chapter 34 Musculoskeletal medicine
INTRODUCTION AND OVERVIEW
Musculoskeletal medicine (MSM) is that branch of medicine dealing with the conservative management of disorders of the musculoskeletal system, including the muscles, aponeuroses, joints and bones of the axial and appendicular skeletons, and those parts of the nervous system associated with them. These disorders represent the most common cause of disability in most countries across all age groups1 and are the third most common reason for presentation to general practice.2 The direct and indirect costs of this burden are in the $15 billions per annum.3
Yet, paradoxically, undergraduate and postgraduate education in MSM is at best elementary. The need for MSM training in medical schools and hospitals has been well established.4 Currently in Australia there is no public MSM outpatients department (OPD) hospital clinic, which differs from our European and American colleagues, who have vibrant systems in place. For instance, osteopathy and musculoskeletal medicine special-interest doctors are recognised in the United Kingdom, musculoskeletal physicians are recognised in Europe and the United States has osteopathic MDs. Historically in Australia it has been left to the allied healthcare professionals and alternative healthcare practitioners to absorb much of the demand for musculoskeletal (MS) management. The medical profession has been slow to embrace MSM, but has a vital role to play. The optimal management of MSM conditions epitomises the need for an integrated approach from practitioners knowledgeable in the biopsychosocial approach to management. General practitioners with postgraduate MS training can work collaboratively with other healthcare providers to minimise pain and optimise function for patients.
One of the most common MS disorders seen by healthcare practitioners in Australia is spinal pain. Persistent back pain is by far the most common reason for chronic MS patient encounter in Australian general practice, followed by knee, shoulder and neck.5
LOW BACK PAIN
DEFINITIONS
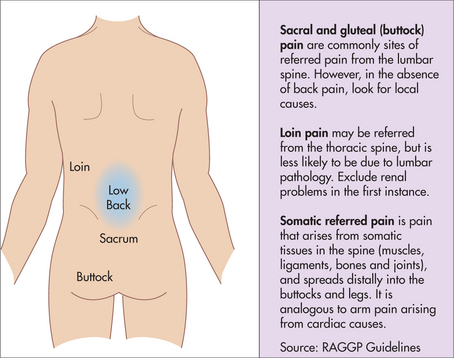
| Somatic referred pain | Radicular pain |
|---|---|
| Due to spread of pain from deep spinal tissues (including muscles) | Due to chemical or mechanical irritation of nerves |
| Back pain worse than leg pain, which may be bilateral | Unilateral leg pain worse than back pain |
| Pain concentrates proximally in buttock and thigh, but may spread below knee | Pain concentrates distally, running into the lower limb, usually extending below the knee |
| Deep, dull aching, expanding pressure-like quality | Sharp, shooting, electric quality, often deep and superficial |
| Vague location, varies over time, ill-defined distribution | Pain runs along defined narrow band in dermatome distribution |
| Poorly defined paraesthesia may be present | Numbness and paraesthesia in dermatomal distribution |
| Normal reflexes and power (if abnormal, further assessment is needed) | Reflexes may be reduced or absent; motor weakness may be present |
EPIDEMIOLOGY
The lifetime prevalence of acute LBP is about 70%,16 with the cumulative lifetime prevalence of episodes lasting more than 2 weeks being 14%.17 In Australia, back complaint is the sixth most common reason for presentation to a general practitioner.2
Data on the natural history of LBP are variable but instructive when closely analysed. A commonly quoted statement is that, with treatment, ‘90% of patients recover within 2 months’.18 This may be true when follow-up is only for 4 weeks.18 More-rigorous studies with 12-month follow-up reveal a different picture.19,20 Around 80% of patients remain disabled to some extent at 12 months, with 10–15% highly disabled. These studies paint a picture of recovery followed by relapse. In general, a patient’s status at 2 months post presentation reflects their status at 12 months.
An Australian study of acute LBP patients without a compensation claim managed with evidence-based guidelines revealed that 70% can expect to recover and stay recovered at 12 months, with a low risk of recurrence.21
HISTORY
EXAMINATION
Although physical examination of LBP patients will rarely allow a patho-anatomic diagnosis to be made, it remains an extremely valuable tool. Its strength lies in the opportunities it opens (Box 34.4). A confidently performed physical examination in association with meaningful dialogue is an important step in the overall management.
