N
naevus Any localized area of pigmentation or vascularization of the skin or eye tissues, usually benign and congenital. Note: also spelt nevus. Plural: naevi.
choroidal n. A benign accumulation of melanocytes in the choroid. It affects some 10% of the population. Ophthalmoscopically it appears as a slate-grey lesion, flat or minimally elevated, oval or circular. It is asymptomatic. With time drusen may also appear.
See melanocyte; melanoma, choroidal.
conjunctival n. A naevus located on the conjunctiva, most often near the limbus. It appears as a yellowish-red area or deeply pigmented mass usually before the age of 20. A pigmented conjunctival naevus must be distinguished from an acquired melanoma of the conjunctiva which occurs later in life (after the third decade, is typically unilateral and may become malignant). A conjunctival naevus rarely becomes malignant. It can be excised if cosmetically undesirable or has enlarged to such a degree as to irritate the eye.
flammeus n. See syndrome, Sturge–Weber.
iris n. A pigmented spot of variable size on the surface of the iris. It is composed of an accumulation of melanocytes in the iris stroma. It is usually benign but occasionally it may transform itself into a malignant melanoma.
See melanocyte; melanoma, iris; syndrome, ICE.
n. of Ota A benign, congenital, usually unilateral, accumulation of melanocytes on the cheek, eyelids, forehead, nose or sclera. Some naevi may become malignant melanoma. Syn. oculocutaneous melanosis; oculodermal melanocytosis.
See melanocytosis, ocular; melanosis.
Nagel anomaloscope See anomaloscope.
nanometre (nm) SI unit of length equal to one-millionth of a millimetre (or 10 ångströms or 10–9 m). Syn. millimicron (obsolete).
See ångström; micrometre.
nanophthalmos See microphthalmia.
naphazoline hydrochloride A sympathomimetic vasoconstrictor, which may be used as a topical decongestant in 0.1% eyedrops. It causes slight mydriasis. It also comes as naphazoline nitrate.
See adrenaline (epinephrine); decongestant, ocular.
narrow-angle glaucoma See glaucoma, angle-closure.
nasal step See Roenne nasal step.
nasolacrimal duct See lacrimal apparatus.
nasotemporal overlap A vertical strip passing through the fovea and above and below it, within which retinal ganglion cells may send their axons either ipsilaterally or contralaterally. The width of this strip is less than 1° in the central retina and increases to several degrees in the upper and lower areas. Therefore information from the fovea and a small area around it is projected to both sides of the visual cortex and this may have some involvement with stereopsis. Syn. bilateral strip.
natamycin See antifungal agent.
nativism The belief that knowledge or behaviour is inborn.
See empiricism; theory, nativist.
nativist theory See theory, nativist.
Nd-Yag laser See laser, neodymium-yag.
near addition See addition, near.
near point of accommodation See accommodation, near point of.
near point of convergence See convergence, near point of.
near point retinoscopy See retinoscopy, dynamic.
near point rule; point sphere See under the nouns.
near point stress See asthenopia.
near reflex See reflex, accommodative.
near sight See myopia.
near triad See reflex, accommodative.
near vision; visual acuity See under the nouns.
nearsightedness See myopia.
nebula See leukoma.
Necker cube Perspective drawing of the outline of a cube that can induce two perceptions, either a three-dimensional cube orientated upward or a three-dimensional cube orientated downward (Fig. N1).
See figure, Blivet; Rubin’s vase; Schroeder’s staircase.
necrosis Death of some or all cells in an organ or tissue. The process involves swelling of the nucleus (pyknosis), fragmentation of the nucleus (karyorrhexis) and complete dissolution of the nuclear chromatin (karyolysis). Necrosis is caused by disease, trauma or interference with blood supply. There are many sequelae to ocular necrosis (e.g. inflammation, reduction in aqueous humour production following ciliary epithelium necrosis, corneal opacity following necrosis of corneal epithelial cells, and visual loss and floaters following retinal necrosis).
