CHAPTER 66 Myocarditis
Definition
Myocarditis refers to focal or diffuse inflammation of the cardiac muscle associated with myocyte damage or necrosis and lymphocyte infiltration as a result of various infectious, immune, or nonimmune insults in the absence of significant acute or chronic ischemia.1–3
Prevalence and Epidemiology
Myocarditis is found in 1% to 10% of postmortem examinations; however, the true prevalence is unknown because of its insidious and variable clinical presentation.1,2 It accounts for 20% of cardiac causes of sudden deaths in military recruits1 and 40% of acute presentations of dilated cardiomyopathy.2 Up to 50% of patients with acquired immunodeficiency syndrome (AIDS) have evidence of myocarditis on biopsy.2
Etiology and Pathophysiology
Infections are a major cause of myocarditis. Viruses, such as coxsackieviruses A and B and other enteroviruses, adenovirus, influenza virus, and Epstein-Barr virus, are the most important causes of myocarditis in the United States.2,4 A wide range of bacteria (Streptococcus, Chlamydia, Neisseria, Borrelia) and parasites (Trypanosoma, Toxoplasma, Trichinella) can also cause myocarditis. Various medications, such as doxorubicin (Adriamycin) and sulfonamides, and toxins, such as cocaine, have also been associated with myocarditis. Large-vessel vasculitis, such as Takayasu arteritis, and autoimmune diseases, such as systemic lupus erythematosus, sarcoidosis, and Wegener granulomatosis, are also important but rare causes of myocarditis.2,4
Manifestations of Disease
Clinical Presentation
The clinical manifestation of myocarditis is variable, ranging from progressive dyspnea and weakness to left ventricular failure to sudden death. Patients may present with influenza-like symptoms, such as fever, fatigue, malaise, and arthralgia.1–3 Arrhythmia is common.4 In addition, chest pain with abnormal electrocardiographic (ECG) recordings and serum troponin elevation in patients with myocarditis can mimic acute myocardial infarction.5 Patients may also present at a late stage with dilated cardiomyopathy.4
Imaging Indications and Algorithm
Imaging plays a pivotal role in the diagnosis of myocarditis. In the past, endomyocardial biopsy was once considered the gold standard for diagnosis of myocarditis; however, it has been shown to have low sensitivity due to sampling error related to the patchy nature of the disease.6 Echocardiography and cardiac MRI should be part of the initial diagnostic evaluation in conjunction with ECG and serum troponin evaluation. More selected biopsy, if needed, may be performed with the MRI result as a guide.5 Coronary computed tomographic angiography (CTA) can be performed in the acute setting to exclude significant coronary arterial stenosis in patients with myocarditis who are presenting with chest pain, raised abnormal cardiac enzymes, and abnormal ECG changes.
Imaging Technique and Findings
Radiography
Chest radiographs may be completely normal in patients with myocarditis, especially acutely (Fig. 66-1). Alternatively, cardiomegaly, interstitial or alveolar pulmonary edema, pleural effusions, and pericardial effusion may be detected as a result of left ventricular failure.2 Less commonly, right ventricular failure may be manifested by right atrial enlargement, prominent azygos vein, and superior vena cava enlargement.