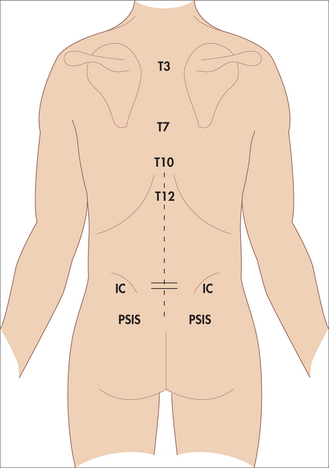
Following the orthopaedic model of ‘look, move and feel’ is the standard approach. Initial inspection allows a record of asymmetry, pain behaviour, gait and skin lesions. A knowledge of surface landmarks (Fig 34.7) adds more meaning to the descriptions. The physician should be alert for pain behaviour from the patient and its interpretation. Importantly, pain behaviour needs to be recognised as the patient’s way of communicating distress. Overt or exaggerated pain behaviour is not a sign of malingering but, rather, a signal for the doctor to explore pain management issues in more depth. This would include psychosocial factors as well as biological.
The patient can be moved in all six planes—flexion, extension, lateral flexion left and right, and rotation left and right. Rotation is best performed sitting, to stabilise the pelvis. While the patient is seated, straight leg raising (SLR) and slump testing may be performed (Fig 34.8). With the patient in the supine position, SLR can be assessed as well as leg length. Hip range of movement (ROM) can be assessed, noting that if back pain is reproduced, this is most likely to be from the effects on lumbar/pelvic structures than the hip joint (groin/anterolateral thigh pain). In the prone position, hip extension and hip rotation can be assessed.
FIGURE 34.8 Slump test. The patient sits on the edge of the couch, then in a stepwise fashion, increased stretch is introduced as follows: i) the patient slumps forward, ii) then flexes the neck, iii) then straightens the leg, iv) then dorsiflexes the foot. Purportedly, if any back or leg pain reproduced so far is eased when the neck is then extended, and/or the ankle plantar flexed, then neuromeningeal irritation, rather than hamstring pain, is invoked (adopted from Kenna & Murtagh23).
Special tests of spinal dysfunction have been described for the lumbar and pelvic region, including many labelled as sacroiliac tests. A combination of tests shows best utility regarding sacro-iliac joints (SIJ) dysfunction.24
INVESTIGATION
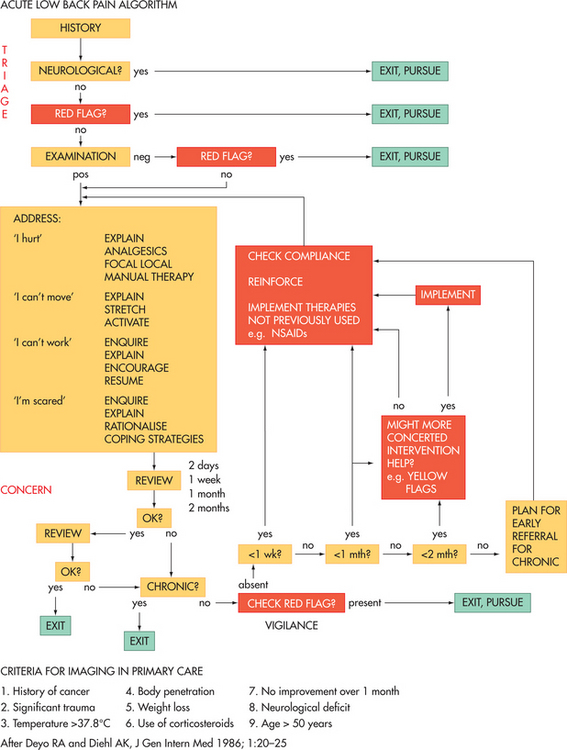
Careful thought is needed before investigating a patient. Concern regarding increasing levels of radiological intervention, especially CT scanning, has become topical.25,26 The risk of exposure to significant ionising radiation, for questionable clinical benefit along with wasting of limited healthcare resources, should be of concern to the healthcare practitioner and consumer alike. By asking: ‘How will this investigation influence my management, what are the chances of a significant finding and will this test detect it?’, unnecessary tests are likely to be avoided.