See apoptosis; retinal necrosis.
necrotizing scleritis See scleritis, necrotizing.
nedocromil sodium See mast cell stabilizers.
negative convergence See divergence.
negative eyepiece See eyepiece, negative.
negative relative accommodation See accommodation, relative amplitude of.
negative relative convergence See convergence, relative.
negative scotoma See scotoma, negative.
negative spherical aberration See aberration, spherical.
neglect, visual See visual neglect.
neodymium-yag laser See laser neodymium-yag.
neomycin sulfate A broad-spectrum antibiotic agent effective against gram-negative and gram-positive organisms, although it is not effective against Pseudomonas aeruginosa. It may be applied topically as eyedrops or eye ointment, but it is most commonly combined with bacitracin and polymyxin B. Syn. framycetin (a mixture of neomycin A, neomycin B and neomycin C).
neonatal conjunctivitis See ophthalmia neonatorum.
neostigmine A reversible anticholinesterase drug, which neutralizes the effect of acetylcholinesterase and thereby allows the prolonged action of acetylcholine on the iris and ciliary muscle. Its action is similar to physostigmine but it is not so irritating a miotic. Both are occasionally used in the treatment of glaucoma.
See acetylcholine; parasympathomimetic; physostigmine; miosis; miotics.
neovascular glaucoma See glaucoma, neovascular.
neovascularization Development of new blood vessels, especially in tissues where circulation has been impaired by disease or trauma.
choroidal n. (CNV) Abnormal growth of blood vessels, originating in the choriocapillaris, which pass through Bruch’s membrane and then proliferate under the retinal pigment epithelium (type 1) and/or under the retina (type 2). It may occur as a result of a rupture of Bruch’s membrane, release of cytokines (e.g. VEGF), inflammation, oxidative stress to the retinal pigment epithelium, or vascular insufficiency. The condition is the main cause of exudative (wet) age-related macular degeneration and it may be associated with various disorders including angioid streaks, choroidal rupture, pathological myopia, chorioretinal scars and birdshot retinochoroidopathy.
See macular degeneration, age-related.
corneal n. See pannus.
iris n. Abnormal formation of new blood vessels on the anterior surface of the iris. It is commonly associated with many conditions that have led to retinal ischaemia, such as diabetic retinopathy, occlusion of the central retinal vein, carotid arterial disease, uveal melanoma, long-standing retinal detachment, etc. The neovascularization begins at the pupil margin and often at the same time in the angle of the anterior chamber and spreads over the whole surface. New vessels are associated with fibrous tissue membranes, which may block the passage of aqueous humour through the trabecular meshwork (neovascular glaucoma) and ectropion uveae near the pupillary margin. Treatment typically includes photocoagulation to prevent the formation of new blood vessels.
nepafenac See antiinflammatory drug.
nerve A whitish cord made up of myelinated or unmyelinated nerve fibres held together by connective tissue sheath in bundles and through which stimuli are transmitted from the central nervous system to the periphery or vice versa.
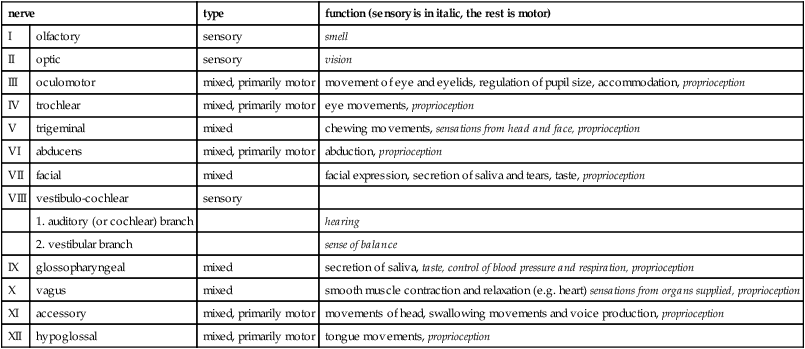
abducens n. Sixth cranial nerve. It has its origin from the abducens nucleus at the lower border of the pons and at the lateral part of the pyramid of the medulla. It passes through the cavernous sinus and enters the orbit through the superior orbital fissure. It supplies motor innervation to the ipsilateral lateral rectus muscle. Additionally, interneurons leave the abducens nucleus and project to the contralateral medial rectus sub nucleus to allow conjugate gaze. A lesion in the nuclear region will cause gaze palsy, whereas an abducens nerve lesion will produce only an abduction deficit. See nucleus, abducens; paralysis of the sixth nerve.
cranial n’s. Twelve pairs of nerves, one set on each side of the brain, that emerge, or enter the cranium. They carry sensory information from the sense organs, the muscles of the head, neck, shoulders, heart, viscera and vocal tract. The motor neurons with axons in the cranial nerves control pupil diameter, accommodation, movements of the eyes and eyelids, mastication, facial expression, head movements, as well as cardiorespiratory and digestive functions.
n. fibre layer See retina.
fifth cranial n. See nerve, trigeminal.
fourth cranial n. See nerve, trochlear.
frontal n. See nerve, ophthalmic.
n. impulse See potential, action.
infratrochlear n. See nerve, ophthalmic.
lacrimal n. See nerve, ophthalmic.
long ciliary n. One of a pair of nerves that comes off the nasociliary nerve and runs with the short ciliaries, pierces the sclera, travels in the suprachoroidal space and supplies sensory fibres to the iris, cornea, and ciliary muscle and sympathetic motor fibres to the dilator pupillae muscle (Fig. N2).
