Nail Disorders
Robert A. Silverman, Adam I. Rubin
Introduction
Nails are specialized cutaneous appendages composed of hard keratins similar to those found in hair, and are unique to primates. In humans, nails function as a stabilizing unit to aid in tactile sensation, grasping, and scratching. Well-manicured or adorned nails in adolescents and adults may be perceived as an attribute of social acceptability and serve as a source of personal satisfaction. Although abnormalities of the nails are rare, they may affect an individual’s self-esteem and their relationships with others. Abnormal nails in a neonate or infant may be indicative of a more widespread inherited or sporadic syndrome, or they may be a localized congenital malformation. In either case, parents may be concerned about their child’s nails, sometimes out of proportion to the magnitude of any other problems that may be present. Investigation and consultations to uncover any associated illness and to allay any untoward parental anxiety are warranted.
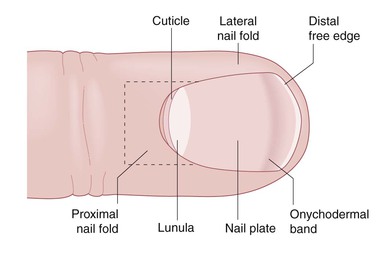
The nail unit is composed of a rectangular nail plate bordered by proximal and lateral nail folds (Fig. 32.1).1 The cuticle attaches the proximal nail fold to the nail plate. This acellular membrane is tightly adherent and prevents invasive microorganisms reaching the underlying matrix. The lunula (half moon) represents the distal portion of the nail’s proliferative matrix. The ventral side of the nail plate has longitudinal ridges that orient the direction of growth from the root over a complementary grooved nail bed. At birth, the dorsal surface of the nail displays unique, somewhat oblique ridges as well. These ridges become parallel and disappear slowly, and over time, the surface becomes smooth. The distal free edge of the plate separates from the bed at the hyponychium. The shape of the nail plate is convex. It is normally thickest at its proximal portion and thins distally. The size of the nail plate is determined by the size and growth of the underlying distal phalanx. Because embryologic development occurs in a cephalocaudal direction, it is not surprising that at birth, especially in premature infants, toenails may be smaller than fingernails. In premature infants, less than 32 weeks’ gestation, nail plates may not extend beyond the distal groove of the hyponychium. In postmature infants, such as macrosomic infants or infants of diabetic mothers, the nail plate may extend well beyond the hyponychium. In adults, it is estimated that fingernails grow 0.1 mm/day and toenails grow 1 mm/month. Similar data in newborns and infants are not available. Box 32.1 lists pathologic factors that affect nail growth.
The anatomic structure of the nail unit is affected by many disease states.1 Conditions may be primary or secondary, localized or generalized, congenital or acquired. They can be associated with genetic syndromes, or drug exposures, or with infectious or systemic disease. Nail morphogenesis begins during the 9th week of gestation and is completed by the end of the second trimester (see Chapter 1).
Beau’s lines
Beau’s lines are transverse grooves or moat-like depressions that extend across the nail plate from one lateral nail fold to the other.2,3 This deformity is a manifestation of nail matrix arrest and is first observed adjacent to the proximal nail fold. Beau’s lines slowly move toward the distal free edge of the nail plate as nail growth resumes. If the rate of nail growth is known, one can estimate the date of nail matrix arrest by measuring the distance between the proximal nail fold and the Beau’s line. Causes of Beau’s lines include high fevers caused by infection, severe cutaneous inflammatory diseases such as Stevens–Johnson syndrome or Kawasaki disease, a reaction to medications, and acrodermatitis enteropathica. Beau’s lines may occur in infants, 4–10 weeks of age, as a result of the stress of delivery. They have also been reported at birth as a result of intrauterine stress in a premature infant (Fig. 32.2).4 Although Beau’s lines should develop on all fingernails and toenails, they are usually most prominent on the thumb and great toe nails because of their slower rate of growth.
Onychomadesis refers to proximal separation of the nail plate from the nail bed. Latent onychomadesis occurs when the nail separates some time after a profound interruption in nail growth. Causes are similar to those that produce Beau’s lines and may occur during the neonatal period as well.