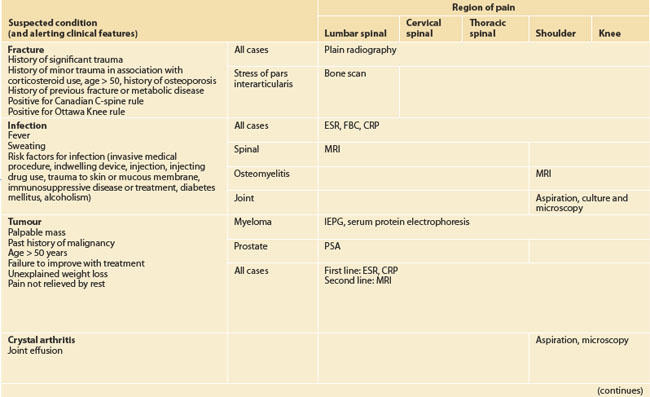
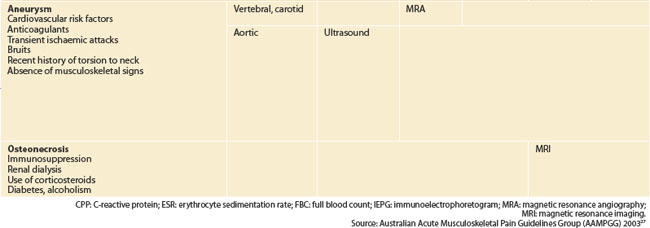
Red flag conditions and their appropriate investigations are shown in Table 34.2. Plain films have a reasonable pick-up rate (Table 34.3) but will miss early disease. CT scans have no role in the investigation of somatic low back pain, except in confirmation of pathology indicated by other investigations or the history/examination. MRI scan is the investigation of choice for red flag conditions of the spine and gives the best information about the status of the intervertebral disc (i.e. presence or absence of modic lesions and high-intensity zones).
TABLE 34.3 Sensitivity* and specificity** of plain films in the evaluation of some pathological causes of back pain
| Condition | Sensitivity | Specificity |
|---|---|---|
| Malignancy | 70% | 90% |
| Osteomyelitis | 80–90% | 70–90% |
| Spondylitis | 50% | 90% |
** 100% minus false positive %
Source: Mazanec 199128
Providing the patient with a proper explanation of the role of the investigation is paramount. This is especially so with radiological investigation, where reported abnormalities are, in most cases, not significant (Table 34.4). However, patients risk being alarmed by being referred for unnecessary investigations and misinterpretation of asymptomatic anatomical abnormalities.29
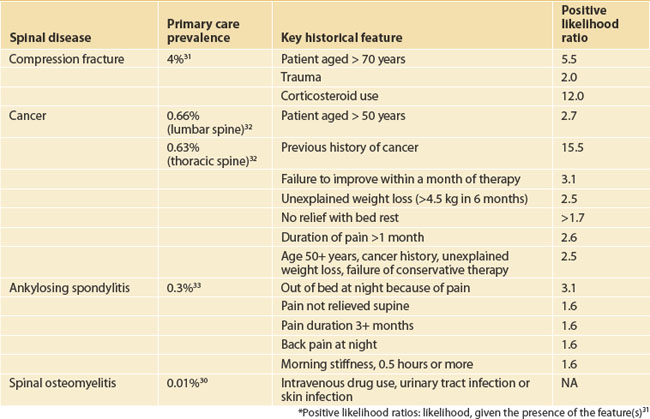
TABLE 34.4 Spinal disease linked to back pain: prevalence in a primary care population,30–33 key historical features and their respective positive likelihood ratios31
DIAGNOSIS
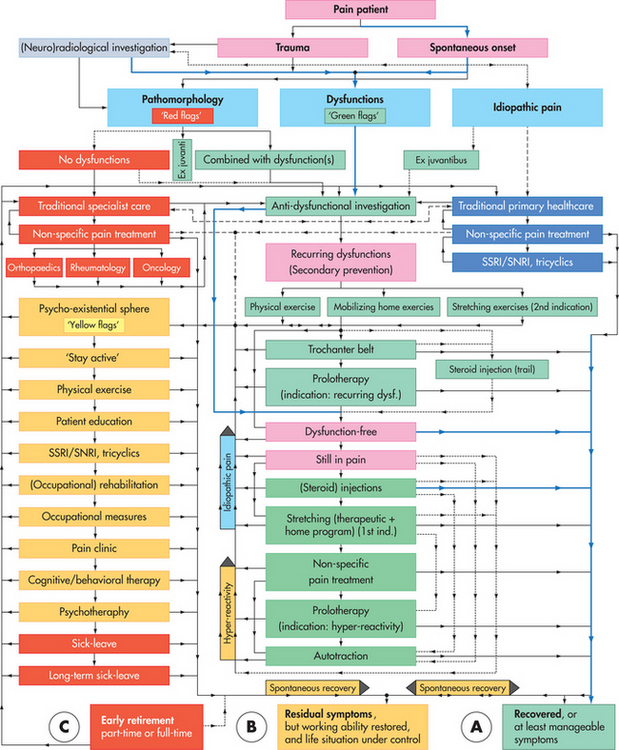
A specific patho-anatomic diagnosis will not be forthcoming for the overwhelming majority of LBP patients. In essence, the initial consultation(s) are primarily to exclude red flag diagnosis and estimate the influence of yellow flags on prognosis. The probability diagnosis will be somatic LBP, and in the acute pain situation no further clarification is necessary. Evidence-informed practice has no value from any further subclassification, even though this is common practice in primary care.34 Primary practitioners can reasonably use a benign label (ligament or muscle strain) to help reassure their patients that they have a good prognosis.