Table N1
Cranial nerves
| nerve | type | function (sensory is in italic, the rest is motor) | |
| I | olfactory | sensory | smell |
| II | optic | sensory | vision |
| III | oculomotor | mixed, primarily motor | movement of eye and eyelids, regulation of pupil size, accommodation, proprioception |
| IV | trochlear | mixed, primarily motor | eye movements, proprioception |
| V | trigeminal | mixed | chewing movements, sensations from head and face, proprioception |
| VI | abducens | mixed, primarily motor | abduction, proprioception |
| VII | facial | mixed | facial expression, secretion of saliva and tears, taste, proprioception |
| VIII | vestibulo-cochlear | sensory | |
| 1. auditory (or cochlear) branch | hearing | ||
| 2. vestibular branch | sense of balance | ||
| IX | glossopharyngeal | mixed | secretion of saliva, taste, control of blood pressure and respiration, proprioception |
| X | vagus | mixed | smooth muscle contraction and relaxation (e.g. heart) sensations from organs supplied, proprioception |
| XI | accessory | mixed, primarily motor | movements of head, swallowing movements and voice production, proprioception |
| XII | hypoglossal | mixed, primarily motor | tongue movements, proprioception |
See nerve, ophthalmic; reflex, pupil light.
nasociliary n. See nerve, ophthalmic.
oculomotor n. Third cranial nerve. It is classified as a motor nerve. Its origin lies in the tegmentum of the midbrain. It passes through the cavernous sinus and just before it enters the orbit it divides into a small superior and a larger inferior division. Both divisions penetrate into the orbit through the superior orbital fissure. In the orbit the superior division passes inward above the optic nerve to supply the superior rectus and the levator palpebrae superioris muscles. The inferior division sends branches to the medial rectus, the inferior rectus and inferior oblique muscles, as well as providing parasympathetic fibres to the sphincter pupillae and ciliary muscles via a branch to the ciliary ganglion.
See nucleus, oculomotor; paralysis of the third nerve.
ophthalmic n. This is the smallest of the three divisions of the trigeminal nerve, the other two being the maxillary and mandibular branches. It comes off the medial and upper part of the convex anterior border of the gasserian ganglion (trigeminal ganglion), passes through the cavernous sinus and just behind the superior orbital fissure it divides into three branches, the lacrimal, frontal and nasociliary, which pass through the fissure to enter the orbit. (1) The smallest of the three, the lacrimal nerve, supplies sensory fibres to the lacrimal gland, the skin of the upper eyelid and the conjunctiva. Just before reaching the gland the nerve communicates with the zygomaticotemporal nerve (itself a branch of the zygomatic nerve). This branch contains parasympathetic fibres from the facial nerve that pass to the lacrimal gland. (2) The frontal nerve, which is the largest of the three divisions, divides into the supratrochlear and supraorbital nerves. The supratrochlear further anastomoses with the infratrochlear nerve and supplies the lower part of the forehead, the upper eyelid and the conjunctiva. The infratrochlear supplies sensory fibres to the skin and conjunctiva round the inner angle of the eye, the root of the nose, the lacrimal sac and canaliculi and caruncle. The supraorbital nerve sends sensory fibres to the forehead, the upper eyelid and conjunctiva. (3) The nasociliary nerve gives origin to several nerves: the long ciliary nerves, the long or sensory root (ramus communicans) to the ciliary ganglion, the posterior ethmoidal nerve and the infratrochlear nerve (Fig. N2).
