chapter 15 Musculoskeletal Examination
Normal Musculoskeletal Variants
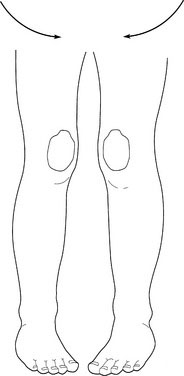
Internal femoral torsion (femoral anteversion)
When children have internal femoral torsion, the patellas show internal strabismus (Fig. 15–1). Gently rotate the knees so that the patella face forward. If internal femoral torsion is the problem, the feet suddenly and miraculously point directly forward.
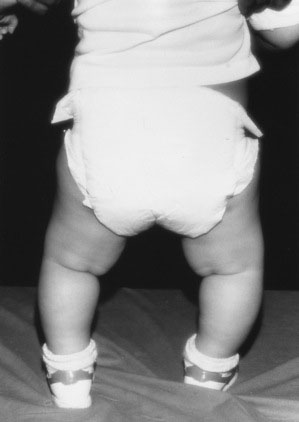
Bowleg (genu varum) and knock knees (genu valgum)
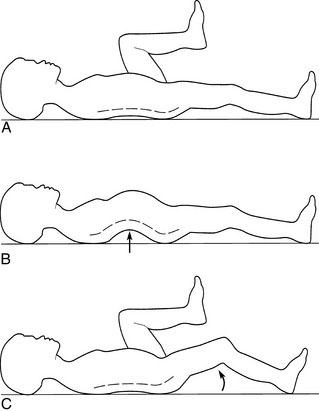
Mild lower extremity bowing is the norm in infants and young children (Fig. 15–2). Internal tibial torsion often accompanies physiologic bowing and accentuates the bowed appearance. No treatment is necessary. By age 2 years, physiologic bowing spontaneously corrects itself in most children. Many healthy children, including those who have had physiologic bowing as toddlers, gradually convert to develop some degree of genu valgum after age 2 years (Fig. 15–3), which usually disappears spontaneously by age 8 years.
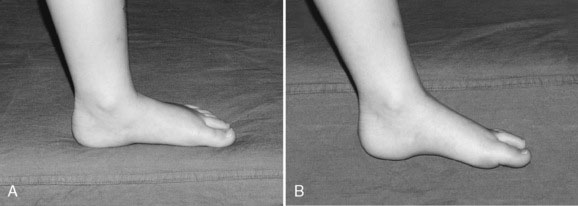
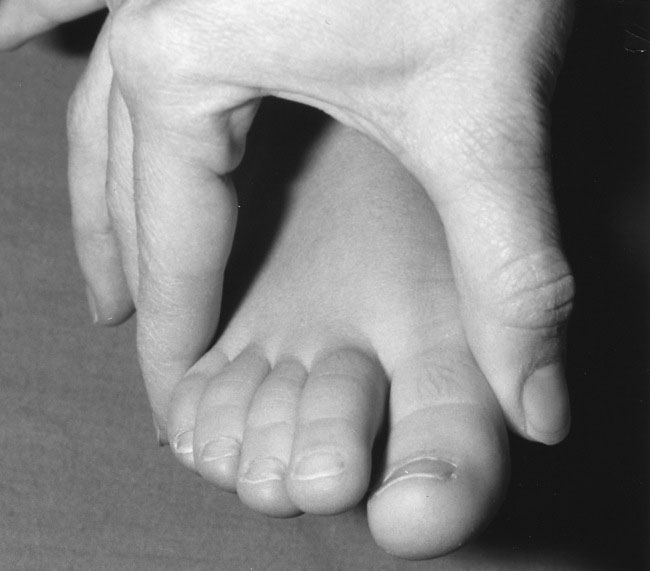
Metatarsus varus (forefoot adduction)
In metatarsus varus, the forefoot turns inward in relation to the long axis of the heel (Fig. 15–4). The critical clinical issue is to determine whether the foot deformity is fixed or flexible. Mild to moderate flexible metatarsus varus usually corrects itself, because it is the result of intrauterine position, or packing. A severe or fixed metatarsus varus may require serial casting or an orthotic device. If you are in doubt about the severity of this condition in a child, consult a pediatric orthopedist.