In the case of persisting pain, precision diagnosis may be sought. Two structures can be relatively easily blocked by guided anaesthetic blocks: the zygapophyseal joints and the sacroiliac joints. Both have validated protocols that must be followed correctly for accurate diagnosis.35,36 Radiofrequency neurotomy may be used as a treatment if the blocks are positive.37,38 The intervertebral disc cannot be specifically blocked, but provocative discography has been used to identify a painful disc. The role of discography has been controversial,39 but it has been used primarily to select patients for fusion surgery.
MANAGEMENT
From the individual patient’s point of view, management must address four key concerns:40
The research data are quite clear on the importance of educating low-back-pain sufferers about the nature of their problem, assuring them of the generally good prognosis and encouraging them to stay as active as possible. What is less clear is the best overall combination of other treatments, such as supervised therapeutic exercise, manual therapy, injections, behavioural therapy, workplace intervention a and myriad other interventions. Few studies have tested combinations of treatments or integrative management, most studies comparing monotherapies against standard/minimal care or another monotherapy. The Australian National Musculoskeletal Medicine Initiative21 and Blomberg’s pragmatic trials41–44 are significant trials that have compared algorithms involving multiple treatments versus standard care. They are informative for an approach to the four concerns above.
Initial presentation
BOX 34.5 Pain management options
BOX 34.6 Recommendations for activity and exercise
COMPLEMENTARY THERAPIES
Acupuncture
For low back pain
A 2005 Cochrane review50 looked at acupuncture for non-specific low back pain and dry-needling for myofascial pain in the lower back. Thirty-five trials were included in the review. The authors concluded that acupuncture relieves pain and improves function in patients with chronic low back pain, compared with no treatment or sham treatment, and this effect was sustained at short-term, but not long-term, follow-up. Acupuncture as an adjunct to conventional treatments is more effective than conventional treatments alone, although the effects are small. Dry-needling can also be a useful adjunct. However, neither acupuncture nor dry-needling are more effective than other treatments, conventional or ‘alternative’. These findings were confirmed by an independent 2005 meta-analysis of acupuncture for low back pain, which concluded that acupuncture provides short-term pain relief of chronic low back pain.51 There was insufficient evidence on acupuncture for acute low back pain.
For neck pain
A 2006 Cochrane review52 found 10 trials on acupuncture for chronic neck pain, and none for acute or sub-acute neck pain. The authors concluded that there was moderate evidence that acupuncture is more effective than sham treatments in relieving pain both immediately post-treatment and at short-term follow-up. Limited evidence suggests that acupuncture is more effective than massage in the short term. There is moderate evidence that acupuncture is more effective than waitlist control for neck pain with radicular symptoms, at short-term follow-up.
For lateral elbow pain
A 2002 Cochrane review53 found four small trials of acupuncture for lateral elbow pain of more than 3 weeks duration, and not due to trauma or systemic inflammation. Two trials, with a total of 130 patients, compared needle acupuncture with sham acupuncture. Acupuncture was found to result in greater relief of pain than sham acupuncture (mean difference 18.8 hours), and was more likely to result in 50% more reduction in pain and overall improvement after 10 treatments. However, these changes were not sustained at medium/long-term follow-up (3–12 months).
Since then, two more trials have been published. Tsui and Leung54 in a small uncontrolled trial (n = 20) found that electroacupuncture was superior to manual acupuncture after 2 weeks, and Fink and colleagues55 found in a small trial (n = 45) that both true and sham acupuncture resulted in a decrease in pain and improvement in function after 2 weeks, the difference being significantly greater in the true acupuncture group. At 2-month follow-up the true acupuncture group maintained the improvement in function but pain scores had returned to baseline.
