Chapter 162 Musculoskeletal Pain Syndromes
Clinical Manifestations
Diagnosis and Differential Diagnosis
Subsequent, repeated physical examinations of children with musculoskeletal pain complaints may reveal eventual development and manifestations of rheumatic or other diseases. The need for additional testing should be individualized, depending on the specific symptoms and physical findings. Laboratory screening and/or radiographs should be pursued if there is suspicion of certain underlying disease processes. Possible indicators of a serious, as opposed to a benign, cause of musculoskeletal pain include pain present at rest and relieved by activity, objective evidence of joint swelling on physical examination, stiffness or limited range of motion in joints, bony tenderness, muscle weakness, poor growth and/or weight loss, and constitutional symptoms (e.g., fever, malaise) (Table 162-1). Results of complete blood count and erythrocyte sedimentation rate (ESR) measurement are likely to be abnormal in children whose pain is secondary to a bone or joint infection, SLE, or a malignancy. Bone tumors, fractures, and other focal pathology resulting from infection, malignancy, or trauma can often be indentified through imaging studies, including plain radiographs, MRI, and technetium Tc 99m bone scans.
Table 162-1 POTENTIAL INDICATORS OF BENIGN VS SERIOUS CAUSES OF MUSCULOSKELETAL PAIN
| CLINICAL FINDING | BENIGN CAUSE | SERIOUS CAUSE |
|---|---|---|
| Effects of rest vs activity on pain | Relieved by rest and worsened by activity | Relieved by activity and present at rest |
| Time of day pain occurs | End of the day and nights | Morning* |
| Objective joint swelling | No | Yes |
| Joint characteristics | Hypermobile/normal | Stiffness, limited range of motion |
| Bony tenderness | No | Yes |
| Muscle strength | Normal | Diminished |
| Growth | Normal growth pattern or weight gain | Poor growth and/or weight loss |
| Constitutional symptoms (e.g., fever, malaise) | Fatigue without other constitutional symptoms | Yes |
| Laboratory findings | Normal CBC, ESR, CRP | Abnormal CBC, raised ESR and CRP |
| Radiographic findings | Normal | Effusion, osteopenia, radiolucent metaphyseal lines, joint space loss, bony destruction |
CBC, complete blood count; CRP, C-reactive protein level; ESR, erythrocyte sedimentation rate.
* Cancer pain is often severe and worst at night.
Adapted from Malleson PN, Beauchamp RD: Diagnosing musculoskeletal pain in children, Can Med Assoc J 165:183–188, 2001.
The presence of persistent pain accompanied by psychologic distress, sleep disturbances, and/or functional impairment and in the absence of objective abnormal laboratory or physical findings suggests the diagnosis of a musculoskeletal pain syndrome. All pediatric musculoskeletal pain syndromes share this general constellation of symptoms at presentation. Several more specific pain syndromes routinely seen by pediatric practitioners can be differentiated by anatomic region and associated symptoms. A comprehensive list of pediatric musculoskeletal pain syndromes is provided in Table 162-2; they include growing pains (Chapter 147), fibromyalgia (Chapter 162.1), complex regional pain syndrome (Chapter 162.2), localized pain syndromes, low back pain, and chronic sports-related pain syndromes (e.g., Osgood-Schlatter disease).
Table 162-2 COMMON MUSCULOSKELETAL PAIN SYNDROMES IN CHILDREN BY ANATOMIC REGION
| ANATOMIC REGION | PAIN SYNDROME(S) |
|---|---|
| Shoulder | Impingement syndrome |
| Elbow |
Adapted from Anthony KK, Schanberg LE: Assessment and management of pain syndromes and arthritis pain in children and adolescents, Rheum Dis Clin N Am 33:625–660, 2007.
Growing Pains
Also known as benign nocturnal pains of childhood, growing pains affect 10-20% of children, with a peak age incidence between 4 and 8 yr. The most common cause of recurrent musculoskeletal pain in children, growing pains are intermittent and bilateral, predominantly affecting the anterior thigh and calf but not joints. Children most commonly describe cramping or aching that occurs in the late afternoon or evening. Pain often wakes the child from sleep but resolves quickly with massage or analgesics; pain is never present the following morning (Table 162-3). Physical findings are normal, and gait is not impaired. Growing pains are generally considered a benign, time-limited condition; however, there is increasing evidence suggesting that growing pains represent a pain amplification syndrome. Indeed, growing pains persist in a significant percentage of children, with some children developing other pain syndromes such as abdominal pain and headaches. Recent studies suggest that growing pains are more likely to persist in children with a parent who has a history of a pain syndrome and in children who have lower pain thresholds. Treatment focuses on reassurance, education, and healthy sleep hygiene.
| INCLUSIONS | EXCLUSIONS | |
|---|---|---|
| Nature of pain | Intermittent; some pain-free days and nights | Persistent; increasing intensity |
| Unilateral or bilateral | Bilateral | Unilateral |
| Location of pain | Anterior thigh, calf, posterior knee—in muscles | Join pain |
| Onset of pain | Late afternoon or evening | Pain still present next morning |
| Physical findings | Normal | Swelling, erythema, tenderness; local trauma or infection; reduced joint range of motion; limping |
| Laboratory findings | Normal | Objective evidence of abnormalities, e.g., from erythrocyte sedimentation rate, radiography, bone scanning |
From Evans AM, Scutter SD: Prevalence of “growing pains” in young children, J Pediatr 145:255–258, 2004.