Ultrasonography
Echocardiographic findings of myocarditis are nonspecific, including segmental wall motion abnormalities and increased left ventricular volume.7 During the acute phase, transient left ventricular wall thickening can be observed, probably related to interstitial edema.8,9 The average brightness of the myocardium is also higher in patients with myocarditis than in control patients.10
Computed Tomography
On delayed enhanced images, nodular, patchy, bandlike enhancement of the mid and epicardial layer of the left ventricular wall can be seen in patients with myocarditis (Fig. 66-2).11 In a study of 12 consecutive patients with acute chest pain consistent with myocardial ischemia and normal coronary angiogram, delayed enhanced MDCT performed 5 minutes after injection of contrast material demonstrated the same accuracy as MRI in differentiating between myocardial infarction and myocarditis in the acute phase.12 Similarly, another study also showed good correlation in the extent and location of hyperenhancement at MDCT compared with cardiac MRI in the early phase of suspected acute myocarditis.13
Magnetic Resonance
ECG-triggered segmented cine steady-state free precession imaging may show segmental or global wall motion abnormality, such as hypokinesis or akinesis. Tissue characterization can be performed with ECG-triggered T2-weighted fat-saturated double-inversion recovery turbo spin-echo sequence (or T2 short tau inversion recovery [STIR]) and postcontrast delayed (10 minutes) T1-weighted inversion recovery gradient-echo sequence; the latter is the most important MR pulse sequence in the diagnosis of myocarditis (Fig. 66-3). T2-weighted images may show patchy areas of increased myocardial signal. Postcontrast T1-weighted gradient-echo images typically demonstrate ovoid or nodular, patchy, epicardial and mid-wall delayed hyperenhancement of myocardium in a nonsegmental vascular territory. Focal delayed hyperenhancement may become diffuse later in the disease process but with eventual regression (Fig. 66-4). Resolution of inflammation may be seen in 3 months. Persistent inflammation may lead to myocardial fibrosis and scar formation, resulting in myocardial thinning and dilated cardiomyopathy in some patients.
A large study showed that areas of delayed hyperenhancement are associated with active inflammation defined by histopathologic examination.14 In a study that included 44 patients with myocarditis, inferolateral wall delayed hyperenhancement was a common feature, although other segments were also involved. About two thirds of all lesions were subepicardial in location.15 Another study suggested that the delayed hyperenhancement pattern may be different between myocarditis caused by parvovirus B19 (PVB19) and myocarditis caused by human herpesvirus 6 (HHV6). Patients with PVB19 infection tended to have presentations similar to that of myocardial infarction and had subepicardial delayed hyperenhancement in the lateral wall. Patients with HHV6 or combined PVB19/HHV6 infection presented with new-onset heart failure and had septal delayed hyperenhancement; this group of patients more frequently progressed toward chronic heart failure.16
Delayed hyperenhancement detects irreversible myocardial injury but is unable to differentiate acute from chronic myocarditis.17 The sensitivity may be limited because myocarditis does not always result in irreversible myocardial injury.18
Perfusion cardiac MR imaging can also play a role in differentiating acute myocardial infarction from myocarditis in patients with acute chest pain. A prospective study showed that all the patients with acute myocardial infarction had a segmental early subendocardial defect on first-pass perfusion and corresponding segmental subendocardial or transmural delayed hyperenhancement in a predominantly anteroseptal or inferior vascular distribution. All but one of 24 patients with myocarditis had no early perfusion defect and focal or diffuse nonsegmental non-subendocardial delayed hyperenhancement predominantly in the inferolateral location.19
T2 imaging has also been used to identify acute myocarditis or edema of the myocardium as part of the acute inflammatory process. Because myocarditis usually results in global, instead of focal, high T2 signal abnormality, the signal intensity of the myocardium is compared with that of skeletal muscle.17 Areas of high T2 signal intensity have been shown to correlate with serum markers of acute myocardial injury.20
In the setting of suspected chronic myocarditis, however, a study of 83 patients showed that increased calculated myocardial global relative enhancement on T1-weighted images and edema ratio on T2-weighted images indicating inflammation were common findings. Delayed hyperenhancement, however, had low sensitivity and accuracy.21 It was suggested that if MRI is normal in this setting, endomyocardial biopsy may not be necessary.
Nuclear Medicine/Positron Emission Tomography
Gallium Ga 67, an agent used for evaluation of inflammation, has been used to distinguish acute myocarditis from acute myocardial infarction and to identify myocarditis in children with Kawasaki disease.22,23 The study result is positive when the myocardial uptake is equal to or greater than that in the sternum.