Herbal treatments
Anti-inflammatory herbs used in musculoskeletal applications:
INITIAL FOLLOW-UP
FURTHER FOLLOW-UP
Management of chronic persistent low back pain is beyond the scope of this chapter.
SPONDYLOLYSIS/LISTHESIS
EPIDEMIOLOGY
The fetal incidence of spondylolysis has conclusively been shown to be zero. It is only on walking that we see spondylolysis occurring. In a study of 32,600 asymptomatic adults, the prevalence of a pars defect was 7.2%.63 The prevalence has not been shown to be any different in patients suffering from low back pain. There is no significant change in that rate from age 20 to age 80. It is therefore the teenage years that we must be vigilant about, as practitioners.
Most spondylolysis occurs at L5 (85–95%), with most of the rest occurring at the neighbouring L4 (5–15%). There is a strong association with spina bifida occulta.64 The young athletic populations are at most risk, with gymnasts, cricketers (fast bowlers), footballers, rowers, weight lifters and throwing track and field athletes at highest risk of symptomatic spondylolysis.
PATHOPHYSIOLOGY AND NATURAL HISTORY
In a 45-year follow-up evaluation of first-grade children with a spondylolytic defect, whether symptomatic or not, subjects with bilateral pars defect had a virtually identical course to that of the general population in terms of disability and pain.65 There appeared to be a marked slowing of slip progression with time, and no subject had reached a 40% slip. Importantly, the authors agreed that there was no justification for advising children and adolescents with spondylolysis and low-grade spondylolisthesis not to participate in sport.
A 7–11-year follow-up of symptomatic young athletes with early-detected spondylolysis recorded similar reassuring findings.66 Most young athletes conservatively treated will have good functional outcomes at 11-year follow-up. If the pars defect is unilateral, there is a good chance of bony union, but it can take over 3 months.
CLINICAL FEATURES
Most spondylolysis and spondylolisthesis will be asymptomatic. In children, only 13% of individuals with a pars defect have symptoms, and then they usually occur at growth spurts.67
IMAGING
To avoid unnecessary radiation, careful thought must be given to ordering radiology. The first rule is not to rush into radiology at the first visit, if there has been no trial of conservative therapy. Most patients suspected of stress fracture are negative to bone scan and X-ray.68 If, at the 4–6-week mark, there are no signs of the patient settling, then the first step would be a simple lateral of the spine. If spondylolisthesis is present, then no further radiology is necessary. Once there is a slip present, a bone scan is unnecessary as it means there is no possible chance of bony repair of a spondylolysis. The presence of spondylolisthesis does not imply that it is the cause of the back pain, but it does rule out any need for bracing the spine.
MANAGEMENT
There are no high-quality controlled trials on treatment for spondylolysis. Most studies are uncontrolled case series involving the use of supervised exercise programs, braces and analgesia. Two studies have shown that specific exercise interventions, alone or in combination with other treatments, have a positive effect on low back pain due to spondylolysis and spondylolisthesis; however, the type of exercise was different in both studies.52
Australian Association of Musculoskeletal Medicine. http://www.musmed.com.
Australasian Faculty of Musculoskeletal Medicine. http://www.afmm.com.au.
Australian Family Physician—back pain (June 2004 issue). http://www.racgp.org.au/afp/200406/20040601masters.pdf.
Australian Family Physician—musculoskeletal medicine (June 2007 issue). http://www.racgp.org.au/afp/200706.
Australasian Musculoskeletal Medicine—journal published biannually by AAMM. http://www.musmed.com/journal.html.
1 Giles LC, Cameron ID, Crotty M. Disability in older Australians: projections for 2006–2031. Med J Aust. 2003;179:130-133.
2 Australian Institute of Health and Welfare. General practice activity in Australia 2006–07. Online. Available: http://www.aihw.gov.au/publications/gep/gpaa06-07/.
3 Access Economics. The prevalence, cost and disease burden of arthritis in Australia, Canberra: Arthritis Foundation of Australia, 2001.
4 Woolf AD, Walsh NE, Akesson K. Global care recommendations for musculoskeletal undergraduate curriculum. Ann Rheum Dis. 2004;63:517-524.
5 Charles J, Britt H, Fahridin S. Chronic musculoskeletal problems managed in general practice. Aust Fam Physician. 2007;36:392-393.