Alterations in nail shape
There is a close interaction between the formation of epidermal appendages and mesoderm during embryologic development. Therefore, it is not surprising that there are many alterations of nail shape that are linked with distant or underlying malformations of bone. It is not uncommon for newborns to have variations of the normal convex curvature of the nail. Koilonychia refers to nails that exhibit a concave or spoon shape.5 This may be a normal variant in newborns, especially when it involves the great toe nails. As the child grows and the distal phalanges lengthen, koilonychia gradually improves. Recently, a case of koilonychia, dome-shaped femoral epiphyses, and platyspondylia has been described.6 It is widely accepted that koilonychia in infants and toddlers may be indicative of iron deficiency.7 However, no well-controlled studies of iron deficiency in large numbers of infants with and without koilonychia have been reported, and improvement of nail shape with the administration of iron has not been documented. Familial koilonychia has also been reported.8 It has been described with other ectodermal defects such as monilethrix, palmoplantar keratoderma, and steatocystoma multiplex, as well as Turner syndrome.9
Other deformities in nail shape include pincer nails, claw nails, and racquet nails. Pincer nails are characterized by a transverse overcurvature of the nail plates.10 The condition is usually acquired, but some cases may result from an inherited developmental anomaly. If the convex transverse overcurvature is prominent, nails may appear similar to those in patients with pachyonychia congenita and occasionally may be quite painful. Congenital claw-like nails have also been reported.11 The nail plates have a dorsal convexity and then curve downward to resemble onychogryphosis. This is usually noted on the second to fourth toes and may be associated with a cleft hand. Hypoplasia of the distal phalanx with absence of the ossification center is observed on radiographs of the affected digits.12 Correction of the deformity is desirable because of the tendency toward recurrent bleeding and ulceration of the tip of the toe. Some authors distinguish claw nails from another isolated ungual anomaly, congenital curved nail of the fourth toe.13 Nails in these cases are normal thickness and have a longitudinal overcurvature. This trait may be sporadic or inherited, and is also associated with underlying distal phalangeal deformities.14 It may not come to medical attention until traumatic dystrophy occurs later in childhood. Racquet nails occur when the width of the nail plate exceeds its length, also referred to as brachyonychia. It may be a sign of foreshortening of the terminal phalanx and may be associated with other congenital anomalies.15
Clubbing is a curved or beak-like deformity of the nail unit that accompanies hypertrophy and hyperplasia of the fibrovascular support stroma of the distal phalanx. It is an acquired sign of both systemic and hereditary diseases.1 In neonates or infants, clubbing may be an early manifestation of cyanotic congenital heart disease, bronchopulmonary diseases, or HIV disease.16,17
Alterations in nail size
Anonychia refers to the absence of nails. The most widely known association is with nail–patella syndrome (see below). Isolated congenital anonychia has been reported in families with both autosomal recessive18,19 and autosomal dominant inheritance. Rudimentary nail units may be evident, but the underlying phalangeal structure is normal. Anonychia and hypoplasia of the nails may be observed with absence of the distal phalanges and foreshortening of the affected digits (Fig. 32.3). Anonychia has been reported with limb defects,20 ectrodactyly,21 flexural pigmentation,22 isolated to the thumbnails,23 and with sensorineural hearing loss.24 These latter cases have been termed DOOR syndrome (deafness, onycho-osteodystrophy, and retardation). Elevated urinary amino acids have been detected in some patients with DOOR syndrome.22 Anonychia of the fifth fingers and toenails is characteristic of Coffin–Siris syndrome.25 Other features include growth and mental retardation, generalized hypertrichosis and scalp hypotrichosis, lax joints, and abnormal facies. Anonychia, nail hypoplasia, and other nail anomalies, such as double nails (Fig. 32.4), may occur as isolated findings.26

Infants with junctional and dystrophic forms of epidermolysis bullosa (EB) frequently have anonychia at birth (Fig. 32.5).27 Subungual hemorrhages, onycholysis (separation of the nail plate from the nail bed) and onychomadesis precede nail loss. One or more fingernails are usually affected. The periungual tissues and nail beds are frequently swollen and inflamed. Granulation tissue develops quickly. Meticulous hygiene, application of topical antibiotics, and wound care with synthetic dressings may optimize regrowth if possible. It is the authors’ opinion that in utero sucking of the fingers results in most of the nail disease that is present at birth in EB.