Indium In 111–labeled antimyosin antibodies, which detect myocardial necrosis, have also been used for diagnosis of myocarditis with high sensitivity and negative predictive value.24
Synopsis of Treatment Options
Medical
The first line of treatment is largely supportive, including hemodynamic support in patients with severe left ventricular failure. In the subacute or chronic phase, management of systolic dysfunction includes angiotensin-converting enzyme inhibitor and β-adrenergic blocker. Immunosuppressants such as prednisone, cyclosporine, and azathioprine may be helpful in selected patients, particularly those with myocarditis related to autoimmune disease or giant cell myocarditis. Intravenous immune globulin, interferon alfa, and interferon beta have also been shown to be effective in selected patients in early studies.5
Reporting: Information for the Referring Physician
KEY POINTS
 Myocarditis is focal or diffuse inflammation of the cardiac muscle associated with myocyte damage or necrosis and lymphocyte infiltration.
Myocarditis is focal or diffuse inflammation of the cardiac muscle associated with myocyte damage or necrosis and lymphocyte infiltration. Patchy areas of high signal intensity in the myocardium are demonstrated on precontrast T2-weighted turbo spin-echo sequence (dark blood double-inversion recovery), T2 STIR (dark blood triple-inversion recovery), or HASTE.
Patchy areas of high signal intensity in the myocardium are demonstrated on precontrast T2-weighted turbo spin-echo sequence (dark blood double-inversion recovery), T2 STIR (dark blood triple-inversion recovery), or HASTE. ECG-gated, delayed contrast-enhanced MR typically shows patchy nodular subepicardial or mid-wall hyperenhancement of left ventricular myocardium in a nonvascular distribution.
ECG-gated, delayed contrast-enhanced MR typically shows patchy nodular subepicardial or mid-wall hyperenhancement of left ventricular myocardium in a nonvascular distribution.1 Ellis CR, Di Salvo T. Myocarditis: basic and clinical aspects. Cardiol Rev. 2007;15:170-177.
2 Brady WJ, Ferguson JD, Ullman EA, et al. Myocarditis: emergency department recognition and management. Emerg Med Clin North Am. 2004;22:865-885.
3 Abbara S, Miller SW. Pericardial and myocardial disease. In: Miller SW, editor. Cardiac Imaging: The Requisites. Philadelphia: Elsevier Mosby; 2005:280-282.
4 Burns DK, Kumar V. The heart. In: Kumar V, Cotran RS, Robbins SL, editors. Basic Pathology. Philadelphia: WB Saunders; 1997:329-330.
5 Magnani JW, Dec GW. Myocarditis: current trends in diagnosis and treatment. Circulation. 2006;113:876-890.
6 Hauck AJ, Kearney DL, Edwards WD. Evaluation of postmortem endomyocardial biopsy specimens from 38 patients with lymphocytic myocarditis: implications for role of sampling error. Mayo Clin Proc. 1989;64:1235-1245.
7 Skouri HN, Dec GW, Friedrich MG, et al. Noninvasive imaging in myocarditis. J Am Coll Cardiol. 2006;48:2085-2093.
8 Hiramitsu S, Morimoto S, Kato S, et al. Transient ventricular wall thickening in acute myocarditis: a serial echocardiographic and histopathologic study. Jpn Circ J. 2001;65:863-866.
9 Nakagawa M, Hamaoka K. Myocardial thickening in children with acute myocarditis. Chest. 1993;104:1676-1678.
10 Lieback E, Hardouin I, Meyer R, et al. Clinical value of echocardiographic tissue characterization in the diagnosis of myocarditis. Eur Heart J. 1996;17:135-142.
11 Brooks MA, Sane DC. CT findings in acute myocarditis: 2 cases. J Thorac Imaging. 2007;22:277-279.
12 Boussel L, Gamondes D, Staat P, et al. Acute chest pain with normal coronary angiogram: role of contrast-enhanced multidetector computed tomography in the differential diagnosis between myocarditis and myocardial infarction. J Comput Assist Tomogr. 2008;32:228-232.