Anthony KK, Schanberg LE. Assessment and management of pain syndromes and arthritis pain in children and adolescents. Rheum Dis Clin N Am. 2007;33:625-660.
Connelly MA, Schanberg LE. Evaluating and managing pediatric musculoskeletal pain in primary care. In: Walco G, Goldschneider K, Berde A, editors. Pain in children: a practical guide for primary care. New York: Humana Press, 2008.
El-Metwally A, Salimen JJ, Auvinen A, et al. Lower limb pain in a preadolescent population: prognosis and risk factors for chronicity—a prospective 1- and 4-year follow-up study. Pediatrics. 2005;116:673-681.
Evans AM. Growing pains: contemporary knowledge and recommended practice. J Foot Ankle Res. 2008;1:4.
Evans AM, Scutter SD. Prevalence of “growing pains” in young children. J Pediatr. 2004;145:255-258.
Kaspiris A, Zafiropoulou C. Growing pains in children: epidemiological analysis in a Mediterranean population. Joint Bone Spine. 2000;76:486-490.
Scharff L, Langan N, Rotter N, et al. Psychological, behavioral, and family characteristics of pediatric patients with chronic pain: a 1-year retrospective study and cluster analysis. Clin J Pain. 2005;21:432-438.
Stahl M, Kautiainen H, El-Metwally A, et al. Non-specific neck pain in schoolchildren: prognosis and risk factors for occurrence and persistence. A 4-year follow-up study. Pain. 2008;137:316-322.
Uziel Y, Chapnick G, Jaber L, et al. Five-year outcome of children with “growing pains”: correlations with pain threshold. J Pediatr. 2010;156:838-840.
Uziel Y, Hashkes PJ. Growing pains in children. Pediatr Rheumatol. 2007;5:5.
Viswanathan V, Khubchandani RP. Joint hypermobility and growing pains in school children. Clin Experiment Rheumatol. 2008;26:962-966.
162.1 Fibromyalgia
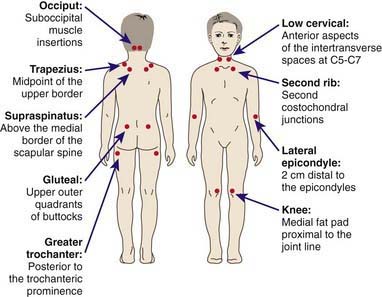
Juvenile primary fibromyalgia syndrome (JPFS) is a common pediatric musculoskeletal pain syndrome. Approximately 25-40% of children with chronic pain syndromes can be diagnosed with JPFS. Although specific diagnostic criteria for JPFS have not been determined, all children and adolescents with JPFS have diffuse musculoskeletal pain in at least 3 areas of the body that persists for at least 3 mo in the absence of an underlying condition. Results of laboratory tests are normal, and physical examination reveals at least 5 well-defined tender points (Fig. 162-1). Children and adolescents with JPFS also present with many associated symptoms, including nonrestorative sleep, fatigue, chronic anxiety or tension, chronic headaches, subjective soft tissue swelling, and pain modulated by physical activity, weather, and anxiety or stress. There is considerable overlap among the symptoms associated with JPFS and the complaints associated with other functional disorders (e.g., irritable bowel disease, migraines, temporomandibular joint disorder, premenstrual syndrome, mood and anxiety disorders, and chronic fatigue syndrome), raising speculation that these disorders may be part of a larger spectrum of related syndromes.
Although the precise cause of JPFS is unknown, there is an emerging understanding that the development and maintenance of JPFS are related both to biologic and psychologic factors. JPFS is an abnormality of pain processing characterized by disordered sleep physiology, enhanced pain perception with abnormal levels of substance P in cerebrospinal fluid, disordered mood, and dysregulation of hypothalamic-pituitary-adrenal and other neuroendocrine axes resulting in lower tender point pain thresholds and increased pain sensitivity. Children and adolescents with fibromyalgia also often find themselves in a vicious cycle of pain, whereby symptoms build on one another and contribute to the onset and maintenance of new symptoms (Fig. 162-2).