Flat feet
Flat feet are the norm in children younger than ages 2 to 3 years and in older children who show greater than average joint mobility. Usually asymptomatic, this normal variant is often simply part of generalized hypermobility. In such children, the normal body weight is sufficient to cause flattening of the feet. When the youngster sits on a table, the longitudinal arch miraculously reappears as the feet are suspended in space (Fig. 15–5).
Slipped Capital Femoral Epiphysis
Slipped capital femoral epiphysis occurs in adolescents. Presenting symptoms include:
Knee pain
Knee pain in children is often due to one of the following causes:
Back pain
Consider osteomyelitis of a vertebral body, discitis, or tumor in all children who present with back pain. Other causes are discussed here.
Generalized Causes of Musculoskeletal Pain
Tumors
Juvenile idiopathic arthritis
Arthritis is defined by the American College of Rheumatology as the presence of joint swelling or two or more of the following findings:
Benign hypermobility
Benign hypermobility syndrome is a common cause of joint pain, particularly in the knees, ankles, and fingers. Occasionally, the affected joints appear swollen for brief periods, but the swelling resolves spontaneously. The symptoms are episodic and may be exacerbated by exercise. The clinical findings that allow you to make a diagnosis of hypermobility are listed in Box 15–1.
The Child with a Limp
Causes of an abnormal gait may be divided into the following categories:
A limp is frequently accompanied by pain in a child, although discomfort may not be the chief complaint (Table 15–1). Recent pain accompanied by worsening symptoms suggests trauma, infection, slipped capital femoral epiphysis, or transient synovitis. The more prolonged the symptoms, the more likely that an abnormality will be detected on imaging studies. A limp that is worse in the morning and improves as the day progresses may be due to inflammatory disease. Limping without pain occurs in conditions such as developmental hip dysplasia, leg-length discrepancy, and neurological disorders.
| Cause | Underlying Conditions |
|---|---|
| Local causes | |
| Hip | Developmental hip dysplasia, |
| Legg-Calvé-Perthes disease (septic arthritis), transient synovitis, slipped capital femoral epiphysis | |
| Knee | Osgood-Schlatter disease, osteochondritis dissecans, tumors |
| Tibia | Toddler’s fracture, stress fracture, fracture through a bone cyst |
| Foot | Tarsal coalition, Köhler disease, tight shoes |
| Back | Spondylolisthesis, osteomyelitis, |
| Scheuermann disease | |
| Short leg | |
| Generalized disorders | |
|---|---|
| Bone diseases | Rickets, infections, leukemia, primary tumors |
| Muscle diseases | Inflammatory, congenital, metabolic myopathies |
| Joint diseases | Juvenile idiopathic arthritis, septic arthritis |
| Neurological diseases | Cerebral palsy |
| Psychiatric diseases | Conversion disorder |
The Child with a Single Swollen Joint
Six broad categories of monoarthritis are listed in Box 15–2. As with musculoskeletal pain, the location provides a diagnostic clue, particularly in rheumatic or orthopedic conditions.
The Child with Multiple Swollen Joints
The broad etiologic categories listed in Box 15–2 for a single swollen joint apply to determining the cause of multiple swollen joints in children, although mechanical and orthopedic conditions are less likely. Septic arthritis is also less likely, although not impossible, if multiple joints are affected. Certain infections usually affect more than one joint, including hepatitis B, Epstein-Barr virus, adenovirus, rubella, and Mycoplasma. Salmonella, Shigella, and Yersinia may cause postinfectious arthritis of multiple joints.
Significant Common Skeletal Deformities
By contrast, a history of torticollis noted shortly after birth suggests a congenital abnormality of the cervical spine (e.g., hemivertebra). Older children may demonstrate acute torticollis after an acute pharyngitis with cervical adenitis or after trauma. Associated symptoms may also suggest the etiology. Gastroesophageal reflux is occasionally associated with an intermittent torticollis, known as Sandifer syndrome. Ocular causes include a fourth cranial nerve palsy and, uncommonly, congenital nystagmus (see Chapter 8). Other uncommon causes are spinal cord or posterior fossa tumors, cervical spine infections, and JIA.