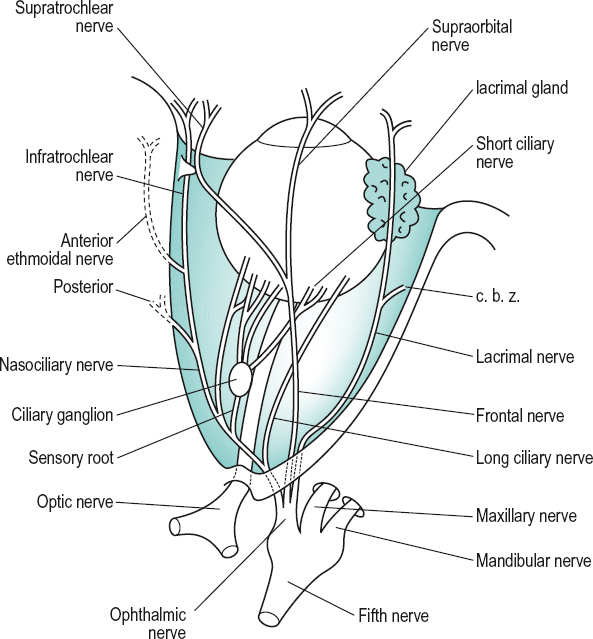
optic n. Second cranial nerve. It forms a link in the visual pathway. It takes its origin at the retina and is made up of nearly 1.2 million fibres from the ganglion cells and some efferent fibres that end in the retina. The nerve runs backward from the eyeball and emerges from the orbit through the optic canal and then forms the optic chiasma. The total length of the optic nerve is 5 cm; the portion before the chiasma called intracranial being about 1 cm, the intracanalicular 6 mm, the intraorbital 3 cm and the intraocular 0.7 mm. The optic nerve is more often divided into only two portions: the intraocular (bulbar) portion and the orbital (retrobulbar) portion (Fig. N2).
See atrophy, optic; fibres, pupillary; neuritis, optic; neuropathy, anterior ischaemic optic; papilloedema.
short ciliary n. One of six to ten branches from the ciliary ganglion that enters the eye around the optic nerve, travels in the suprachoroidal space and innervates the ciliary muscle, the sphincter pupillae muscle and the cornea.
See reflex, pupil light.
sixth cranial n. See nerve, abducens.
supraorbital n.; supratrochlear n. See nerve, ophthalmic.
third cranial n. See nerve, oculomotor.
trigeminal n. Fifth cranial nerve. It is the largest of the cranial nerves. It originates above the middle of the lateral surface of the pons as two divisions, a larger sensory root and a motor root. The sensory root passes to the gasserian ganglion (trigeminal ganglion) and from that ganglion the three divisions of the fifth nerve are given off: the ophthalmic, maxillary and mandibular nerves. The fifth nerve is sensory to the face, the eyeball, the conjunctiva, the eyebrow, the teeth, the mucous membranes in the mouth and nose. The motor root of the nerve has no connection with the ganglion. It joins the mandibular nerve and is motor to the muscles of mastication.
trochlear n. Fourth cranial nerve. It is the most slender of the cranial nerves but with the longest intracranial course (75 mm). It is the only motor nerve that originates from the dorsal surface of the brain between the midbrain and the cerebellum. It passes through the cavernous sinus and then enters the orbit through the superior orbital fissure and supplies motor fibres to the superior oblique muscle.
See nucleus, trochlear; paralysis of the fourth nerve.
zygomatic n. A branch of the maxillary division of the trigeminal nerve, it enters the orbit by the inferior orbital fissure and soon divides into the zygomaticotemporal and zygomaticofacial branches. The former gives a twig to the lacrimal nerve and is thought to conduct autonomic fibres to the lacrimal gland and the latter supplies the skin over the zygomatic bone.
neural rim See neuroretinal rim.
neuritis, optic Inflammation of the optic nerve, which can occur anywhere along its course from the ganglion cells in the retina to the synapse of these cell fibres in the lateral geniculate body. If the inflammation is restricted to the optic nerve head the condition is called papillitis (or intraocular optic neuritis) and if it is located in the orbital portion of the nerve it is called retrobulbar optic neuritis (or orbital optic neuritis).
In papillitis the optic nerve head is hyperaemic with blurred margins and slightly oedematous. Haemorrhages and exudates may also appear. In retrobulbar optic neuritis, there are usually no visible signs in the fundus of the eye until the disease has advanced and optic atrophy may appear. However, both types are accompanied by a loss of visual acuity along with a central scotoma and impairment of colour vision. The loss of vision may occur abruptly over a few hours and recovery may be equally rapid but in some patients the loss may be slow. In retrobulbar optic neuritis, there is also pain on movement of the eyes and sometimes tenderness on palpation. The disease is usually unilateral although the second eye may become involved later. It is usually transient and full or partial recovery takes place within weeks. The primary cause of optic neuritis is multiple sclerosis but it may also be associated with severe inflammation of the retina or choroid, vitamin B deficiency, diabetes mellitus, thyroid disease, lactation, toxicity or syphilis.