Micronychia
Small nails may be localized to one or a few digits or involve all of the nail fields (Fig. 32.6). Conditions associated with micronychia are listed in Table 32.1.28–32 Current theory suggests that at least some forms of micronychia, such as in fetal alcohol syndrome and exposure to anticonvulsants, are due to inhibition of retinoic acid synthesis during early embryologic development.33,34 Selected specific causes of micronychia are discussed in subsequent sections.

TABLE 32.1
Causes of micronychia
| Disorder | Clinical manifestations |
| Nail-patella syndrome | Small or absent patellas, iliac horns, triangular lunulae |
| Congenital onychodysplasia | |
| Ectodermal dysplasias | Variable sweating, hair and tooth abnormalities |
| Congenital malalignment of index fingers | None, except underlying phalangeal malformation |
| Fetal teratogens | |
| Alcohol | Microcephaly, short palpebral fissures, maxillary hypoplasia |
| Hydantoins (and other anticonvulsants) | Short stature, retardation, hypertelorism, depressed nasal bridge, cardiac anomalies, mucosal changes |
| Polychlorinated biphenyls | Natal teeth, pigment anomalies, mucosal changes |
| Warfarin | Nasal hypoplasia, stippled epiphyses |
| Chromosome and genetic abnormalities | |
| Coffin–Siris syndrome | Hypoplasia of the fifth digit, lax joints, blepharoptosis, and multiple genetic mutations |
| Dyskeratosis congenita | Hyperpigmentation and hypopigmentation, Fanconi-like anemia, blepharitis, leukoplakia, XLRa and DKC1 mutation |
| Adams–Oliver syndrome | Large defects of aplasia cutis of the scalp with cutis marmorata, congenital heart malformations and transverse limb reduction defects, DOCK6 and RBPJ mutations |
| Simpson-Golabi-Behmel syndrome | Macrosomia, abnormal facies, supernumerary nipples, polydactyly, heart defects, X-linked GPC3 mutation |
| Trisomies | 3q, 8, 13, 18 |
| Turner syndrome | XO, webbed neck, nevi, lymphedema, coarctation of the aorta |
| Noonan syndrome | XY male with a Turner phenotype and pulmonic stenosis |
| Amniotic bands | Hypoplasia of the distal phalanx associated with aplasia cutis |
a X-linked recessive inheritance.
Nail–patella syndrome
Nail–patella syndrome, also known as hereditary osteo-onychodysplasia (HOOD), is an autosomal dominant genodermatosis characterized by nail hypoplasia present at birth, chronic progressive nephropathy, and hypoplastic patellae that may result in debilitating osteoarthritis. This disorder has a high degree of penetrance and widely variable expressivity.35 Nail disease is usually the only manifestation in neonates. However, there are rare reports of infants with proteinuria, signifying the early onset of renal pathology.36
Ungual manifestations are most prominent on the ulnar sides of the thumbs and index fingers, and to a lesser degree on other digits. They include micronychia, hemionychia, and occasionally anonychia. If present, a triangularly shaped lunula with a distal apex is nearly pathognomonic for the condition.37 Nail plates may be thin and display koilonychia, which can lead to frequent chipping and splitting later in childhood.