6 Merskey H, Bogduk N, editors. Classification of chronic pain. Seattle, WA: IASP Press, 1994.
7 Weddell G, Harpman JA. The neurohistological basis for the sensation of pain provoked from deep fascia, tendon, and periosteum. J Neurol Psychiatry. 1940;3:319-328.
8 Inman VT, Saunders JBD. Referred pain from skeletal structure. J Nerv Ment Dis. 1944;99:660-667.
9 Kellgren JH. On the distribution of pain arising from deep somatic structures with charts of segmental pain areas. Clin Sci. 1939;4:35-46.
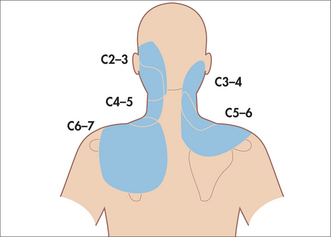
10 Dwyer A, Aprill C, Bogduk N. Cervical zygapophyseal joint pain patterns I: a study in normal volunteers. Spine. 1990;15:453-457.
11 Aprill C, Dwyer A, Bogduk N. Cervical zygapophyseal joint pain patterns II: a clinical evaluation. Spine. 1990;15:458-461.
12 Fukui S, Ohseto K, Shiotani M, et al. Referred pain distribution of the cervical zygapophyseal joints and cervical dorsal rami. Pain. 1996;68:79-83.
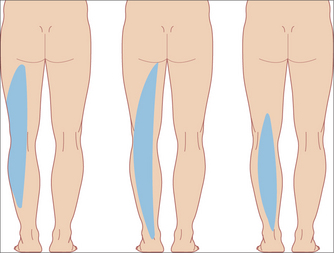
13 McCall IW, Park WM, O’Brien JP. Induced pain referred from posterior lumbar elements in normal subjects. Spine. 1979;4:441-446.
14 Fukui S, Ohseto K, Shiotani M, et al. Distribution of referred pain from the lumbar zygapophyseal joints and dorsal rami. Clin J. 1997;13:303-307.
15 Deyo RA, Rainville J, Kent DL. What can the history and physical examination tell us about low back pain? JAMA. 1992;268:760-765.
16 Bogduk N. Mechanisms of musculoskeletal pain. Australasian Musculoskeletal Medicine. 2006;11:6-18.
17 Deyo RA, Tsui-Wu YJ. Descriptive epidemiology of low back pain and its related medical care in the United States. Spine. 1987;12:264-268.
18 Coste J, Delecoeuillerie G, Cohen de Lara A, et al. Clinical course and prognostic factors in acute low back pain: an inception cohort study in primary care setting. Br Med J. 1994;308:577-580.
19 Von Korff M, Deyo RA, Cherkin D, et al. Back pain in primary care: outcomes at 1 year. Spine. 1993;18:855-862.
20 Croft PR, Macfarlane GJ, Papageorgiou AC, et al. Outcome of low back pain in general practice: a prospective study. Br Med J. 1998;316:1356-1359.
21 McGuirk B, King W, Govind J, et al. The safety, efficacy and cost-effectiveness of evidence-based guidelines for the management of acute low back pain in primary care. Spine. 2001;26:2615-2622.
22 Bogduk N. National musculoskeletal medicine initiative. Evidence-based clinical practice guidelines for the management of acute low back pain. CD-ROM Medseed Compass; 2003.
23 Kenna C, Murtagh J. Back pain and spinal manipulation. Sydney: Elsevier, 1997.
24 Hancock MJ, Maher CG, Latimer J, et al. Systematic review of tests to identify the disc, SIJ or facet joint as the source of low back pain. Eur Spine J. 2007;16(10):1539-1550.
25 Mendelson R, Conor P. Towards the appropriate use of diagnostic imaging. Med J Aust. 2007;187:5-6.
26 Birnbaum S. CT scanning: too much of a good thing. Br Med J. 2007;334:1006.
27 Australian Acute Musculoskeletal Pain Guidelines Group. Appendix C; 2003. Online. Available: http://www.nhmrc.gov.au.
28 Mazanec DJ. Low back pain syndromes. In: Panzer RJ, Black ER, Griner PF, editors. Diagnostic strategies for common medical problems. American College of Physicians, 1991.
29 Borenstein DG, O’Mara JW, Boden SD, et al. The value of magnetic resonance imaging of the lumbar spine to predict low-back pain in asymptomatic subjects. J Bone Joint Surg. 2001;83:1306-1311.
