Chapter 30 Mycobacterial infections
| CLASSIFICATION | OBLIGATE HUMAN PATHOGEN | FACULTATIVE HUMAN PATHOGEN |
|---|---|---|
| Slow Growers | ||
| M. tuberculosis complex | ||
| M. tuberculosis | x | |
| M. bovis | x | |
| M. africanum | x | |
| M. mycoti | x | |
| Photochromogens (Runyon Group 1) Form Yellow-Orange or Rust Pigment with Light |
||
| M. kansasii | x | |
| M. marinum | x | |
| M. simiae complex (M. simiae, M. triplex, M. genavense, M. heidelbergense, and M. lentiflavum) | x | |
| Others include M. intermedium, and M. asiaticum | x | |
| Scotochromogens (Runyon Group 2) Form Light Yellow to Orange Pigment with and without Light |
||
| M. scrofulaceum | x | |
| M. szulgai | x | |
| Others include M. injectum, M. lentiflavum, M. gordonae | x | |
| Nonchromogens (Runyon Group 3) Unable to Form Pigment |
||
| M. avium-intracellulare complex (M. avium, M. intracellulare, and other unidentified species) | x | |
| M. haemophilum | x | |
| M. xenopi | x | |
| M. ulcerans | x | |
| Others include M. celatum, M. genavense, M. gastri, and M. malmoense | x | |
| Rapid Growers (Runyon Group 4) Growth within 7 Days |
||
| M. fortuitum | x | |
| M. abscessus | x | |
| M. chelonei ssp. chelonei, abscessus, unnamed subspecies | x | |
| Others include M. phlei, M. smegmatis, M. fredericksbergense | x | |
| Noncultivable Unable to Cultivate in Media |
||
| M. leprae | x | |
Data from Bhambri S, Bhambri A, Del Rosso JQ: Atypical mycobacterial cutaneous infections, Dermatol Clin 27(1):63–73, 2009.
| CLASSIFICATION | PRIMARY INFECTION (NONIMMUNE HOST) | SECONDARY INFECTION (IMMUNE HOST) |
|---|---|---|
| Exogenous | ||
| Primary inoculation tuberculosis | x | |
| Tuberculosis verrucosa cutis | x | |
| Endogenous | ||
| Scrofuloderma | x | |
| Periorificial tuberculosis | x | |
| Hematogenous/lymphatic | ||
| Lupus vulgaris | x | |
| Acute miliary tuberculosis | x | |
| Gummas | x | |
Data from Semaan R, Traboulsi R, Kanj S: Primary mycobacterium tuberculosis complex cutaneous infection: report of two cases and literature review, Int J Infect Dis 12(5):472–477, 2008.

Figure 30-3. Tuberculosis cutis orificialis. Erythematous eroded plaque of perianal area.
(Courtesy of James E. Fitzpatrick, MD.)
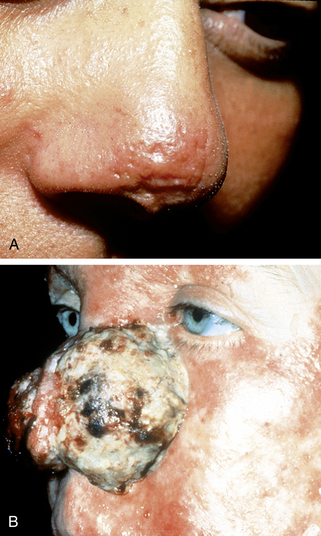
Figure 30-4. Lupus vulgaris. A, Red-brown plaque on nasal tip. B, Lupus vulgaris with squamous cell carcinoma.
Available at http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5211a1.htm. Treatment of Tuberculosis Accessed December 13, 2009.
Table 30-3. First-Line Antituberculous Agents and Major Side Effects
| DRUG | SIDE EFFECT | SPECIAL COMMENT |
|---|---|---|
| Isoniazid | Peripheral neuritis Hepatitis |
From pyridoxine deficiency Occurs with 1%–2%, increased risk with age >35 |
| Rifampin | Hepatitis Orange stain of secretions |
More common when given with isoniazid May permanently stain contact lenses |
| Rifabutin | Neutropenia Hepatitis Orange stain of secretions |
Occurs in HIV patients More common when given with isoniazid May permanently stain contact lenses |
| Rifapentine | Hepatitis Orange stain of secretions |
More common when give with isoniazid May permanently stain contact lenses |
| Pyrazinamide | Hyperuricemia | May precipitate gout |
| Ethambutol | Optic neuritis | Avoid in children under age 13 |
Data available at http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5211a1.htm. Accessed December 13, 2009.
Key Points: Mycobacterial Infections
Cohen JL: Understanding, avoiding, and managing dermal filler complications, Dermatol Surg 34(Suppl 1):S92–S99, 2008.