Skeletal deformities are not visible until ossification centers develop. Parents may be screened for small, easily subluxed patellae, characteristic posterior iliac horns, hypoplasia of the proximal radius and ulna, scoliosis, and thickened scapulae. Generally, patients with nail–patella syndrome are not identified until early adulthood, when knee dislocation, pain, and gait disturbances bring them to medical attention.38
Renal disease that presents as asymptomatic proteinuria is the most serious manifestation of nail–patella syndrome. It is usually not apparent until adulthood, but a newborn and a 2-year-old child with nephrosis have been reported.39 Renal biopsies have uncovered glomerulonephritis secondary to glomerular basement membrane zone thickening from collagen fibril deposition. These findings have even been noted in a spontaneously aborted 18-week-old fetus.40
Other manifestations include heterochromic irides, colobomas, microcorneas, glaucoma,41 popliteal pterygia, and mild mental deficiency. It has been suggested that these, as well as other findings such as colon cancer, in specific kindreds may be a result of contiguous gene defects, translocations, or other genetic aberrations.42 Complications from cerebral and large vessel dilation have also been reported, and are also caused by collagenous basal lamina reduplication.43
Mutations in the LIM homeodomain protein gene LMX1b have been demonstrated in the region of 9q34 and result in the nail–patella syndrome.44 This gene is responsible for dorsoventral body pattern formation during fetal development. It is linked to the ABO blood group and had been believed to be an abnormality in COL5A1, which is necessary for the production of collagen type V, an important component in the glomerular and other basement membrane zones.45
Congenital onychodysplasia of the index fingers
Congenital onychodysplasia of the index fingers (COIF), also now known as Iso–Kikuchi syndrome, was first described in 1969.46,47 Original cases were congenital, limited mainly to the index fingers, and characterized by anonychia, micronychia, and/or polyonychia (Fig. 32.7). They were nonfamilial and nonhereditary, and without underlying bone or joint abnormalities. Since that time, the clinical criteria have been changed or expanded to encompass a number of additional observations.48
Although the index fingers are most commonly affected, onychodystrophy has been reported on other fingers and toes.49,50 Malalignment, ‘rolled micronychia,’ hemionychogryphosis, onychoheterotopia, and polyonychia with syndactyly have also been detailed. Unlike nail–patella syndrome, abnormalities in the nail unit are more prominent on the radial aspects of the digits. A Y-shaped bifurcation of the distal phalanx on lateral radiographs is frequent and is characteristic of the condition.51 Familial cases have also been documented.52
The pathogenesis of congenital onychodysplasia is poorly understood. An abnormal vascular supply, anomalies from an abnormal grip, external deformation from pressure against the cranium, exposure to teratogens, and genetic influences have been implicated by a number of authors.50 It is quite possible that the clinical findings may be explained by any of these theories if the inciting event occurs at a specific time during the embryologic development of the nail unit.
Onychoatrophy
Onychoatrophy refers to a progressive reduction in size and thickness of the nail unit. The term is usually used to describe acquired dissolution of ungual structures and should not be used synonymously with micronychia, although some authors do so. Inflammatory disorders, which are observed in older children and adults, but rarely documented in newborns and infants, such as Stevens–Johnson syndrome or graft-versus-host disease, may result in onychoatrophy. Infants with congenital disorders that have a progressive phenotype, such as acrogeria or dyskeratosis congenita, can have onychoatrophy as well. Occlusion of the digital artery by emboli may result in phalangeal necrosis and destruction of nail structures. Other postnatal vascular insults, such as extensive aplasia cutis congenita or disseminated intravascular coagulation from homozygous protein C deficiency, could potentially have similar effects.