Obtaining the History
Even before beginning the detailed history, ask the child’s age because age and sex yield important clues to the cause of the musculoskeletal pain (Table 15–2). Establish the purpose of the visit and determine whether the parents
TABLE 15–2 Age Range and Sex Predominance for Common Musculoskeletal Disorders in Childhood
| Musculoskeletal Disorder | Peak Age Range (yr) | Sex Predominance |
|---|---|---|
| Trauma | Any age | Female and male |
| Infection | Any age* | Female and male |
| Malignancy | ||
| Osteoid osteoma | Any age (mostly 10-20) | Male > female |
| Primary malignant bone tumor | ≥10 | Female and male |
| Secondary bone tumor | Any age | Female and male |
| Juvenile idiopathic arthritis | ||
| Oligoarthritis | 1-3 | Female >> male |
| Polyarthritis RF-negative | 2-5 | Female > male |
| Polyarthritis RF-positive | >10 | Female >> male |
| Systemic | Any age | Female and male |
| Enthesitis-related arthritis | >8 | Male >> female |
| Psoriatic arthritis | 1-3 and >8 | Female > male |
| Transient synovitis | 4-8 | Male > female |
| Legg-Calvé-Perthes disease | 4-9 | Male > female |
| Slipped capital femoral epiphysis | 8-16 | Male > female |
| Osteochondritis dissecans | >10 | Male > female |
| Growing pains | 4-13 | Female and male |
| Fibromyalgia | >10 | Female >> male |
| Reflex sympathetic dystrophy | >10 | Female >> male |
RF, rheumatoid factor; >, greater than; >>, much greater than.
* Septic arthritis is most common in children aged 3 years or younger.
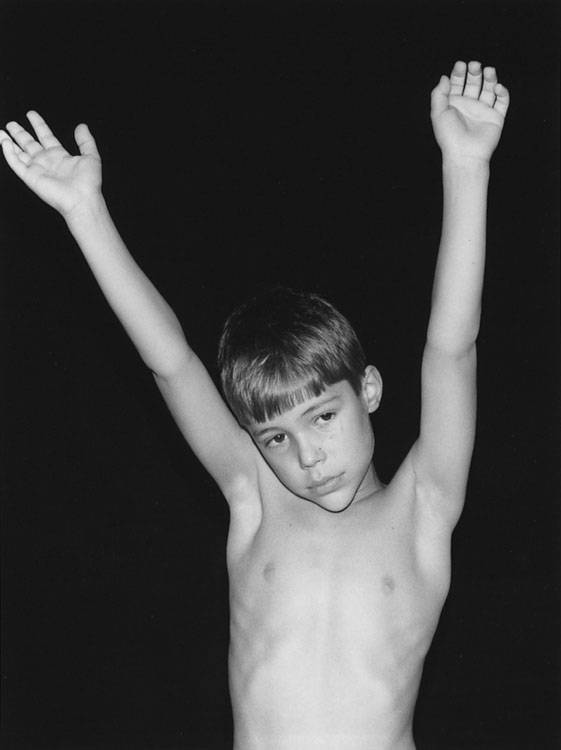
Approach to the Physical Examination
Observation
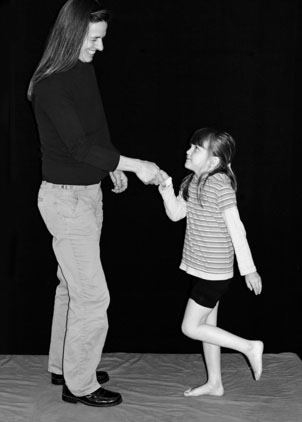
Watch the child closely. Observe for any obvious abnormalities while the child is walking or playing. If the youngster is old enough, begin the examination with nonthreatening activities that will help establish the extent of physical limitation. To detect subtle abnormalities in one limb, ask the child to hop on one foot at a time while you hold one of his or her hands. Note whether the child grasps your hand more firmly when supported on the affected leg (Fig. 15–6). Ask the youngster to walk on the heels and toes to determine whether there is impairment due to muscle weakness or due to local pain or tenderness. A simple screening technique to assess either strength or lower extremity joint disease is to ask the child to squat and walk across the room like a duck (Fig. 15–7). A normal “duck-walk” makes significant joint disease in the knees and hips extremely unlikely.

FIGURE 15–7 Squatting like a duck is a good screening test for weakness or other lower limb problems.
