Myopic Macular Schisis
OCT Features:
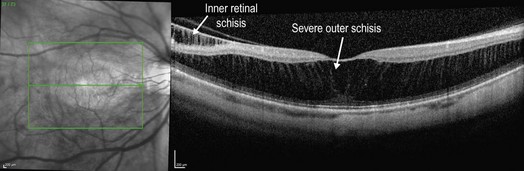
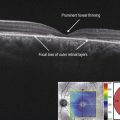
OCT is critical in confirming the diagnosis and following the morphologic changes in myopic schisis. OCT can readily visualize subtle schisis that is often asymptomatic (Fig. 9.3.1), and may be confused for other conditions such as cystoid macular edema. There is a characteristic splitting of the retinal layers that tends to occur in the outer layers, leaving a thicker inner retina split from a thinner outer retina. Joining these two layers are perpendicular strands, which may represent stretched Müller cells. There can be a range of severity in myopic macular schisis, including more moderate (Fig. 9.3.2) and severe (Fig. 9.3.3) changes. The choroid is characteristically thin, as in other instances of high myopia. Other changes include prominent posterior hyaloid, epiretinal membrane, lamellar macular hole or full-thickness macular hole.
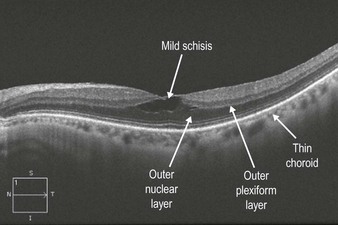
Figure 9.3.1 OCT of mild myopic macular schisis with splitting of the retina at the level of the outer nuclear layer and outer plexiform layer junction. The space created by the schisis is thickest centrally and tapers on each end, which is more apparent in other figures below.
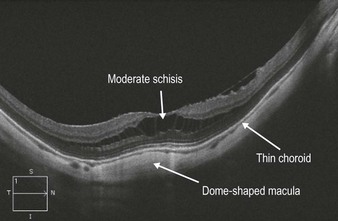
Figure 9.3.2 OCT of moderate myopic macular schisis shows splitting of the retina within the inner portion of the outer nuclear layer. The central area of schisis is thickest with tapering on either side. Three-dimensionally, the schisis space would resemble a flying saucer. Within the schisis cavity, there are perpendicular strands crossing the full length of the cavity, which may represent Müller’s cell footplates. Also note that there is a mild posterior staphyloma and dome-shaped macula present. The choroid is also characteristically thin.