Ectopic nails
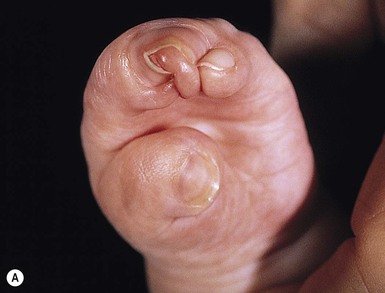
Onychoheterotopia, or ectopic nails, occurs when ungual tissue develops on areas other than the dorsal aspect of the distal phalanx.50 Cases that have been reported tend to involve the palmar surface of the fifth fingers.53–56 They have been both sporadic and reported in siblings, suggesting possible autosomal recessive inheritance. Other abnormalities of the hand may also be present, including underlying osseous malformations. A circumferential nail of the fifth finger has been documented in association with a deletion in the long arm of chromosome 6.57 This tubular defect may occur on other digits as well.58 The presence of a circumferential nail is frequently observed at the tip of the fused digits of the hand in acrocephalosyndactyly or Apert syndrome.59 Synonychia and fusion of all of the toes are also observed in this sporadic condition, which is caused by mutations in the gene encoding fibroblast growth factor receptor-2 (FGFR-2) found on the chromosomal locus 10q26 (Fig. 32.8).60
Hypertrophy of the nail
Large nails with anatomically normal nail units may be observed in newborns with macrodactyly. Conditions that display macronychia include epidermal nevus syndrome, Proteus syndrome, Maffucci syndrome, Klippel–Trenaunay–Weber syndrome, and gigantism. Patients with the ectrodactyly–ectodermal dysplasia–cleft lip/palate (EEC) syndrome also may have a large nail on the fused digits. Several terms are used to describe different types of enlarged nails. Onychauxis refers to nails that exhibit thick nail plates but retain a normal overall size and shape. Onychogryphosis is present when the nail plate thickens and develops an inferior overcurvature. If nail growth is uneven, the plate deviates obliquely and takes on the appearance of a ram’s horn. The nail plates are usually discolored and display oyster-like striations across the surface. Although onychogryphosis is usually observed on toenails in the elderly or on digits that have been permanently injured, hereditary autosomal dominant and congenital forms involving both the fingernails and toenails have been reported.53,54 Hemionychogryphosis has been seen in cases of congenital malalignment of the great toe nails and COIF. Pachyonychia refers to thickening and superior deviation of the nail plate owing to the accumulation of subungual hyperkeratosis. This may be observed in older patients with psoriasis or onychomycosis, but the term is classically used to describe the inherited condition pachyonychia congenita.
Pachyonychia congenita
Pachyonychia congenita61 is characterized by hard, thick nails that angle upwards at their distal free edge because of accumulation of keratin in the ventral nail plate. The lateral borders curve under and give the plates a pincer-like appearance (Fig. 32.9). Unlike onychogryphosis, the nails of pachyonychia congenita have a smooth surface. Although pachyonychia congenita syndrome is transmitted as an autosomal dominant trait with a high degree of penetrance, full expressivity may not become evident until later childhood or adulthood. Infants with pachyonychia congenita initially display a yellowish-brown discoloration of the nails. Thickening from subungual hyperkeratosis occurs gradually over months to years.
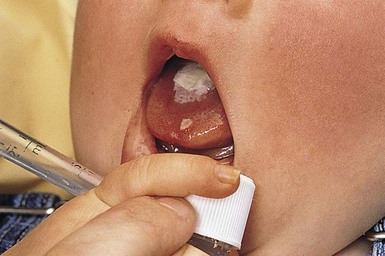
Until recently, patients with pachyonychia congenita were classified into one of two syndromes that had one of several genetic defects in hard keratin.55 Mutations in keratin 16 (located on chromosome 17) or in keratin 6A (located on chromosome 12) have been found in type I, the Jadassohn–Lewandowski variant. As newborns, these patients may have foamy white mucosal plaques of oral leukokeratosis (Fig. 32.10). During childhood, debilitating palmoplantar keratoderma, hyperhidrosis, and secondary bullae develop. Clusters of rough, dry, spiny papules become evident over the body, particularly on the elbows and knees, similar to psoriasis. Later, there may be eruption of epidermoid cysts. Type II patients with the Jackson–Lawler form of the disease have abnormalities in the keratin 17 gene (found on chromosome 17) or keratin 6B (found on chromosome 12). Natal teeth with milia, minimal oral leukokeratosis, cylindromas, steatocystomas, and milder keratoderma are present in these cases. However, considerable overlap may exist with some signs.
A recent publication from the International Pachyonychia Congenita Consortium (IPCC) recommends the elimination of the terms ‘PC-1’ and ‘PC-2’ and proposed their replacement with notation of the specific keratin defect. In this classification scheme a diagnosis of PC-6a, PC-6b, PC-16, and PC-17 would correspond to mutations in the KRT6A, KRT6B, KRT16, and KRT17 genes, respectively. A designation of PC-U (unknown) may be applied when the classic clinical findings of PC are found in the absence of a known PC keratin gene mutation. This new classification recognizes the overlap in signs and symptoms of the different genotypes of PC and will aid in future gene therapy for these patients.61 A registry and support group for patients and their families with pachyonychia congenita is now available (www.pachyonychia.org).
