MUSCULOSKELETAL INJURIES
OVERUSE SYNDROMES
Carpal Tunnel Syndrome
Carpal tunnel syndrome is caused by elevated pressure in the “carpal tunnel,” which is a space at the base of the wrist through which pass nine tendons that flex (bend toward the palm) the fingers, along with the median nerve. It can be caused for a number of reasons, which include forceful, repetitive use of the wrist. The pressure causes the median nerve to have diminished function, which leads to the signs and symptoms. These include pain, numbness, tingling, and/or burning sensation on the palm side of the thumb, index finger, middle finger, and thumb side of the fourth finger. The “pinkie” side of the fourth finger and fifth finger are spared, as they are serviced by the ulnar nerve, which lies outside the carpal tunnel. Treatment is to avoid the offending activity and to splint the wrist in a “neutral” position of function (see page 73), both night and day if possible. A nonsteroidal antiinflammatory drug may be helpful. If the case is severe, a physician may prescribe oral steroids or inject steroids into the carpal tunnel. Medical evidence does not support the use of vitamin B6. If carpal tunnel syndrome persists and the victim shows loss of nerve function or muscle wasting at the base of the thumb, surgery may be advised to decrease the pressure.
Shin Splints
Shin splints is the term used to describe a painful disorder generated by excessive walking, running, or hiking. The sufferer has irritated the thin membrane that connects his two lower leg bones along the longitudinal axes where the membrane attaches to the bones. With every footstep, there is further irritation of the membrane, so that it can become impossible to walk rapidly. The victim should attempt to curtail running or vigorous walking activity, and may benefit from the administration of aspirin or a nonsteroidal antiinflammatory drug (such as ibuprofen or naproxen). A shoe that is well cushioned (particularly its ball and heel) is very important for prevention and recovery. More complex orthotics may be required.
Plantar Fasciitis
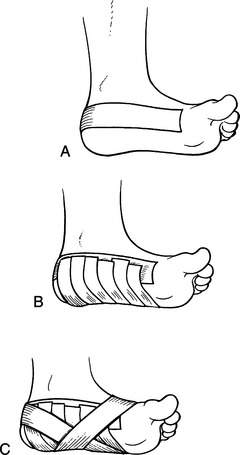
If the victim must continue to walk on the painful foot, it can be taped to provide arch support; this can do much to reduce pain. It is accomplished as follows: Apply a thin layer of benzoin or spray tape adhesive onto the bottom of the foot. Fix an anchor strip of ¾ in (1.9 cm) adhesive tape in a U shape around the heel from just under the malleoli (prominences of the ankle) up to just behind the level of the “knuckles” of the toes (Figure 169, A). Next, lay fairly tight cross-strips of ½ in (1.3 cm) tape across the bottom of the foot, with their ends torn to lay on the anchor strip (Figure 169, B). This creates a “sling” of tape under the foot for support. Finally, apply another U-shaped piece of tape around the heel that crosses under the center of the arch and locks down the crosspieces (Figure 169, C).
Torn Muscle
A torn muscle (“pulled” muscle) is recognized as sudden pain in a muscle group associated with a particular vigorous exertion, such as sprinting or lifting a heavy object. Depending on the severity of the injury, there may be associated bruising, swelling, loss of mobility, and/or weakness. For instance, a small tear in the deltoid muscle of the shoulder may cause minor discomfort on lifting the arm over the head, while a complete separation of the quadriceps group in the anterior thigh will cause inability to straighten the leg at the knee, extreme local pain, blue discoloration of the knee, and a defect in the shape of the muscles above the knee that is easily felt and seen.
Minor muscle injuries should be treated in the first 24 hours with immobilization, the application of cold (insulated ice packs or chemical cold packs, for example; do not apply ice directly to the skin) for 30 to 45 minutes every 2 to 3 hours, and elevation. After 48 to 72 hours, the application of heat (warm water or a heating pad, not ointments) and gentle movement should be started. If a significant injury is suspected (for example, complete tear of the biceps muscle or quadriceps muscle group), the injury should be immobilized as for a fracture (see page 74) and the victim transported to a physician.
Sprains and Strains
Sprains and strains are injuries to ligaments (which attach one bone to another) and tendons (which attach muscle to bone) that are incurred by twisting, direct blunt trauma, or overexertion. Symptoms include pain, swelling and/or deformity, decreased range of motion secondary to pain, and bruising. The treatment is the same as for a suspected fracture. The injured part should be elevated, immobilized (see page 74), and treated with cold applications for the first 24 to 48 hours (“RICE”: rest, ice, compression, and elevation). After 72 hours, heat may be applied. It is important to prevent reinjury (ankles are notorious) by proper wrapping or the application of a splint. Because the injured joint is immediately weakened, it should not be relied on for great exertion.
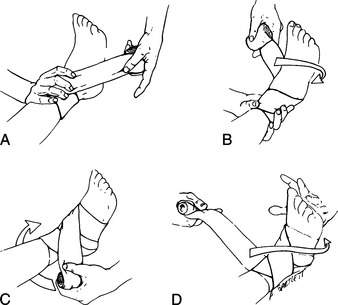
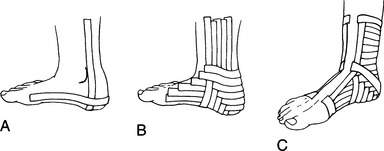
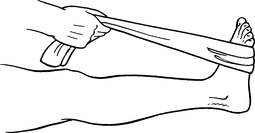
The most common sprain is of an ankle. If the injury is minor (no chance of a fracture) and/or if the victim needs to put weight on the ankle to seek help, the ankle may be wrapped snugly with an elastic wrap in a figure-of-eight method (Figure 170) or taped in a crisscross weave (Figure 171). During the wrapping or taping, have the victim point his toes and ankle upward by passing a slender rope or strap around the ball of the foot and pulling toward the body (Figure 172). This allows the ankle to be strapped with the foot perpendicular to the leg and the ankle ligaments in the shortened position in which they best heal. A splint can be fashioned from a SAM Splint (see Figures 91 and 92) to provide additional support. If the sprain is severe, splint the ankle as for a fracture. An Aircast Air-Stirrup ankle brace is excellent for in-shoe support.