Figure 162-2 Cycle promoting juvenile primary fibromyalgia syndrome symptoms and their maintenance.
(Adapted from Anthony KK, Schanberg LE: Juvenile primary fibromyalgia syndrome, Curr Rheumatol Rep 3:162–171, 2001.)
American Pain Society. Guidelines for the management of fibromyalgia syndrome pain in adults and children. Glenview, IL: American Pain Society; 2005.
Degotardi PJ, Klass ES, Rosenberg BS, et al. Development and evaluation of a cognitive-behavioral intervention for juvenile fibromyalgia. J Pediatr Psychol. 2006;31:714-723.
Häuser W, Bernardy K, Üçeyler N, et al. Treatment of fibromyalgia syndrome with antidepressants. JAMA. 2009;301:198-212.
Kashikar-Zuck S, Parkins IS, Graham TB, et al. Anxiety, mood, and behavioral disorders among pediatric patients with juvenile fibromyalgia syndrome. Clin J Pain. 2008;24:620-626.
Langhorst J, Klose P, Musial F, et al. Efficacy of acupuncture in fibromyalgia syndrome—a systematic review with a meta-analysis of controlled clinical trials. Rheumatology. 2010;49:778-788.
2009 Milnacipran (Savella) for fibromyalgia. Med Lett. 2009;51:45-46.
Swain NF, Kashikar-Zuck S, Graham TB, et al. Tender point assessment in juvenile primary fibromyalgia syndrome. Arthritis Rheum. 2005;53:785-787.
Wang C, Schmid CH, Rones R, et al. A randomized trial of tai chi for fibromyalgia. N Engl J Med. 2010;363(8):743-754.
162.2 Complex Regional Pain Syndrome
Complex regional pain syndrome (CRPS) is characterized by ongoing burning limb pain that is subsequent to an injury, immobilization, or another noxious event affecting the extremity. CRPS1, formerly called reflex sympathetic dystrophy, has no evidence of nerve injury, whereas CRPS2, formerly called causalgia, follows a prior nerve injury. Key associated features are pain disproportionate to the inciting event, persisting allodynia (a heightened pain response to normally non-noxious stimuli), hyperalgesia (exaggerated pain reactivity to noxious stimuli), swelling of distal extremities, and indicators of autonomic dysfunction (i.e., cyanosis, mottling, and hyperhidrosis) (Table 162-4).
Table 162-4 DIAGNOSTIC CRITERIA FOR COMPLEX REGIONAL PAIN SYNDROME
| A diagnosis of complex regional pain syndrome (CRPS) requires regional pain, sensory symptoms, plus two neuropathic pain descriptors and two physical signs of autonomic dysfunction: |
| NEUROPATHIC DESCRIPTORS |
Data from Wilder RT, Berde CB, Wolohan, M, et al: Reflex sympathetic dystrophy in children: clinical characteristics and follow-up of seventy patients, J Bone Joint Surg Am 74:910–919, 1992.
Berde C, Lebel A. Complex regional pain syndromes in children and adolescents. Anesthesiology. 2005;102:252-255.
Higashimoto T, Baldwin EE, Gold JI, et al. Reflex sympathetic dystrophy: complex regional pain syndrome type I in children with mitochondrial disease and maternal inheritance. Arch Dis Child. 2008;93:390-397.
Leone V, Tornese G, Zerial M, et al. Joint hypermobility and its relationship to musculoskeletal pain in schoolchildren: a cross-sectional study. Arch Dis Child. 2009;94:627-632.
Ross J, Grahame R. Joint hypermobility syndrome. BMJ. 2011;342:275-277.
Wilder RT. Management of pediatric patients with complex regional pain syndrome. Clin J Pain. 2006;22:443-448.
162.3 Erythromelalgia
Children with erythromelalgia experience episodes of intense pain, erythema, and heat in their hands and feet (Fig. 162-3) and less commonly in their face, ears, or knees. Symptoms may be triggered by exercise and exposure to heat, and they last for hours and occasionally for days. Although most cases are sporadic, an autosomal dominant hereditary form results from a mutation in the gene SCN9A on chromosome 2q31-32, which is responsible for sodium channel function in dorsal root ganglia. Erythromelalgia is also associated with an array of disorders, including myeloproliferative diseases, peripheral neuropathy, frostbite, hypertension, and rheumatic disease. Treatment includes avoidance of heat exposure as well as other precipitating situations and the utilization of cooling techniques that do not cause tissue damage during attacks. Nonsteroidal anti-inflammatory drugs, narcotics, anesthetic agents, anticonvulsants, and antidepressants as well as biofeedback and hypnosis may be useful in managing pain. Drugs acting on the vascular system (aspirin, sodium nitroprusside, magnesium, misoprostol) may also be effective.