Ingrown toenails
There are three types of ingrown toenail in neonates. Congenital malalignment of the great toe presents with a trapezoid-shaped nail plate that deviates laterally with respect to the longitudinal axis of the distal phalanx (Fig. 32.11).56 Cases may be unilateral, bilateral, sporadic, or inherited as an autosomal dominant trait.57 While classically affecting the great toes, malalignment of the fourth toenail and index fingers has also been reported.62,63 Recurrent damage to the nail matrix occurs when the child is old enough to crawl and walk. This damage is manifested by multiple transverse ridges, discoloration caused by infection and hemorrhage, paronychia, onycholysis, and nail loss.58 Mild degrees of malalignment may improve over time.59 However, when marked deviation of the nail plate results in the distal free edge embedding into the soft tissues of the hyponychium, surgical rotation of the misdirected matrix may be necessary to prevent chronic long-term disability.60
Congenital hypertrophy of the lateral nail folds of the hallux may present at birth or in the first month of life as red, firm, enlarged masses of tissue that may cover significant amounts of the nail plate.64 If the induration persists, it may become painful or infected when the infant begins to crawl or walk. The condition usually remits spontaneously. A 2-week trial of a potent topical steroid solution (e.g., fluocinonide 0.05% twice daily) would not be unreasonable if surgical reduction of the excess tissue is contemplated.
Embedding of the distal free margin of the nail plate into the soft tissue of the hyponychium is not uncommon. A prominent ridge of tissue may form a wall that results in embedding or superior deflection of the nail plate. Most neonates outgrow these findings by 6 months of age.65 Some authors believe that factors such as sleeping prone, especially when the child begins to kick actively, and tight-fitting sleepsuits may predispose the older infant to paronychia.66
Paronychia and infectious nail dystrophy
Infections of the nail unit in neonates are extremely important to identify and treat promptly because of the possibility of irreversible damage to the nail matrix. Once the protective cuticle or hyponychium are compromised, then the matrix, an area of relative immune privilege, can be easily invaded.67 Acute paronychia presents with red, swollen, tender nail folds. Purulent material accumulates in the periungual groove and can extend under the nail plate. Chronic paronychia manifests with painless swelling of the nail fold, loss of the cuticle, and the development of granulation tissue. Organisms responsible for paronychia include Candida spp.,68 Staphylococcus, Streptococcus, Veillonella (in neonates),69 anaerobes, saprophytes, and herpes simplex. Paronychia is most common on the fingers as a result of developmentally appropriate sucking or mouthing of the digits. Systemic diseases associated with paronychia include mucocutaneous candidiasis, DiGeorge syndrome, acrodermatitis enteropathica, Langerhans’ cell histiocytosis,70 and HIV infections.71 Once diagnostic tests have been completed (e.g., cultures, Gram stain, potassium hydroxide preparation, and Tzanck preparation), treatment can be started. Burow’s solution soaks aid in gentle debridement of infected tissues. In mild cases, twice-daily use of topical solutions such as clindamycin or clotrimazole is indicated. Several days of concomitant applications of a topical steroid solution may reduce any pain and swelling. In more severe cases, purulent material may have to be surgically drained and granulation tissue may need to be cauterized.