The Achilles tendon, which runs from the heel into the lower calf, may become irritated or inflamed due to recurrent impact or repetitive stretching, particularly if the heel is not well padded. An inflamed Achilles tendon that is painful should be protected against further irritation by limiting vigorous exercise and using a heel cup or extra padding underneath the heel to reduce stretch forces on the tendon. Achilles tendon rupture is usually caused by a sudden forceful impact on the foot that is “flexed,” with toes pointed down, commonly during a jumping activity. There is pain and a sensation that something has torn or “popped.” The victim has difficulty walking and pushing down with the forefoot. A simple test that can detect a complete Achilles tendon rupture is to have the victim lie face down with the leg bent at the knee. Squeeze his calf and see if the foot moves in such a way that the toes point downward. If there is no motion (in comparison to the uninjured side), the tendon may be ruptured. For treatment, splint the foot and ankle with the toes pointed slightly downward, and try to eliminate weight bearing.
BURSITIS
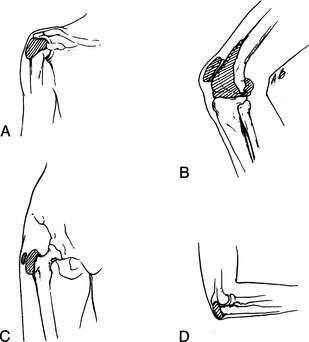
Bursitis is irritation and inflammation of the lubricating sac (bursa) that allows muscles to move freely around a joint. Common areas of irritation include the shoulder (irritated by arm swinging), the sac in front of the kneecap (irritated by prolonged kneeling), on the outside of the hip (irritated by walking, hiking, or falling), and behind the elbow (irritated by a fall) (Figure 173). Evaluation and treatment are the same as for arthritis.
VENOUS THROMBOSIS AND THROMBOPHLEBITIS
Thrombophlebitis is inflammation in a vein associated with the development of a blood clot (known as venous thrombosis: “DVT” means deep venous thrombosis). This occurs in conditions of injury to the veins (cuts, bruises), or after periods of prolonged rest in a single position (sitting on a plane, cramped in a cave); it may also be associated with other risk factors (genetic predisposition, pregnancy, tobacco use, cancer, varicose veins). A blood clot irritates the lining of the vein and causes local redness or purplish discoloration, swelling, warmth, and pain. If the clot enlarges, an entire limb length can become affected. These clots are most common in the lower leg, so the calf muscle may be tender to compression. If the clot is in a deep vein, it may break off and travel to the lungs, where it causes a serious condition known as pulmonary embolism (see page 46).
To avoid venous thrombosis: avoid prolonged periods of inactivity; get up and walk around once an hour when traveling on a plane, bus, or train; remain fit, active, and well hydrated; consider support hose if you have varicose veins or a history of blood clot formation in your legs or pelvis; and do not use tobacco products.
BACK PAIN
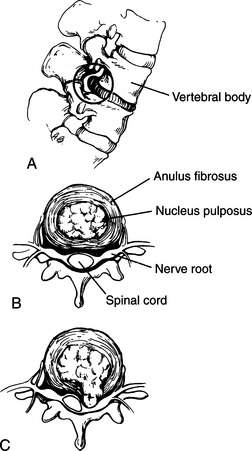
If one of the cushioning intervertebral (between the vertebrae) disks has been injured (Figure 174), additional symptoms may be noted, which include numbness and/or tingling of parts of the leg (indicating impingement of the disk on a nerve root arising from the spinal cord), shooting pains through the buttocks and posterior leg (indicating irritation of the sciatic nerve [sciatica]), leg weakness, foot drop, constipation, or difficulty with urination. The acute treatment is the same as for muscular back strain.
1. Proper size. It fits the torso closely, in particular the upper part of the body. When the padded waist strap is tightened, the weight of the pack should be distributed evenly across the hips.
2. The shoulder straps should be wide and well padded, to avoid compressing the front of the shoulders and armpits. They should be easily loosened and tightened. There should be a connecting strap that can be opened, closed, and adjusted traversing the front of the chest attached to and between the shoulder straps.
3. Adjustable straps to fine-tune the tightness of the waist strap and the proximity of the pack to the back of the wearer are desirable.
4. Multiple compartments allow rational storage, ease of finding carried items, and more even weight distribution than possible with a single-compartment pack. Side pockets, top pockets, tie-down loops, an adjustable top cover, and other features to partition objects into discrete locations while protecting them from the elements are all good to have.
5. The pack should be designed so that it can be donned from a sitting or standing position, using the legs for stabilization. If it can only be put on by hoisting it and slinging it across the back, muscle strain is inevitable.
6. For a child-carrier pack, be certain that it is designed so that an active child can’t easily self-extricate the pack and have it wind up dangling or on the ground.