil RJ, Schlesinger J. Surgical anatomy of the nose. Clin Plast Surg. 1996;23:195.
26. Pitanguy I. Revisiting the dermocartilaginous ligament. Plast Reconstr Surg. 2001;107:264.
27. Colton JJ, Beekhuis GJ. Management of nasal fractures. Otolaryngol Clin North Am. 1986;19:73.
28. Harrison DH. Nasal injuries: their pathogenesis and treatment. Br J Plast Surg. 1979;32:57.
29. Verwoerd CD. Present day treatment of nasal fractures: closed versus open reduction. Facial Plast Surg. 1992;8:220.
30. Krause C. Nasal fractures: evaluation and repair. In: Mathog RH, editor. Maxillofacial Trauma. Baltimore: Williams & Wilkins; 1984:257-265.
30A. Fry HJH. Interlocked stresses in human nasal septal cartilage. Br J Plast Surg. 1966;19:276.
31. Osguthorpe JD, Hoang G. Nasolacrimal injuries: evaluation and management. Otolaryngol Clin North Am. 1991;24:59.
32. Leipziger LS, Manson PN. Nasoethmoid orbital fractures. Current concepts and management principles. Clin Plast Surg. 1992;19:167.
33. Stranc MF, Robertson GA. A classification of injuries of the nasal skeleton. Ann Plast Surg. 1979;2:468.
34. Greene D, Maas CS, Carvalho G, et al. Epidemiology of facial injury in female blunt assault trauma cases. Arch Facial Plast Surg. 1999;1:288.
35. Zachariades N, Koumoura F, Konsolaki-Agouridaki E. Facial trauma in women resulting from violence from men. J Oral Maxillofac Surg. 1990;48:1250.
36. Kern RC, Quinn B, Rosseau G, et al. Post-traumatic olfactory dysfunction. Laryngoscope. 2000;110:2106.
37. Guyuron B, Zarandy S. Does rhinoplasty make the nose more susceptible to fracture? Plast Reconstr Surg. 1994;93:313.
38. Pollock RA. Nasal trauma: pathomechanics and surgical management of acute injuries. Clin Plast Surg. 1992;19:133.
39. de Lacey GJ, Wignall BK, Hussain S, et al. The radiology of nasal injuries: problems of interpretation and clinical relevance. Br J Radiol. 1977;50:412.
40. Illum P. Legal aspects in nasal fractures. Rhinology. 1991;29:263.
41. Remmler D, Denny A, Gosain A, et al. Role of three-dimensional computed tomography in the assessment of nasoorbitoethmoidal fractures. Ann Plast Surg. 2000;44:553.
42. Klotz DA, Winkle MR, Richmon J, et al. Surgical management of posterior epistaxis: a changing paradigm. Laryngoscope. 2002;112:1577.
43. Ridder GJ, Boedeker CC, Fradis M, et al. Technique and timing for closed reduction of isolated nasal fractures: a retrospective study. Ear Nose Throat J. 2002;81:49.
44. Staffel JD. Optimizing treatment of nasal fractures. Laryngoscope. 2002;112:1709.
45. Clark WD, Stiernberg CM. Early aggressive treatment of nasal fractures. Ear Nose Throat J. 1986;65:481.
46. Hill CD. Joint Commission focuses on pain management. From the Joint Commission on Accreditation of Healthcare Organizations Web site. August 3, 1999. Available at http://www.jcaho.org/news+room/health+care+issues/jcaho+focuses+on+pain+management.htm
47. Waldron J, Mitchell DB, Ford G. Reduction of fractured nasal bones; local versus general anesthesia. Clin Otolaryngol. 1989;14:357.
48. Watson DJ, Parker AJ, Slack RW, et al. Local versus general anaesthetic in the management of the fractured nose. Clin Otolaryngol. 1988;13:491.
49. Metzinger SE, Bailey DJ, Boyce RG, et al. Local anesthesia in rhinoplasty: a new twist? Ear Nose Throat J. 1992;71:405.
50. Arndt KA, Burton C, Noe J. Minimizing the pain of local anesthesia. Plast Reconstr Surg. 1983;72:676.
51. el-Kholy A. Manipulation of the fractured nose using topical anaesthesia. J Laryngol Otol. 1989;103:580.
52. Jones TM, Nandapalan V. Manipulation of the fractured nose: a comparison of local infiltration anaesthesia and topical local anaesthesia. Clin Otolaryngol. 1999;24:443.
53. Gilbert SE. Overlay grafting for lateral nasal wall concavities. Otolaryngol Head Neck Surg. 1998;119:385.
54. Tardy E. Rhinoplasty: The Art and the Science. Philadelphia: WB Saunders; 1997.
55. von Schoenberg M, Robinson P, Ryan R. Nasal packing after routine nasal surgery—is it justified? J Laryngol Otol. 1993;107:902.