Onychomycosis
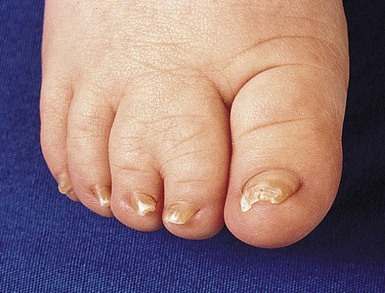
Onychomycosis is rare in neonates and infants yet the literature documents many case reports of dermatophyte infection occurring in the first few months of life.2–4,72 Tinea unguium may be less prevalent in this age group because of faster linear nail growth and subsequent elimination of fungi, a smaller contact surface, a lower incidence of tinea pedis, and less frequent exposure to fungi in public areas.73–75 A series of 16 patients under 2 years of age included seven cases of Down syndrome, two cases associated with preterm birth, and two others with perinatal hypoxia.76 There was a strong association of concomitant fungal infection in the families, with 14/16 fathers and 7/16 mothers having tinea pedis or onychomycosis. Toenails were more affected than fingernails. However, fingernail involvement is more common in young children than in adults.77
It is not surprising that Candida can affect neonates, as Candida species are known to be abundant in their environment, mostly affecting the skin and mucosa, and not the nails.78 In the neonatal and infant population, candidal onychomycosis has been documented to be caused by Candida albicans,79 Candida parapsilosis,80 and Candida tropicalis.78 Congenital candidiasis localized to the nails has been reported in premature and term newborns (Fig. 32.12).79,81 A potential source of infection is maternal vulvovaginitis, which may be asymptomatic, or associated with vaginal discharge that has resolved by the time nail changes are noted. Therefore, it is prudent to inquire about potential symptoms. In neonates, nail candidiasis has been associated with congenital cutaneous candidiasis.68,81,82 A series of six cases of isolated congenital nail candidiasis without other associated skin findings has been reported.83 In three cases, Candida vaginitis was diagnosed during the third trimester of pregnancy. Nail changes were noted at birth in two cases, and shortly afterwards (3 weeks to 1.5 months of life) in the remaining cases. All six had involvement of multiple fingernails, and in two cases, several toenails were affected as well. None were immunosuppressed or had chronic mucocutaneous disease.
Clinical features of onychomycosis in the neonate and infant are identical to those seen in older patients. Dystrophy includes thickening, a yellow discoloration, and subungual debris. White superficial onychomycosis has also been reported.84 Latent onychomadesis secondary to candidiasis has also been observed.85
A definitive diagnosis should be made before any treatment of neonatal onychomycosis. Either clippings sent for histology, fungal cultures, or potassium hydroxide preparations obtained by gentle curettage with a serrated curette can establish a diagnosis. Documentation of infection is important, especially when multiple nails are involved, since psoriasis, lichen planus, trachyonychia, yellow nail syndrome, and pachyonychia congenita are in the clinical differential diagnosis.
Topical therapy should be considered initially because of the lack of potential systemic side effects. It may work well in young children because of their relatively thin nail plates as well as presumed faster nail growth. There are neither published guidelines nor FDA approved medications for the treatment of onychomycosis in this age group. Topical antifungal agents including ciclopirox and amorolfine lacquers as well as bifonazole-urea ointment under occlusion can be successful76,86 over 6–12 weeks.87 Congenital candidal nail infection also responds to topical therapy. Agents reported to be successful include ciclopirox olamine 8% nail lacquer,79 clotrimazole 1% cream, ciclopirox olamine 1% cream, or combinations of the products. It should also be noted that at least one case of candida onychomycosis resolved spontaneously, after several months without any treatment.78
If oral medication with itraconazole, fluconazole or terbinafine is considered for refractory cases, monthly laboratory monitoring should be considered. An 8-week-old infant with Trichophyton rubrum affecting 18 nails responded to a combination of 8% ciclopirox nail lacquer and oral terbinafine at a dose of 25 mg/day; the infant weighed 6 kg.88 A premature infant that developed onychomycosis caused by Candida parapsilosis that affected multiple fingernails and toenails was treated successfully with systemic fluconazole 5 mg/kg per day for 30 days and topical ketoconazole once per day for 6 months,80 with a clinical response within 7 weeks.
Choice of potential therapies for onychomycosis in the neonatal and infant age group will depend on the number and severity of the nails affected, as well as the existence of other comorbid conditions.
Onycholysis
Separation of the nail plate from the nail bed is known as onycholysis. This usually occurs at the distal free edge of the nail plate, but may be observed laterally as well. The separation creates a narrow space that can fill with keratin, exogenous debris, or fluids such as water or saliva. The air pocket of the cleft gives an onycholytic nail a grayish-white color. Onycholysis is a physical sign for which there are numerous causes (Box 32.2).