See disease, Devic’s; papilloedema; pupil, Marcus Gunn; rule, Kollner’s; test, photostress.
neurofibromatosis type 1 See disease, von Recklinghausen’s.
neurofibromatosis type 2 An autosomal dominant inherited disease with a gene locus at 22q12 characterized by bilateral acoustic neuromas, meningioma, glioma and Schwannoma. Ocular manifestations are juvenile cataract and hamartoma (benign tumour-like nodules) of the retina and retinal pigment epithelium. It is much less common than neurofibromatosis type 1 (von Recklinghausen’s disease).
See retinal pigment epithelium, congenital hypertrophy of the.
neuroimaging, functional Methods used to detect structural abnormalities in the central nervous system and localized brain neural activity in response to performing specific sensory, motor and cognitive tasks. Two common methods are functional MRI (fMRI) and positron emission tomography (PET). These techniques can be used to detect tumours, strokes, focal cerebral lesions, and to map the cortex in healthy individuals.
See magnetic resonance imaging; tomography, computed; tomography, positron emission.
neuromyelitis optica See disease, Devic’s.
neuron Structural unit of the nervous system consisting of the nerve cell body and its various processes, the dendrites, the axon and the ending (also called bouton, end foot or axon terminal). There are many types of neurons within the nervous system; some transmit afferent nerve impulses to the brain (e.g. those carrying information from the photoreceptors to the visual cortex), or to the spinal cord (e.g. those carrying information from the receptors in the skin to the spinal cord). They are called sensory neurons. Others transmit efferent motor nerve impulses to a muscle (e.g. those carrying information from the Edinger–Westphal nucleus to the sphincter pupillae and ciliary muscles). These are called motor neurons. Other neurons carry nerve impulses from one neuron to another (internuncial neurons). Note: also spelt neurone.
See potential, action; synapse.
neuroparalytic keratitis See keratitis, neuroparalytic.
neuropathy, anterior ischaemic optic (AION) A group of disorders that have in common ischaemia of the anterior portion of the optic nerve (especially the optic nerve head). Affected patients, usually between 50 and 75 years of age, present with sudden, severe visual loss often accompanied by periocular pain and jaw claudication. The disc is pale and swollen and severe optic atrophy eventually ensues. Ischaemia is due either to inflammation of the arterioles (posterior ciliary arteries) supplying blood to the anterior portion of the optic nerve (i.e. arteritic) or to an idiopathic aetiology (i.e. non-arteritic). Arteritic AION generally affects older individuals and is most commonly associated with temporal (giant cell) arteritis. Systemic findings include weight loss, malaise, scalp and joint pain and tenderness, and possibly hypertension. Rapid diagnosis and treatment (usually corticosteroids) is crucial in order to avoid permanent visual loss as well as systemic complications. Non-arteritic AION generally affects younger patients and causes severe visual loss. There are few systemic effects of the condition. No specific treatment has been identified.
See arteriosclerosis; hemianopia, altitudinal.
neuropathy, Leber’s optic See Leber’s hereditary optic atrophy.
neuropathy, optic A non-inflammatory or degenerative disease of the optic nerve.
See ophthalmopathy.
neuroprotection A therapeutic strategy aimed at preventing the ultimate result of a neurodegenerative disease process. Example: in current glaucoma therapy, the principal objective is to lower the intraocular pressure, but that appears to be only one of the risk factors that lead ultimately to shrinkage and/or death of retinal ganglion cells and visual field loss. Visual field losses occur even after the intraocular pressure is returned to within the normal range in some patients. Neuroprotection is aimed at preventing that secondary ganglion cell degeneration in glaucomatous eyes, which may have been caused as a result of inflammatory or toxic mediators released by the primary degenerative event. Neuroprotective strategies presently being evaluated include glutamate antagonists, calcium channel blockers, nitric oxide synthase inhibitors and neurotrophins.
neuroretinal rim A term used in describing the area of the optic disc which contains the neural elements and is located between the edge of the disc and the physiological cup. When describing the neuroretinal rim, as is often done in cases of glaucoma, one must include its colour, size, slope and uniformity. Syn. neural rim.
neuroretinitis Inflammation of the optic nerve head and adjacent retina. It is characterized by optic disc oedema, loss of vision, macular exudates, which frequently form a star-like pattern, and whitish lesions scattered throughout the fundus. A common cause is viral infection and it may also appear as a complication of syphilis.