To test pelvic girdle muscle strength, ask the child to sit on the floor and then stand up; often with proximal muscle weakness, the child cannot rise from the floor without assistance or without either using a chair or table or climbing up the legs (placing the hands on the thighs to assist), a phenomenon (Fig. 15–8) known as the Gower maneuver.
Back examination
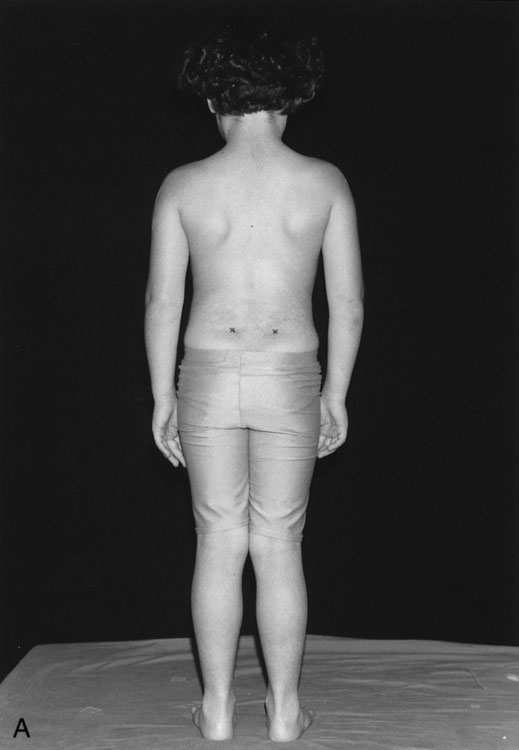
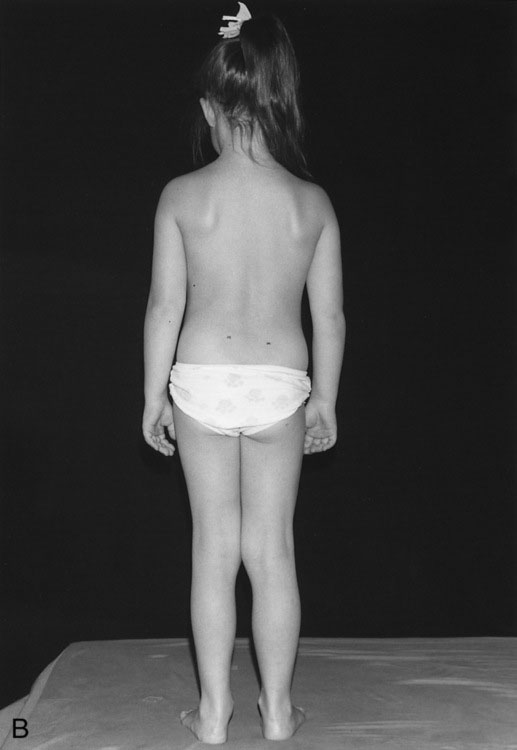
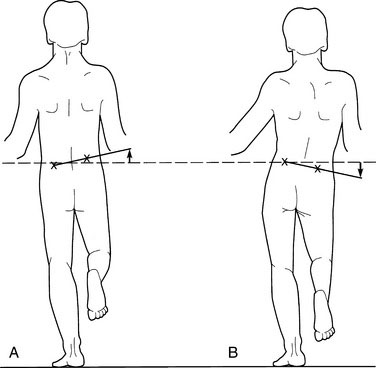
Look at the child from behind while the youngster stands upright. If the spinal dimples are level, there is no significant leg-length discrepancy (Fig. 15–9). Inspect the lower back for the presence of a tuft of hair, midline nevi, angioma, lipoma, or a central dimple, suggesting an underlying vertebral and spinal cord abnormality. If the spinal cord is tethered by a bony spicule or fibrous band (diastematomyelia), the child may present with back or lower extremity pain or may be asymptomatic for years.