Chromonychia
Nail dyschromia may be due to discoloration of the nail plate or nail bed (Table 32.2).89 The causes of nail discoloration may be exogenous, secondary to local infectious agents, systemic drugs or diseases, primary skin diseases, or ungual neoplasms (Fig. 32.13). The shape of the discolored area depends upon how and where in the nail unit the pigment is deposited, and the duration of the pigment deposition.
TABLE 32.2
Chromonychia (nails with abnormal color)
| Condition | Color | Other features |
| Hematomas | Purple | Observed on fingers, similar to sucking blisters (Fig. 32.13) |
| Endocarditis | Purple | Splinter-shaped |
| Phototoxicity | Purple | Drugs, porphyrias |
| Hyperbilirubinemia | Yellow-brown | Scleral icterus |
| Yellow nail syndrome | Yellow | Lymphedema, respiratory disease, nephrotic syndrome |
| Pernicious anemia | Blue-gray | Macrocytosis |
| Onychomycosis | Gray-green | Aspergillus, Pseudomonas |
| Candidiasis | White | |
| PCB exposure | Brown-gray | |
| Addison/Cushing disease | Brown |
Leukonychia (white nails) is the most common type of nail dyschromia.90 It should not be confused with onycholysis. Total or subtotal leukonychia may be inherited as an autosomal dominant trait.91 Partial leukonychia on the distal portion of the nail apparatus may be a sign of congenital candidiasis limited to the nail plates.92 Proximal partial leukonychia is also a sign of subungual onychomycosis from dermatophytes or other fungi.93 Transversely striated leukonychia in a longitudinal band may be observed after a febrile illness, similar to Beau’s lines. Multiple striations are associated with successive events that affect the matrix, including the administration of chemotherapeutic agents,94 the classic Mees’ lines of heavy metal intoxication, or Muehrcke’s paired lines of hypoalbuminemia. Muehrcke’s lines have also been described in the presence of zinc deficiency. Partial leukonychia in which the proximal portion of the nail is white has several eponyms. They include Lindsay’s half-and-half nails of uremia, and Terry’s nails secondary to cirrhosis or congestive heart failure. Leukonychia may also be a sign of malnutrition or iron deficiency anemia. Punctate leukonychia is manifested by small, irregular white spots. It is usually caused by repeated minor trauma to the nail matrix.
Single longitudinal pigmented bands of the nail in children are due to melanocytic lesions located in the nail matrix (Fig. 32.14).95 Multiple longitudinal pigmented bands are common in dark-skinned persons but are unusual in children. Multiple brown bands may be observed in fetal hydantoin syndrome, Addison and Cushing disease, Peutz–Jeghers syndrome, HIV, and after exposure to maternal chlorpromazine ingestion or other maternally ingested drugs.96 A study of longitudinal pigmented bands in 100 individuals found that 22 had nail matrix nevi.97 Twelve patients had lesions present at birth, and most were located on the fingernails. The bands were different shades, from light tan to black, and their width varied from 2 mm to the breadth of the entire nail plate. Periungual pigmentation (Hutchinson’s sign) was present in many of these benign lesions. In a series of eight cases of longitudinal melanonychia in children, four were present at birth.98 No cases of melanoma were documented in either series. There have even been isolated reports of spontaneous regression of ungual nevi.99 To date, six cases of melanoma of the nail unit in young children have been reported.100 Most cases of suspected ungual melanomas are probably benign Spitz nevi. Their pathology should be interpreted with caution, even by dermatopathologists. Most experts in nail diseases do not recommend biopsy of longitudinal pigmented bands unless a previously stable lesion undergoes progressive, rapid change. Biopsy specimens should be obtained from children who are predisposed to developing malignancies (e.g., xeroderma pigmentosum or dysplastic nevus syndrome). Improperly performed biopsies can lead to permanent nail dystrophy.

Access the full reference list at ExpertConsult.com ![]()