neurosensory retina See retina, neurosensory.
neurotransmitter A substance stored in the synaptic vesicles that is released when the axon terminal is excited by a nervous impulse. The substance then travels across the synaptic cleft to either excite or inhibit another neuron. This is accomplished by either decreasing the negativity of postsynaptic potentials (excitation), or increasing the negativity of postsynaptic potentials (inhibition). Common neurotransmitters include acetylcholine, dopamine, endorphins, adrenaline (epinephrine), gamma-aminobutyric acid (GABA), amino acids, such as glutamate and glycine, noradrenaline (norepinephrine), serotonin and substance P. Common neurotransmitters in the retina are glutamate (the primary excitatory neurotransmitter), GABA (inhibitory), glycine (inhibitory), dopamine (excitatory) and acetylcholine (excitatory).
neurotrophic keratitis; keratopathy See keratopathy, neurotrophic.
neutral density filter See filter.
neutral point See point, neutral.
neutralization 1 . A technique for determining the power of an ophthalmic lens. It is accomplished by placing a lens of known power and opposite sign in contact with the unknown lens and moved back and forth in a plane perpendicular to the line of sight until the observation of movement (against or with) of the distant image seen through the lenses disappear. The unknown lens will have the opposite power to that which neutralizes this apparent movement. 2. A method of breaking down hydrogen peroxide from a contact lens (mostly soft) following contact lens disinfection to avoid possible irritation to ocular tissues. This can be achieved by rinsing and dilution with saline, by using a solution with an enzyme catalase or a platinum disc incorporated into the lens case, or with a chemical agent such as sodium pyruvate or sodium thiosulfate. See disinfection; focimeter.
nevus See naevus.
New Aniseikonia Test See test, New Aniseikonia.
Newton’s formula An expression relating the focal lengths of an optical system (f and f’) and the object x and image x’ distances measured from the respective focal points. Thus,
< ?xml:namespace prefix = "mml" />

If the optical system is a lens in air –f = f’ and the formula becomes

Syn. Newton’s equation; Newton’s relation.
See paraxial equation, fundamental; sign convention; theory, gaussian.
Newton’s rings; theory See under the nouns.
newtonian telescope See telescope.
nicotine An alkaloid with pharmacological actions similar to those of acetylcholine at autonomic ganglia and skeletal neuromuscular junctions.
See acetylcholine; cholinergic.
nictitating membrane See membrane, nictitating.
Niemann–Pick disease See disease, Niemann–Pick.
night blindness See hemeralopia.
night vision See vision, scotopic.
nit See candela per square metre.
nocturnal vision See vision, scotopic.
nodal plane; points See under the nouns.
nodes of Ranvier See cell, Schwann.
nodule A small, circumscribed mass of tissue or an aggregation of cells.
Busacca’s n’s. Nodules often found in the iris stroma of an eye affected by granulomatous uveitis (up to about 30% of cases). Syn. floccules of Busacca.
See nodules, iris.
Dalen–Fuchs n’s. Multiple, small yellow-white mounds consisting mainly of epithelial cells protruding through the retinal pigment epithelium. They are seen in the fundus of an eye with sympathetic ophthalmia, Vogt– Koyanagi–Harada syndrome or some other granulomatous inflammations.
iris n’s. Small, solid elevations found on the iris and epithelial cells and lymphocytes. They are usually whitish or grey, depending on their location.
See nodules, Busacca’s; nodules, Koeppe’s; nodule, Lisch.
Koeppe’s n’s. Small nodules frequently found on the iris around the pupillary margin of an eye affected by granulomatous uveitis.
See nodules, iris.
Lisch n. A small, abnormal, lightly pigmented swelling which develops on the surface of the iris in almost all patients with neurofibromatosis type 1 during the second or third decades of life.
See disease, von Recklinghausen’s.
nomogram See tonography.
non-concomitance See incomitance.
non-contact tonometer See tonometer, non-contact.
non-invasive break-up time test See test, non-invasive break-up time.
non-steroidal antiinflammatory drug See antiinflammatory drug.
nonius horopter See horopter, nonius.
noradrenaline (norepinephrine) A neurohumoral transmitter for most postganglionic sympathetic fibres. It is produced with adrenaline (epinephrine) in the adrenal medulla. It is a powerful excitator of α-adrenergic receptors.
See adrenaline (epinephrine); adrenergic receptors; mydriatic; neurotransmitter.
norepinephrine See noradrenaline.
norfloxacin See antibiotic.
normal retinal correspondence See retinal corresponding points.
normal saline See saline, physiological.