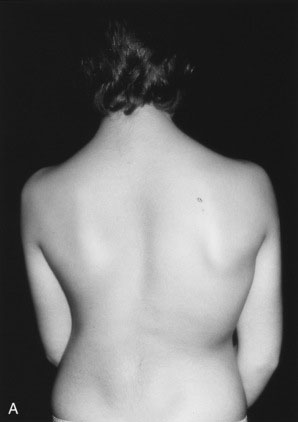
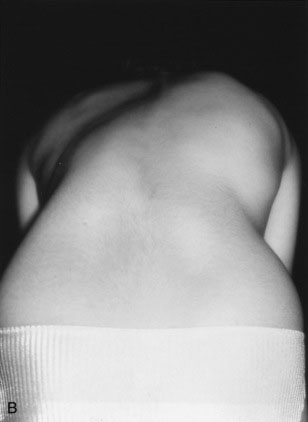
Next, with the child still standing, examine the back for scoliosis. Observed from behind, the shoulders should be level. Note any scapular prominence. With nonstructural scoliosis, a lateral curve is present that is flexible and is corrected with side bending to the convex side; with structural scoliosis, the curve is not corrected with side bending. A structural thoracic scoliosis leads to deformity of the rib cage, with the ribs on the convex side of the curve protruding on forward bending to produce a rib prominence on that side (Fig. 15–10). Ask the child to bend forward at the waist, keeping the knees straight and allowing the arms to hang down freely. This position accentuates even a slight rib or lumbar asymmetry. Inspect the back for compensatory secondary curves above and below the major curve. These secondary curves help keep the head aligned over the pelvis. If the child has a leg-length discrepancy, correct it before checking for scoliosis.
Have the child lie in a prone position, and palpate the spine, the paravertebral muscles, and the sacroiliac joints. Test back movement thoroughly in older children. Check lateral flexion by asking the child to tilt sideways without bending forward and to touch the tips of the fingers to just below the sides of the knees. Normally, the fingertips can touch the head of the fibula (Fig. 15–11). To test rotation, first have the patient straddle a chair to stabilize the pelvis and cross the arms across the chest to stabilize the shoulder girdle; then ask the patient to rotate the trunk (Fig. 15–12).
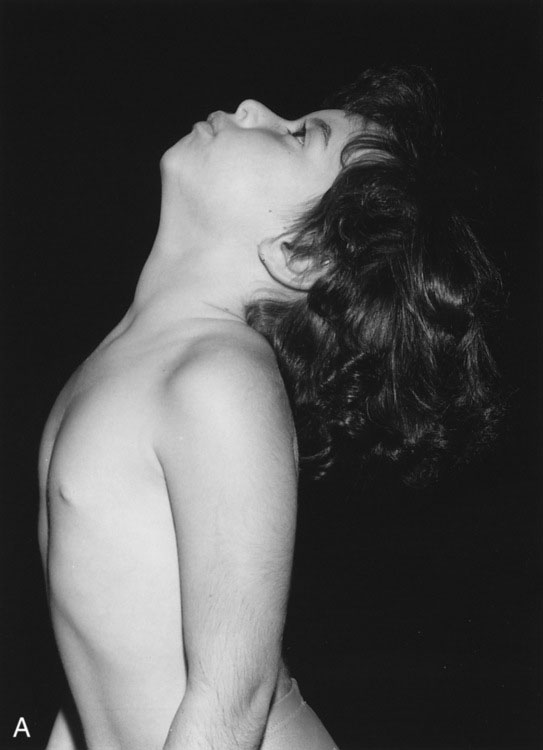
Cervical spine examination
Next, observe the cervical spine from the side, noting the presence or absence of the normal cervical lordosis. Palpate the paravertebral muscles and the spinous processes to detect tenderness or masses. Test the range of motion—extension, flexion, rotation, and lateral flexion. Normally, the cervical spine extends so that the child’s occiput touches the upper back, and the youngster looks directly at the ceiling (Fig. 15–13A). Loss of extension is often the most sensitive test for early cervical spine involvement in JIA (see Fig. 15–13B), whereas flexion may remain normal despite significant cervical disease. To test rotation, ask the child to look toward each shoulder; the normal range is 80° to 90°. Ask the child to touch each ear to the shoulder to test lateral flexion; the normal range is 45°.
Temporomandibular joint examination
Inspect the TM joint for overlying swelling just anterior to the tragus of the ear. Do not confuse this swelling with parotid gland swelling, which extends over the angle of the jaw behind and below the ear. Look for micrognathia. Mandibular growth may be impaired by arthritis affecting the TM joints in childhood (Fig. 15–14), and facial asymmetry may develop if one TM joint is more severely affected than the other.
