154a
Nail diseases: Psoriasis

Nail pitting is a change seen in psoriasis. The nails appear to have a tiny ice pick depression.

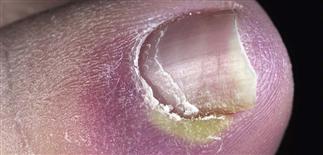
Affected by psoriasis, this nail has distal subungual hyperkeratosis, onycholysis, and a yellow-brown color change termed oil spot lesion, due to serum accumulation.

All five fingernails are affected with psoriasis. There is onycholysis and some yellow-brown discoloration typical of oil spot change.

The oil spot sign of psoriasis is a brown color. Often, there are other psoriasis findings such as onycholysis or pitting.
DESCRIPTION
Nail changes are characteristic of psoriasis, and the nails of all patients with suspect psoriasis should be examined. Psoriasis of the nails may be the only sign that the patient has psoriasis; these patients may have no skin lesions.
HISTORY
• The incidence of nail involvement in psoriasis varies from 10–50%. • Nail involvement may be the only sign of psoriasis, but it usually occurs simultaneously with skin disease. One or several nails may be involved. • Pain may restrict activities.
PHYSICAL FINDINGS
• Pitting is the most common finding. There may be a few or many pits, and they are haphazardly distributed on the nail plate surface. • Onycholysis is separation of the nail from the nail bed. Separation begins at the distal groove or under the nail plate and may involve several nails. The separated nail appears yellow and is often misinterpreted as a fungal infection. • Subungual scaly debris may accumulate under the distal nail plate. The yellow-white debris elevates the distal nail. This also is commonly mistaken for nail fungus infection. • Surface distortion of the nail plate occurs when psoriasis affects the nail matrix. • Oil spot lesions are yellow-brown spots seen through the nail surface. Psoriasis of the nail bed causes serum and scaling debris to accumulate under the nail plate. • Nail psoriasis may have a very similar appearance to tinea of the nail unit. Culture of nail clippings or subungual debris, potassium hydroxide preparations, and nail biopsy will help establish the diagnosis of fungal nail infection. Nail biopsy is performed by submitting nail clippings to the laboratory for histologic identification of hyphae to rule out fungal infection.
TREATMENT
• Many topical agents (calcipotriol, tazarotene, and anthralin) have been tried, but results are discouraging. • Intralesional injections at monthly intervals into the matrix and lateral nail folds are effective but painful. Triamcinolone acetonide (Kenalog) 2.5–5 mg/mL is delivered with a 30-gauge needle. The procedure is painful and most patients do not continue. • Treatment of skin disease with systemic agents such as tumor necrosis factor inhibitors adalimumab, etanercept, or other immune suppressive such as ciclosporin, methotrexate, or acitretin will improve the nails, but not indicated for nail disease alone.
154b
Nail diseases: Paronychia, Pseudomas infection, white spots or bands
Acute paronychia. The pus is collecting in the lateral nail fold and should be drained. The most common cause is Staphylococcus aureus.

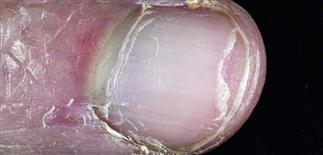
Chronic paronychia presents as swelling and tenderness of the proximal and lateral nail folds. The problem often occurs if there is repeated wet work. Candida is the most common cause.

Separation of the nail from the nail bed results in a warm moist space that predisposes to Pseudomonas infection (green color) under the nail. Soaking the finger makes it worse.