Norrie’s disease See disease, Norrie’s.
nose pad See pad.
nuclear layer, inner retinal See retina.
nucleus 1 . A mass of grey matter composed of nerve cell bodies in any part of the brain or spinal cord and dealing with a common function. 2. Core or central portion of the cell body of a neuron, containing cellular DNA in particular. Plural: nuclei.
abducens n. Nucleus of the abducens nerve (sixth cranial nerve) located in the lower part of the pons and whose axons supply the lateral rectus muscle.
accessory oculomotor n. See nucleus, Edinger–Westphal.
n. of the crystalline lens See lens, crystalline.
Edinger–Westphal n. Part of the oculomotor nucleus, it is situated posterior to the main nucleus and contains the parasympathetic component of the complex. Axons from the Edinger–Westphal pass out along the third (or oculomotor) nerve to synapse in the ciliary ganglion. Postganglionic fibres pass through the short ciliary nerves to the sphincter pupillae and ciliary muscles. The nucleus also receives fibres concerned with accommodation and fibres from the pretectal nucleus dealing with pupil light reflexes. Syn. accessory oculomotor nucleus; accessory parasympathetic nucleus.
See nucleus, pretectal; reflex, pupil light lateral n. Part of the oculomotor nucleus which supplies, via the oculomotor nerve, all the extraocular muscles except the superior oblique and the lateral rectus muscles. lateral geniculate n.
See geniculate body, lateral.
oculomotor n. This is the nucleus of the oculomotor nerve (third cranial nerve). It is a complex mass of cells located in the midbrain at the level of the superior colliculus and beneath the cerebral aqueduct (of Sylvius) which connects the third and fourth ventricles. It is divided into several subnuclei.
See nerve, oculomotor; nucleus, Edinger– Westphal; nucleus, Perlia’s; nucleus, trochlear.
olivary n. See pretectum; reflex, pupil light.
Perlia’s n. Midline part of the oculomotor nucleus. It is rudimentary in man and primates and may provide part of the innervation of the superior rectus muscle.
pretectal n. A complex group of nerve cells in the midbrain anterior to the superior colliculi. One of these, the pretectal olivary nucleus, receives retinal inputs via the optic tract and superior brachium and sends axons to both Edinger–Westphal nuclei. It constitutes a centre of the pupil light reflex. Another, the nucleus of the optic tract, may be involved in the control of reflex eye movements. Other fibres from the pretectal nucleus innervate the cornea, the iris, the ciliary muscle and the extraocular muscles (except the lateral rectus and superior oblique muscles), as well as the levator palpebrae muscle.
trochlear n. A nucleus of the trochlear nerve (fourth cranial nerve) located at the level of the inferior colliculus and below the posterior end of the oculomotor nerve nucleus, it sends fibres to the contralateral superior oblique muscle.
null point See nystagmus.
nyctalopia See blindness, congenital stationary night; hemeralopia.
nystagmograph Instrument for recording the movements of the eyes in nystagmus.
nystagmoid Resembling nystagmus.
nystagmus A regular, repetitive, involuntary movement of the eye whose direction, amplitude and frequency are variable. Nystagmus can be induced, acquired or congenital. (In a very small percentage of people it can even be induced voluntarily.) These eye movements typically appear as one of two types: pendular nystagmus or jerk nystagmus (Fig. N3). Jerk nystagmus is one in which there is a slow and fast phase, the nystagmus being conventionally defined by the direction of the fast phase. A feature of jerk nystagmus is the null zone (or null point) which represents the direction of gaze at which the nystagmus has the smallest amplitude. A jerk nystagmus is usually due to a motor defect that may be induced by brainstem or cerebellar lesions, drug intoxication (upbeat nystagmus in which the fast phase is in the upward direction or downbeat nystagmus in which the fast phase is downward); associated with a lesion of the central nervous system or the vestibular nerve or nuclei (central nystagmus and vestibular nystagmus); or to disease or injury to the labyrinth (labyrinth nystagmus); or to multiple sclerosis. Jerk nystagmus can also be induced physiologically, as for example optokinetic nystagmus (OKN) or train nystagmus, which occurs when watching objects that traverse the visual field rapidly, or as a result of thermal stimulation of the labyrinth of the inner ear by cold or hot water (caloric nystagmus or Barany’s nystagmus), or when the eyes of a fatigued person are turned into an extreme position of gaze (end-point nystagmus), or when a person who had been spinning round is stopped (vestibular nystagmus).