Test jaw movement when the child opens the mouth widely. Because the jaw is smaller on the side of the more severely affected TM joint, the jaw shifts slightly toward the affected TM joint when the child opens the mouth wide. The interdental distance—the distance between the upper and lower central incisor teeth when the child opens the mouth maximally—is at least 3 cm in a normal child (Fig. 15–15). Palpate the mandibular condyles for tenderness, and try to appreciate their normal rounded contour, which may be lost with persistent arthritis. Crepitus may be present if the cartilage separating the condyle from the temporal bone is eroded.
Approach to the Examination of Specific Joints
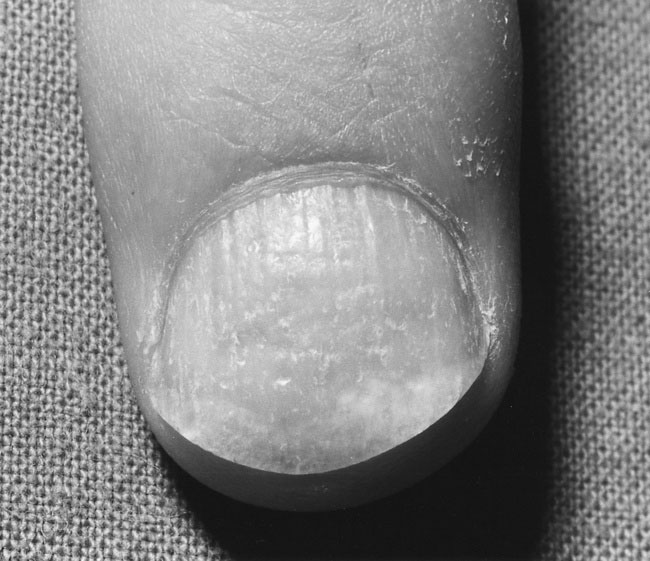
Hand examination
It is least threatening for a child if you begin the peripheral joint examination by inspecting the hands. Check the fingers for psoriatic nail pitting (Fig. 15–16), clubbing, periungual erythema, nail fold vasculitic infarcts (Fig. 15–17), loss of the distal finger pulp, ulcerated fingertips, and sclerodactyly. Note any swelling, redness, deformity, or asymmetry between the two hands (Fig. 15–18).

FIGURE 15–17 The dark spots on the nail bed represent small vasculitic infarcts, seen typically in connective tissue diseases.
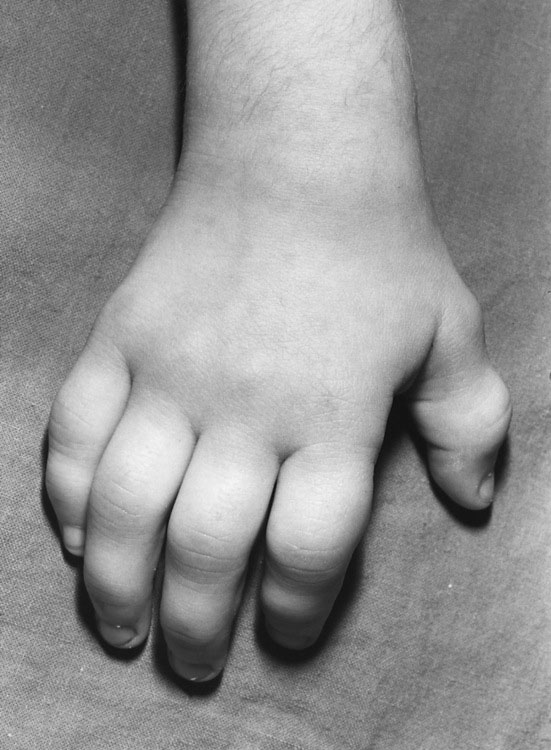
FIGURE 15–18 Marked swelling of the interphalangeal joints with flexion contractures in juvenile idiopathic arthritis.