30 Liang M, Komaroff AL. Roentgenograms in primary care patients with acute low back pain: a cost effectiveness analysis. Arch Intern Med. 1982;142:1108-1112.
31 Deyo RA, Rainville J, Kent DL. What can history and physical examination tell us about low back pain? JAMA. 1992;268:760-765.
32 Deyo RA, Diehl AK. Cancer as a cause of back pain: Frequency, clinical presentation, and diagnostic strategies. J Gen Intern Med. 1988;3:230-238.
33 Carter ET, McKenna CH, Brian DD, et al. Epidemiology of ankylosing spondylitis in Rochester, Minnesota, 1935–1973. Arthritis Rheum. 1979;22:365-370.
34 Kent P, Keating JL. Classification in nonspecific low back pain: what methods do primary care clinicians currently use? Spine. 2005;30(12):1433-1440.
35 Bogduk N. International Spinal Injection Society guidelines for the performance of spinal injection procedures. Part1: Zygapophyseal joint blocks. Clin J Pain. 1997;13:285-302.
36 Schwarzer AC, April CN, Bogduk N. The sacroiliac joint in chronic low back pain. Spine. 1995;20:31-37.
37 Binder D, Nampiaparampil D. The provocative lumbar facet joint. Curr Rev Musculoskelet Med. 2009;2(1):15-24.
38 Mulner S. Review article: radiofrequency neurotomy for the treatment of sacroiliac joint syndrome. Curr Rev Musculoskelet Med. 2009;2(1):10-14.
39 Carragee EJ, Alamin TF. Discography: a review. The Spine Journal. 2001;1:364-372.
40 Watson PN. The MSM Quartet. Letter to the editor. Australasian Musculoskeletal Medicine. 1999;2:8-9.
41 Blomberg S. A pragmatic approach to low back pain including manual therapy and steroid injections. A multicenter study in primary health care. 1993; PhD Thesis, Uppsala University, Sweden.
42 Blomberg S, Hallin G, Grann K, et al. Manual therapy with steroid injections—a new approach to treatment of low back pain. A controlled multicenter trial with an evaluation by orthopedic surgeons. Spine. 1994;19(5):569-577.
43 Grunnesjo MI, Bogefeldt JP, Svardsudd KF, et al. A randomized controlled clinical trial of stay-active care versus manual therapy in addition to stay-active care: functional variables and pain. J Manipulative Physiol Ther. 2004;27(7):431-441.
44 Blomberg S. A pragmatic strategy for low back pain—an integrated multimodal programme based on antidysfunctional medicine. In: Hutson M, editor. Textbook of musculoskeletal medicine. Oxford University Press; 2005:1-20.
45 Hagen KB, Hilde G, Jamtvedt G, et al. Bed rest for acute low-back pain and sciatica. Cochrane Database Syst Rev. 2004;4:CD001254.
46 Kendall NAS, Linton SJ, Main CJ. Guide to assessing psychosocial yellow flags in acute low back pain: risk factors for long-term disability and work loss. Wellington, New Zealand: Accident Rehabilitation and Compensation Insurance Corporation of New Zealand and the National Health Committee; 1997. Online. Available: http://www.nhc.govt.nz.