56. Houghton DJ, Hanafi Z, Papakostas K, et al. Efficacy of external fixation following nasal manipulation under local anaesthesia. Clin Otolaryngol. 1998;23:169.
57. Malki D, Quine SM, Pfleiderer AG. Nasal splints, revisited. J Laryngol Otol. 1999;113:725.
58. Moser N, Hood C, Ervin D. Toxic shock syndrome in a patient using bilateral silicone nasal splints. Otolaryngol Head Neck Surg. 1995;113:632.
59. Wagner R, Toback J. Toxic shock syndrome following septoplasty using plastic septal splints. Laryngoscope. 1986;96:609.
60. Cox AJ. Nasal fractures—the details. Facial Plast Surg. 2000;16:87.
61. Frodel JL. Management of the nasal dorsum in central facial injuries: indications for calvarial bone grafting. Arch Otolaryngol Head Neck Surg. 1995;121:307.
62. Fry HJH. Nasal skeletal trauma and the interlocked stresses on the nasal septal cartilage. Br J Plast Surg. 1967;20:146.
63. Hellmich S. Reconstruction of the destroyed septal infrastructure. Otolaryngol Head Neck Surg. 1989;100:92.
64. Burm JS, Oh SJ. Indirect open reduction through intercartilaginous incision and intranasal Kirschner wire splinting of comminuted nasal fractures. Plast Reconstr Surg. 1998;102:342.
65. Won Kim S, Pio Hong J, Kee Min W, et al. Accurate, firm stabilization using external pins: a proposal for closed reduction of unfavorable nasal bone fractures and their simple classification. Plast Reconstr Surg. 2002;110:1240.
66. Stucker FJ, Bryarly RC, Schockley WW. Management of nasal trauma in children. Arch Otolaryngol. 1984;110:190.
67. Goode RL, Spooner TR. Management of nasal fracture in children: a review of current practices. Clin Pediatr. 1972;11:526.
68. Sarnat BG, Wexler MR. Longitudinal development of upper facial deformity after septal resection in growing rabbits. Br J Plast Surg. 1969;22:313.
69. van Loosen J, Baatenburg de Jong RJ, van Zanten GA, et al. A cephalometric analysis of nasal septal growth. Clin Otolaryngol. 1997;22:452.
70. Martinez SA. Nasal fractures: what to do for a successful outcome. Postgrad Med. 1987;82:71.
71. Jugo SB. Total septal reconstruction through decortication approach in children. Arch Otolaryngol Head Neck Surg. 1987;113:173.
72. Crysdale WS, Walker PJ. External septorhinoplasty in children: patient selection and surgical technique. Laryngoscope. 1994;23:28.
73. Ortiz-Monasterio F, Olmedo A. Corrective rhinoplasty before puberty: a long-term follow-up. Plast Reconstr Surg. 1981;68:381.
74. Pirsig W, Lehmann I. The influence of trauma on the growing septal cartilage. Rhinology. 1975;13:39.
75. Triglia JM, Cannoni M, Pech A. Septorhinoplasty in children: benefits of the external approach. J Otolaryngol. 1990;19:274.
76. Walker PJ, Crysdale WS, Farkas LG. External septorhinoplasty in children: outcome and effect on growth of septal excision and reimplantation. Arch Otolaryngol Head Neck Surg. 1993;119:984.
77. Berstein L. Early submucous resection of nasal septal cartilage. A pilot study in canine pups. Arch Otolaryngol. 1973;97:273.
78. Jeffries DJR, Rhys Evans PH. Cartilage regeneration following septal surgery in young rabbits. J Laryngol Otol. 1984;98:577.
79. Schrader M, Jahnke K. Tragal cartilage in the primary reconstruction of defects resulting from a nasal septal abscess. Clin Otolaryngol. 1995;20:527.
80. Fry HJH. The pathology and treatment of haematoma of the nasal septum. Br J Plastic Surg. 1969;22:331.
81. Canty PA, Berkowitz RG. Hematoma and abscess of the nasal septum in children. Arch Otolaryngol Head Neck Surg. 1996;112:1373.
82. Matsuba HM, Thawley SE. Nasal septal abscess: unusual causes, complications, treatment and sequelae. Ann Plast Surg. 1986;16:161.
83. Thomson CJR, Berkowitz RG. Extradural frontal abscess complicating nasal septal abscess in a child. Int J Pediatr Otorhinolaryngol. 1998;45:183.
84. Zapalac JS, Marple BF, Schwade ND. Skull base cerebrospinal fluid fistulas: a comprehensive diagnostic algorithm. Otolaryngol Head Neck Surg. 2002;126:669.