Wrist examination
Inspect the wrist for deformity or malalignment. In JIA, ulnar posturing (deviation) of the wrist is not uncommon, and volar subluxation may occur with long-standing or severe disease. Examine the wrist for evidence of swelling along the joint line, which would indicate an effusion. Swelling may also be seen over the dorsum of the hand distal to the wrist joint (Fig. 15–19); its presence suggests tenosynovitis of the extensor tendon sheaths, which is confirmed if the swelling moves as the child opens and closes the fist. When the fingers are actively extended, the distal margin of the swelling moves proximally and appears to “tuck in”; hence, this phenomenon has been called the tuck sign (Fig. 15–20). Observe the range of motion at the wrist; in most children, flexion and extension to 80° to 90° are possible.
Shoulder examination
The shoulder mechanism consists of the glenohumeral joint and the shoulder girdle. The deltoid muscle produces the normal rounded contour of the shoulder, a contour that is lost with anterior shoulder dislocation or with significant muscle atrophy from primary muscle or joint disease (Fig. 15–21). Inspect the shoulder for normal contour and for an effusion, which results in an anterior prominence just lateral to the coracoid process.
Test mobility at the shoulder joint by asking the child to perform the following active movements:
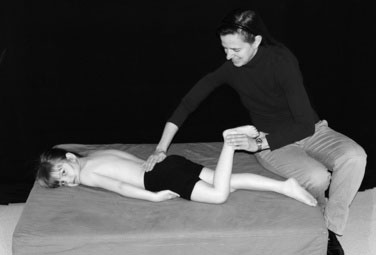
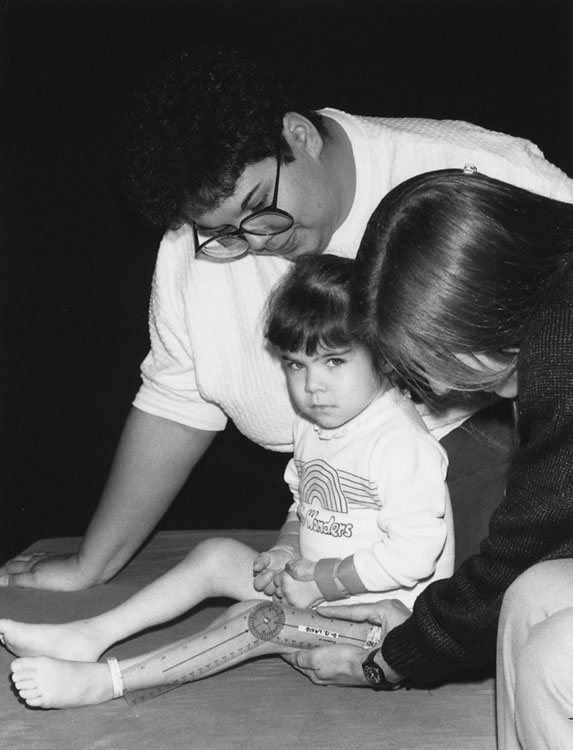
Hip examination
A screening test for hip disease in addition to the “duck-walk” test is the log roll, a painless test used to detect muscle spasm secondary to hip joint irritability. With the child lying supine, place your hand on the thigh and gently roll the hip into internal and external rotation, noting any resistance, which would suggest hip disease. To accurately assess the range of hip movement, you must place your other hand on the child’s pelvis to stabilize it (Fig. 15–23). When the pelvis moves, the end of hip movement has been reached. Normal hip mobility varies significantly with age and is generally greater in infants than in older children.

FIGURE 15–23 How to test hip abduction. Use one hand to stabilize the pelvis. Normal range is 40° to 50°.
It is best to examine hip rotation with the child lying prone and to symmetrically move the legs into external and internal rotation with the knees flexed, so that you can more easily appreciate pelvic movement, especially if you are an inexperienced examiner (Fig. 15–24). Flex the knee to 90°, move the foot outward to test internal rotation (normal range, 40° to 45°), and swing the foot inward to test external rotation (normal, 30° to 40°). The loss of internal rotation is often the first sign of hip involvement in children with joint inflammation. A valuable sign of hip disease is the external rotation of the hip as it is flexed from the extended position. The diminished abduction and internal rotation of the hip may be the earliest and sometimes the only abnormalities detected in the child with Legg-Calvé-Perthes disease or slipped capital femoral epiphysis.