13 Dambrin G, Laissy JP, Serfaty JM, et al. Diagnostic value of ECG-gated multidetector computed tomography in the early phase of suspected acute myocarditis. A preliminary comparative study with cardiac MRI. Eur Radiol. 2007;17:331-338.
14 Mahrholdt H, Goedecke C, Wagner A, et al. Cardiovascular magnetic resonance assessment of human myocarditis: a comparison to histology and molecular pathology. Circulation. 2004;109:1250-1258.
15 Bohl S, Wassmuth R, Abdel-Aty H, et al. Delayed enhancement cardiac magnetic resonance imaging reveals typical patterns of myocardial injury in patients with various forms of non-ischemic heart disease. Int J Cardiovasc Imaging. 2008;24:597-607.
16 Mahrholdt H, Wagner A, Deluigi CC, et al. Presentation, patterns of myocardial damage, and clinical course of viral myocarditis. Circulation. 2006;114:1581-1590.
17 Abdel-Aty H, Simonetti O, Friedrich MG. T2-weighted cardiovascular magnetic resonance imaging. J Magn Reson Imaging. 2007;26:452-459.
18 Aretz HT, Billingham ME, Edwards WD, et al. Myocarditis. A histopathologic definition and classification. Am J Cardiovasc Pathol. 1987;1:3-14.
19 Laissy JP, Hyafil F, Feldman LJ, et al. Differentiating acute myocardial infarction from myocarditis: diagnostic value of early- and delayed-perfusion cardiac MR imaging. Radiology. 2005;237:75-82.
20 Abdel-Aty H, Boye P, Zagrosek A, et al. Diagnostic performance of cardiovascular magnetic resonance in patients with suspected acute myocarditis: comparison of different approaches. J Am Coll Cardiol. 2005;45:1815-1822.
21 Gurberlet M, Spors B, Thoma T, et al. Suspected chronic myocarditis at cardiac MR: diagnostic accuracy and association with immunohistologically detected inflammation and viral persistence. Radiology. 2008;246:401-409.
22 Hung MY, Hung MJ, Cheng CW. Use of gallium 67 scintigraphy to differentiate acute myocarditis from acute myocardial infarction. Tex Heart Inst J. 2008;34:305-309.
23 Matsuura H, Ishikita T, Yamamoto S, et al. Gallium-67 myocardial imaging for the detection of myocarditis in the acute phase of Kawasaki disease (mucocutaneous lymph node syndrome): the usefulness of single photon emission computed tomography. Br Heart J. 1987;58:385-392.
24 Narula J, Malhotra A, Yasuda T, et al. Usefulness of antimyosin antibody imaging for the detection of active rheumatic myocarditis. Am J Cardiol. 1999;84:946-950.

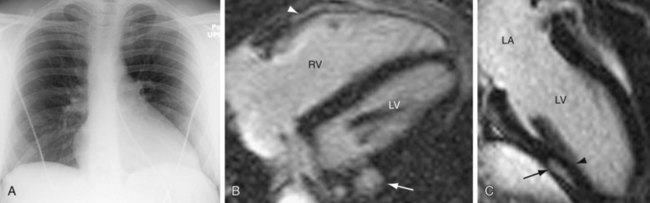
 FIGURE 66-1
FIGURE 66-1
 FIGURE 66-2
FIGURE 66-2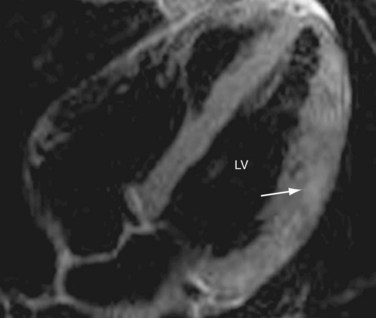
 FIGURE 66-3
FIGURE 66-3
 FIGURE 66-4
FIGURE 66-4