White spots in the nail plate, a very common finding, possibly result from cuticle manipulation or other mild forms of trauma. Psoriasis of the mid-nail matrix can also produce this change.
ACUTE PARONYCHIA
• Bacterial infection of proximal and lateral nail fold causes rapid onset of pain, swelling. • Caused by trauma and manipulation, or may occur spontaneously. • Pus accumulates behind cuticle or deeper in lateral nail folds. • Drain pus by inserting the pointed end of a comedone extractor or similar instrument between nail fold and nail plate. Pain is abruptly relieved. • Deeper infections may require incision to drain abscess. • Small confined abscesses may respond to just drainage. Larger abscesses with surrounding erythema treated with antistaphylococcal antibiotics.
CHRONIC PARONYCHIA
• Contact irritant exposure is major cause. Bakers, dishwashers, surgeons, dentists at risk. • Many or all fingers are involved. Tenderness, erythema, and mild swelling about the proximal and lateral nail folds. • Cuticle disappears, leaving space between proximal nail fold and nail plate exposed to infection. Manipulation of the cuticle accelerates the process. • Bacteria and yeast grow in the warm moist space under the proximal nail fold. • Chronic inflammation causes nail plate to be distorted, but it remains uninfected. • Psoriasis may have an identical appearance. • Goals of treatment are to avoid irritation and to suppress inflammation and infection. • Protect by wearing vinyl gloves with cotton glove underneath (http://www.allerderm.com). • Group V topical steroids and not oral antibiotics are mainstay of treatment. • Fungoid tincture (miconazole) is applied twice daily to proximal nail fold and allowed to flow into the space created by the absent cuticle. Cuticle may never re-form in patients with long-standing inflammation. • Fluconazole (150 mg q.d.) for 1–2 weeks may control treatment-resistant cases. Short courses of fluconazole may have to be repeated as the infection recurs.
PSEUDOMONAS INFECTION
• Separation of the nail plate (onycholysis) exposes a damp, macerated space between nail plate and nail bed. • Pseudomonas thrives in this warm moist space and stains the nail plate undersurface green-black. Little discomfort or inflammation, as occurs with subungual hematoma. • Apply a few drops of a bleach mixture (one part chlorine bleach to four parts water) under the nail three times daily. Vinegar (acetic acid) may also be used. • Cut unattached nail to eliminate damp space under the nail.
WHITE SPOTS OR BANDS
• White spots in the nail plate are common. • Probably a result of repeated low-grade trauma. • The spots or bands eventually grow out and disappear. Patients often misinterpret this finding as a fungal infection.
154c
Nail diseases: Ridging and beading, habit tic deformity, onycholysis

Longitudinal ridging is common in aging. Beading occurs at all ages but is more common in the elderly. The beads cover part or most of the plate surface and are arranged longitudinally.

Horizontal nail plate indentations along the length of the nail are the hallmark of habit tic nail deformity. Repeated trauma from a habit of rubbing or pushing on the proximal nail fold causes this.