Measure leg length from the anterior superior iliac spine to the medial malleolus, preferably with a steel tape (Fig. 15–25). It is important to position the patient supine with the legs fully extended and parallel and with the pelvis level.
A fixed flexion deformity of the hip may not be obvious on your initial observation of a child. Clues to a flexion contracture include an accentuated lumbar lordosis and a tendency to stand with one knee slightly bent despite the absence of knee disease. Perform the Thomas test, to detect a fixed flexion deformity, as follows (Fig. 15–26):
Use the Trendelenburg test to evaluate a painful hip or to gauge hip girdle weakness in the older child who will cooperate. Ask the child to stand on one leg; normally, the pelvis rises slightly on the side opposite to the leg one stands on because the hip abductors contract on the weight-bearing leg. When hip abductor muscles are weak, the pelvis drops downward on the side opposite to the weight-bearing (affected) leg (Fig. 15–27).
The Ortolani test is used specifically to detect the “clunk” of developmental hip dysplasia in the newborn (see Chapter 4). In an older infant or a child with untreated development hip dysplasia, the result is always negative because the dislocated femoral head can no longer be reduced into the acetabulum. Late diagnostic signs of developmental hip dysplasia are a painless limp, asymmetric posterior skin folds on the thighs, a shortened thigh (because the femoral head no longer remains in the acetabulum), and tightened muscles around the hip joint, which restrict hip movement, particularly abduction.
Knee examination
Inspect the knee for obvious swelling, redness, or evidence of injury. The first sign of a knee effusion is the loss of the normal concavity along the medial side of the patella. Check for the characteristic swelling over the tibial tuberosity seen in Osgood-Schlatter disease. Inspect the quadriceps muscle for wasting. Note any knee deformity. The most common knee deformity seen in children with JIA is a flexion contracture, which should be measured with a goniometer (Fig. 15–28). Bony overgrowth at the knee may occur with JIA because of epiphyseal overgrowth in the affected knee and may contribute to a leg-length discrepancy. Posterior subluxation of the tibia is demonstrable when the knee is bent to 90° and the proximal tibia sags posteriorly. This condition is an uncommon complication of JIA. Some children, including those with generalized ligamentous laxity, may have genu recurvatum (hyperextensible knees).
Evaluate patellar pain with the following additional tests:
Ankle and foot examination
Lateral compression of the metatarsals is a good screening test for inflammation of the metatarsophalangeal (MTP) joints. Perform this maneuver extremely gently because it can cause intense pain if one or more MTP joints are inflamed (Fig. 15–29). If the child complains of pain on compression, examine the MTP joints individually to identify the affected joint. Examine the toes for swelling or deformity. Diffuse swelling of a toe that gives it a sausage-like appearance, termed dactylitis, may occur with infection, psoriasis, and Reiter syndrome. Common toe deformities include hallux valgus, syndactyly (webbing deformity), polydactyly, and overlapping fifth toe.
Muscle assessment
You can make a more formal assessment of power performed by using a simple grading scale, shown in Table 15–3. Keep in mind, however, that there is considerable individual variability among both patients and examiners, and strength assessments that use this scale are estimations. Further description of the assessment of muscle power can be found in Chapter 13.
| Grade | Percentage of Function | Activity Level |
|---|---|---|
| 0—None | 0 | No evidence of muscle contractility |
| 1—Trace | 15 | Evidence of slight contractility; no effective joint motion |
| 2—Poor | 25 | Full range of motion without gravity |
| 3—Fair | 50 | Full range of motion against gravity |
| 4—Good | 75 | Complete range of motion against gravity with some resistance |
| 5—Normal | 100 | Complete range of motion against gravity with full resistance |
From Cassidy JT, Petty RE: Textbook of Pediatric Rheumatology, 4th ed. Philadelphia, WB Saunders, 2001.
Cassidy J.T., Petty R.E. Textbook of pediatric rheumatology. Philadelphia: WB Saunders, 2005.
Morrissey R.T. 6th ed. Lovell and Winter’s pediatric orthopedics. Philadelphia: Lippincott, 2005.
Stiell I.G., Greenberg G.H., McKnight R.D., et al. Decision rules for the use of radiography in acute ankle injuries: refinement and prospective validation. JAMA. 1993;269:1127-1132.