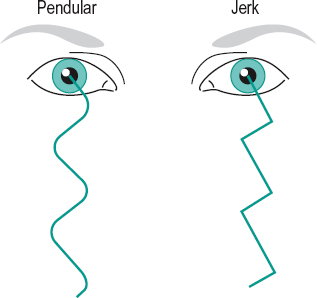
The other type is a nystagmus which is characterized by movements of equal velocity in each direction, the pendular nystagmus. A pendular nystagmus usually occurs as a result of poor central vision (sensory deprivation nystagmus) as in bilateral chorioretinitis, total colour blindness, albinism, congenital cataract, corneal scarring, amblyopia (amblyopic nystagmus) or in coal miners after many years of working in the dark (miner’s nystagmus). In some cases one eye rotates upward and intorts while the other rotates downward, and extorts (see-saw nystagmus as a result of brainstem stroke, chiasmal lesion or multiple sclerosis). In some cases there is a mixture of the two main types; pendular in the primary position and jerk on lateral gaze (mixed nystagmus). The movements of the eyes are usually the same in both eyes (conjugate nystagmus) but in other cases they may be unrelated as a result of internuclear ophthalmoplegia (dissociated nystagmus). Examples of the latter are end-gaze nystagmus, convergence-retraction nystagmus and see-saw nystagmus. Or the eye movements are of equal amplitude and type but in opposite or different directions (disjunctive nystagmus), also commonly associated with internuclear ophthalmoplegia. There are also cases of unknown origin (idiopathic nystagmus).
See ataxia, hereditary spinal; disease, Wernicke’s; foveation period; law, Alexander’s; monochromat; ophthalmoplegia, internuclear; oscillopsia; prisms, yoke; procedure, Faden; reflex, vestibulo-ocular; spasmus nutans; syndrome, Down’s; test, optokinetic nystagmus.
n. blockage syndrome See syndrome, nystagmus blockage.
caloric n. See caloric testing.
congenital n. A motor nystagmus that is present at birth or soon after. It may be inherited as X-linked recessive or autosomal dominant, or induced in the uterus, and results from decreased vision due to corneal opacity, cataract, albinism, aniridia, macular disease or optic atrophy. It is typically a horizontal jerk nystagmus and it may be associated with abnormal head movement and decreases in intensity with convergence. The visual prognosis is reasonably good, but if the head turn is excessive, extraocular muscle surgery may be needed.
See spasmus nutans.
convergence-retraction n. A jerk nystagmus which appears on attempted upward gaze and in which the fast phase brings the two eyes towards each other in a convergent movement with retraction of the globes into the orbit. It may result from a lesion affecting the tectum or dorsal midbrain or a pineal tumour, or form part of Parinaud’s syndrome.
See pinealoma.
gaze-evoked n. An acquired form of horizontal nystagmus characterized by a jerk nystagmus on eccentric gaze with the fast phase towards the direction of gaze. This type of nystagmus is believed to be due to cerebellar or brainstem disease affecting the conjugate gaze centres.
occlusion n. A form of nystagmus occurring when one eye is covered, or which increases in intensity when one eye is covered. The nystagmus is typically of the horizontal, jerk variety, with the fast phase occurring in the direction of the occluded eye.
physiological n. See movements, fixation.
rotary n. A very rare form of nystagmus in which the eyeball makes a movement about the visual axis. It may result from a lesion to the vestibular nerve.
See nystagmus, vestibular.
sensory n. A form of nystagmus thought to be due to an abnormality in the afferent mechanism. It is most often due to inadequate image stimulation of the macula, leading to abnormal development of the ocular fixation reflex. Causes include congenital cataracts, optic nerve hypoplasia, aniridia, albinism, achromatopsia, as well as Leber’s congenital amaurosis.
vestibular n. There are two main types of vestibular nystagmus: Peripheral vestibular nystagmus results from stimulation, injury or disease (e.g. Menière’s disease) of the labyrinth or of the vestibulo-cochlear nerve (VIII). It presents as a jerk, mainly horizontal, nystagmus with a torsional component. It may be accompanied by vertigo, tinnitus and hearing loss. Fixation inhibits the nystagmus. Central vestibular nystagmus results from stimulation, injury, disease of the central vestibular pathways of the brainstem or the cerebellum, or lesion of the vestibular nuclei. It is typically a jerk nystagmus, which can be purely horizontal, vertical or torsional. It is not inhibited by fixation.
nystatin See antifungal agent.