Distal separation of the nail plate from the nail bed is called onycholysis. Some causes are trauma, psoriasis, tinea, and phototoxic drug reaction.
Distal splitting of the nail plate is a common complaint without a simple fix. Hydration of the plate with a thick emollient can be helpful.
RIDGING AND BEADING
• Longitudinal ridging is a common aging change that is occasionally seen in young people. Beading occurs at all ages but is more common in the elderly. • The beads cover part or most of the plate surface and are arranged longitudinally. • Patients may sand or buff the nail to smooth the surface. • Elon nail conditioner (http://www.ilovemynails.com) prevents dryness and cracking.
HABIT TIC DEFORMITY
• Biting or picking a section of the proximal nail fold of the thumb with the index fingernail is a common habit. Other nails can be affected. • Linear bands of horizontal grooves extend up the nail surface. Nail rippling from chronic eczema of the proximal nail fold causes a similar appearance. • Patients who can stop this habit will eventually regrow normal nails.
ONYCHOLYSIS
• Onycholysis is the separation of the nail from the nail bed. It is more common in women with long nails. Vigorous cleaning under the nail accelerates the process. • Separation begins at the distal end and slowly progresses proximally. • The non-adherent portion of the nail is white, yellow, or green-tinged. • Causes include psoriasis, trauma to long nails, Candida or Pseudomonas infections, internal drugs, contact with chemicals, maceration from prolonged immersion, and allergic contact dermatitis (e.g. to nail hardener or adhesives). • Screen patients with unexplained onycholysis for hyperthyroidism and asymptomatic thyroid disease. • Treat by cutting the separated portion of the nail. This promotes dryness and discourages infection under the nail. Do not soak the fingertip. • Avoid exposure to contact irritants. • Yeast grows in the space between the nail and nail bed. Use liquid topical agents (e.g. fungoid tincture that contains miconazole). Consider oral fluconazole (Diflucan) for resistant cases. A short course of fluconazole (e.g. 150 mg every day for 5–7 days) may have to be repeated as the nail grows out.
DISTAL PLATE SPLITTING
• Brittle nails and splitting are found in 20% of adults. • The splitting into layers or peeling of the distal nail plate resembles the scaling of dry skin. • Nails, like the skin, dry in the winter. Repeated water immersion encourages the process. Vinyl gloves protect during wet work. • Rehydrate the nail by soaking in water. Then apply a thick lubricant such as Aquaphor ointment or Elon nail conditioner (http://www.ilovemynails.com). These are found in some pharmacies. • The B-complex vitamin biotin (2.5 mg q.d.) may improve nail plate thickness and integrity.
154d
Nail diseases: Digital mucous cyst, nevi and melanoma, hematoma
A flesh-colored, almost translucent, rounded cystic papule is present on the distal fingertip. Such digital mucous cysts can compress the matrix and result in a longitudinal nail plate depression.

Digital mucous cyst: incision with a #11 surgical blade. A clear, sometimes blood-tinged, viscous, jelly-like substance exudes when the cyst is incised.

Melanoma: Hutchinson sign. Pigment that extends on to the nail folds is a sign of subungual melanoma. In this case, the pigment extension is marked.

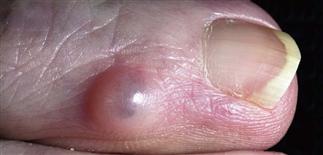
Trauma to the nail plate can result in subungual hemorrhage. The hemorrhage is trapped by the nail plate; the resultant pressure can be tender until relieved by drainage.
DIGITAL MUCOUS CYSTS
• Digital mucous cysts are focal collections of mucin lacking a cystic lining. • These dome-shaped, pink-white structures occur on the dorsal surface of the distal phalanx of middle-aged and elderly people. • A clear, viscous, jelly-like substance exudes when the cyst is incised. • Cysts on the proximal nail fold compress the nail matrix cells and induce a longitudinal nail groove. • Surgical excision by a qualified hand surgeon to remove lesion if painful. Otherwise, these benign lesions should be left alone.
NEVI AND MELANOMA
• Junctional nevi can appear in the nail matrix and produce a brown pigmented band. Brown longitudinal bands are common in black people but rare in white people. • Melanoma of the nail can occur anywhere around or under the nail. • The lesion may present as a pigmented band that increases in width. The spontaneous appearance of such a band is noteworthy and concerning; such lesions should be biopsied. • Benign subungual nevi are rare in white people, so subungual nevoid lesions should be regarded as malignant until proved otherwise. • Hutchinson sign is the periungual extension of brown-black pigmentation from longitudinal melanonychia on to the proximal and lateral nail folds. It is an important indicator of subungual melanoma. • When there is suspicion of subungual melanoma, biopsy should not be delayed. A dermatologist or plastic surgeon familiar with nail biopsy techniques is best to perform this procedure.
SUBUNGUAL HEMATOMA
• Trauma to the nail plate may cause immediate bleeding and pain. Bleeding may cause separation and more pain. • Puncture the nail surface with a red-hot paper clip tip to drain the blood. • Trauma to the proximal nail fold causes hemorrhage that may not be apparent for days. The nail plate may emerge from the nail fold with bloodstains and mimic melanoma.