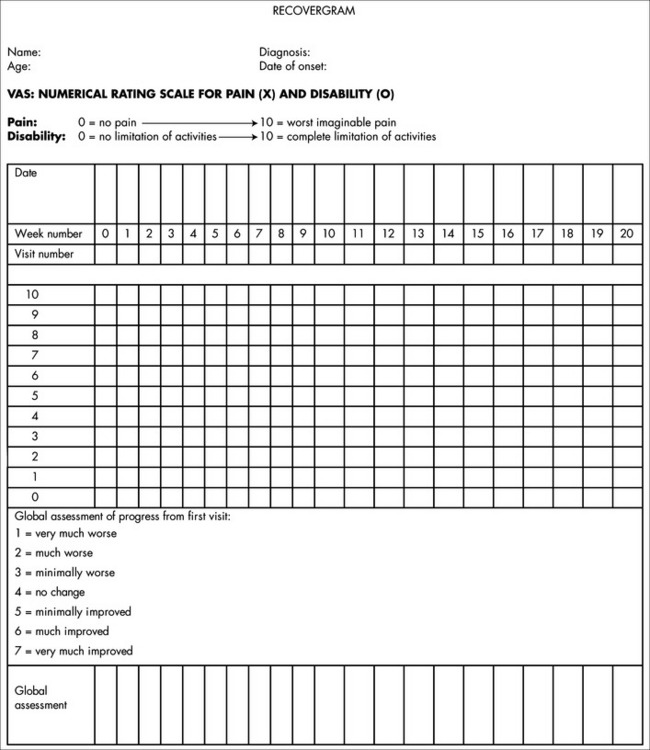
47 Watson P. The recovergram. Australasian Musculoskeletal Medicine. 2000;5(2):24-28.
48 Hammill R, Beazell J, Hart J. Neuromuscular consequences of low back pain and core dysfunction. Clin Sports Med. 2008;27:449-462.
49 Little P, Lewith G, Webley F, et al. Randomised controlled trial of Alexander technique lessons, exercise, and massage (ATEAM) for chronic and recurrent back pain. Br Med J. 2008;337:a884.
50 Furlan AD, van Tulder MW, Cherkin DC, et al. Acupuncture and dry-needling for low back pain. Cochrane Database Syst Rev. 2005. CD001351.
51 Mainheimer E, White A, Berman B, et al. Meta-analysis: acupuncture for low back pain. Ann Intern Med. 2005;142:651-663.
52 Trinh KV, Graham N, Gross AR, et al. Acupuncture for neck disorders. Cochrane Database Syst Rev. 2006;3:CD004870.
53 Green S, Buchbiner R, Barnsley L, et al. Acupuncture for lateral elbow pain. Cochrane Database Syst Rev. 2002. CD003527.
54 Tsui P, Leung MCP. Comparison of the effectiveness between manual acupuncture and electro-acupuncture on patients with tennis elbow. Acupunct Electrother Res. 2002;27:107-117.
55 Fink M, Wolkenstein E, Lunnemann M, et al. Chronic epicondylitis: effects of real and sham acupuncture treatment: a randomised controlled patient- and examiner-blinded long-term trial. Forsch Komplementarmed. 2002;9:210-215.
56 Laudahn D, Walper A. Efficacy and tolerance of Harpagyphytum extract LI 174 in patients with chronic non-radicular back pain. Phytother Res. 2001;15(7):621-624.
57 Chrubasik S, Junck H, Breitschwerdt H, et al. Effectiveness of Harpagophytum extract WS 1531 in the treatment of exacerbation of low back pain: a randomized, placebo-controlled, double-blind study. Eur J Anaesthesiol. 1999;16(2):118-129.
58 European Scientific Co-operative on Phytomedicine (ESCOP). 2nd edn. Stuttgart: Thieme; 2003.
59 Chrubasik S, Model A, Black, et al. A randomised double-blind pilot study comparing Doloteffin® and Vioxx® in the treatment of low back pain. Rheumatology. 2003;42(1):141-148.
60 Gagnier JJ, van Tulder M, Berman B, et al. Herbal medicine for low back pain. Cochrane Database Syst Rev. 2006;2:CD004504.
61 Chrubasik S, Eisenberg E, Balan E, et al. Treatment of low back pain exacerbations with willowbark extract: a randomised double-blind study. Am J Med. 2000;109(1):9-14.
62 Jayaprakasam B, Nair NG. Cyclooxygenase 2 enzyme inhibitory withanolides from Withania somnifera leaves. Tetrahedron. 2003;59(6):125-132.
63 Moreton RD. Spondylolysis. JAMA. 1966;195:671-674.
64 Standaert CJ, Herring SA. Spondylosis: a critical review. Br J Sports Med. 2000;34(6):415-422.
65 Beutler WJ, Fredrickson BE, Murtland A, et al. The natural history of spondylolysis. Spine. 2003;28:1027-1035.
66 Miller SF, Congeni J, Swanson K. Long-term functional and anatomical follow-up of early detected spondylolysis in young athletes. Am J Sports Med. 2004;32:928-933.
67 Hessinger RN. Spondylolysis and spondylolisthesis in children and adolescents. J Bone Joint Surg. 1989;14:1342-1355.
68 Elliot S, Hutson MA, Wastie ML, et al. Bone scintigraphy in the assessment of spondylolysis in patients attending a sports injury clinic. Clin Radiol. 1988;39:269-272.
69 Chou R, Huffman LH. American Pain Society, American College of Physicians. Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007;147(7):492-504.
70 O’Sullivan PB, Phyty GD, Twomey LT, et al. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine. 1997;22(24):2959-2967.